Introduction
Nasopharyngeal angiofibroma (NA) is a rare,
non-encapsulated and highly-vascularized benign tumor that
primarily affects adolescent males (1,2). Extremely
few studies have described NA in elderly individuals; in our
previous report of 162 cases from 1995 to 2012, all patients were
male subjects ranging in age from 8–41 years (mean, 17.5 years)
(3). Although NA is a benign neoplasm
histopathologically, it has a propensity for locally destructive
growth with bone erosion, which can lead to life threatening
complications, such as fatal epistaxis, and other complications,
including facial swelling, proptosis, cranial neuropathy, and
intraoperative massive hemorrhage (1,4). In the
majority of cases, patients present with symptoms of a painless,
unilateral nasal obstruction and epistaxis (4). Currently, surgery is the standard
treatment for NA (5).
The present study reports the case of a 72-year-old
male with NA that underwent a successful resection via an
endoscopic-assisted sublabial and buccolabial incision approach
(6). This case confirms the
occurrence of NA in the elderly, and also highlights the potential
of an endoscopic-assisted sublabial and buccolabial incision
approach for the treatment of NA in elderly patients.
Case report
A 72-year-old male presented with continuous
headaches, right nasal epistaxis, right nasal obstruction and a
decreased sense of smell for three months. The patient was admitted
to the First Affiliated Hospital of Medical School of Zhejiang
University (Hangzhou, China) on March 29, 2013, three months after
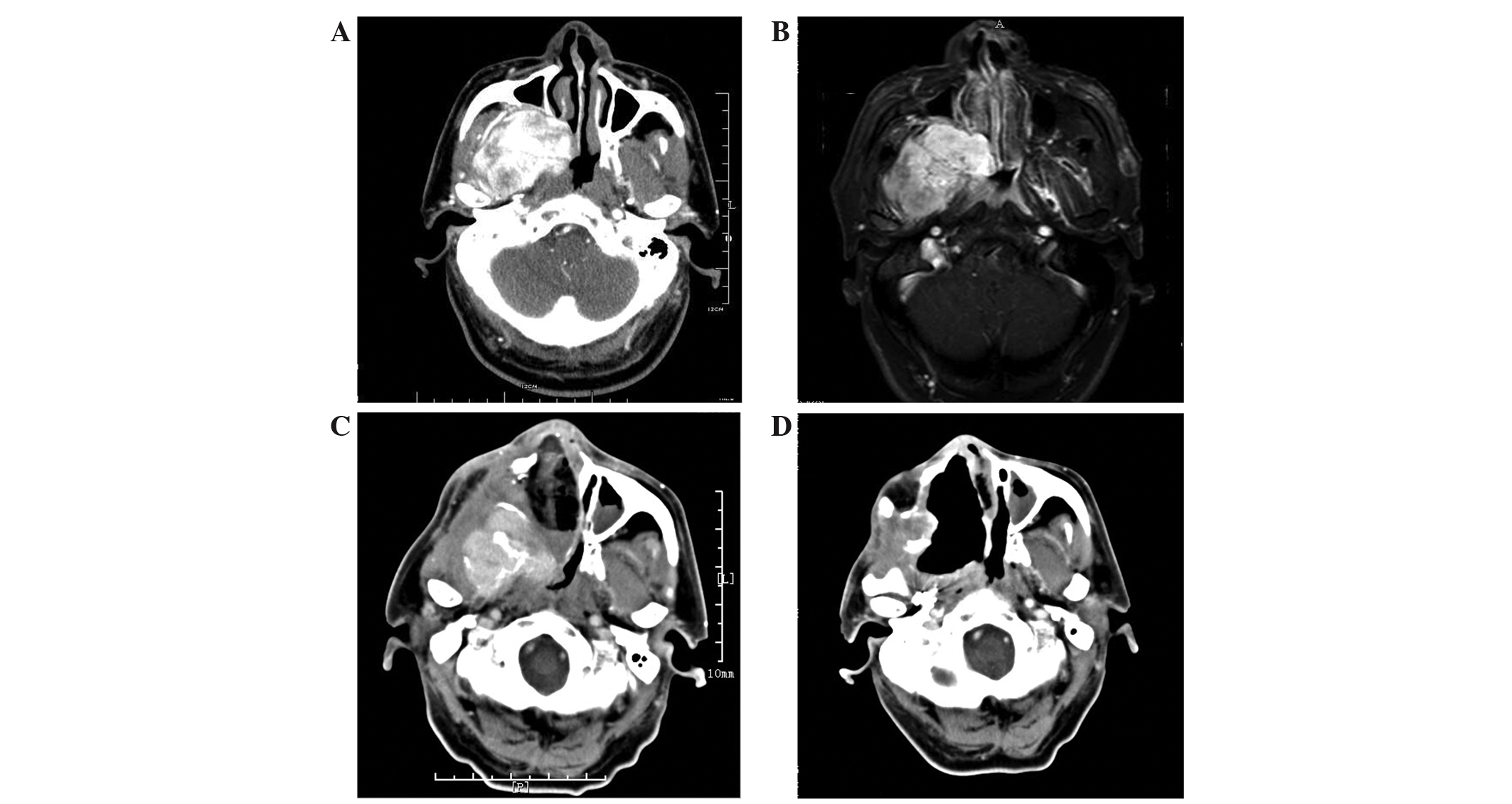
the initial onset of these symptoms. The contrast-enhanced computed
tomography (CT) and magnetic resonance imaging (MRI) revealed a
highly vascular nasopharyngeal mass, and the sphenomaxillary fossa
was enlarged (Fig. 1A and B).
Surgical resection was performed using a lateral rhinotomy
approach. However, due to massive hemorrhage, the tumor was not
completely removed. Histopathological examination of the excised
lesion revealed the presence of angiofibroma. Five months after
surgery, the patient presented with recurrent right spontaneous
epistaxis and right nasal obstruction and was subsequently referred
to the Fudan University Affiliated Eye, Ear, Nose and Throat
Hospital (Shanghai, China) to receive additional treatment.
A physical examination at our hospital revealed a
red mass in the right nasal cavity. Contrast-enhanced CT confirmed
the presence of a large soft-tissue nasal and nasopharyngeal mass
that extended into the right maxillary antrum and up towards the
orbital floor, with destruction of the medial and lateral walls of
the antrum, into the sphenoid sinus on the right side and continued
dorsally to the right parapharyngeal space and infratemporal fossa
(Fig. 1C).
An endoscopic-assisted sublabial and buccolabial
incision approach was used to remove the tumor following
pre-operative embolization. Using clamp forceps, the nasal
component of the tumor was pushed down into the nasopharynx and
drawn out through the oral cavity. In order to remove the
infratemporal fossa extension of the NA, a sublabial and
buccolabial incision, which extended from the first molar teeth to
the maxillary tuberosity at the gingivobuccal sulcus, was made on
the involved side. Due to the complex anatomy and high vascularity
of the region, a blood loss of ~2,800 ml occurred during the
surgery. The patient therefore received a blood transfusion of 400
ml fresh frozen plasma and 4 units of packed red blood cells. The
extensive hemorrhage also led to a poor surgical field. In order to
prevent accidental injury, the surgery was terminated without
further investigation. A contrast-enhanced CT scan was performed
the next day to determine whether the tumor had been completely
removed. The results revealed the presence of residual tumor in the
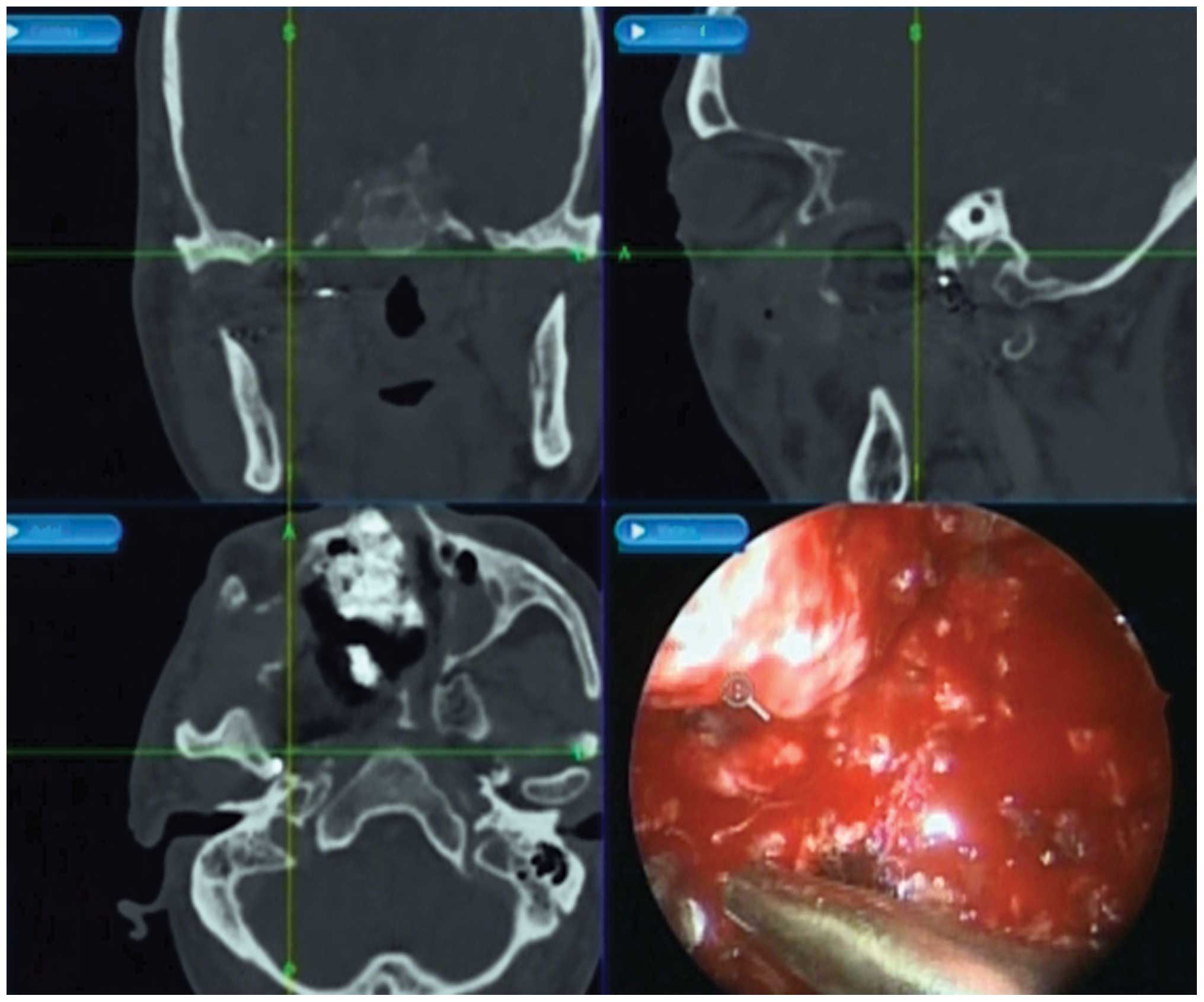
right parapharyngeal space and infratemporal fossa. A day later, a
repeat endoscopic-assisted sublabial and buccolabial incision
approach was performed to remove the residual tumor. An
image-guided navigation system (Medtronic, Louisville, KY, USA) was
used for the localization of the residual tumor in the right
parapharyngeal space and infratemporal fossa (Fig. 2). A contrast-enhanced CT scan
performed 2 weeks subsequent to the procedure confirmed the
complete removal of the tumor (Fig.
1D). The patient was followed up for 6 months, without
exhibiting evidence of recurrence.
A hematoxylin and eosin-stained section revealed
that the tumor was composed of a characteristic fibrous stroma in
which the vascular channels were lined by flat endothelial cells
(Fig. 3A). A Van-Gieson-stained
section established that the tumor was mainly composed of collagen
fibers, while elastic fibers were scarcely discernible (Fig. 3B). Immunohistochemically, the tumor
was positive for the expression of cluster of differentiation
(CD)31 (Fig. 3C), CD34 (Fig. 3D), CD68 (Fig. 3E), HHF35 (Fig. 3F), smooth muscle actin (Fig. 3G), and vimentin (Fig. 3H). The percentage of Ki-67-positive
cells was 4% (Fig. 3I). According to
these findings, a diagnosis of angiofibroma was established.
This study was approved by the Ethics Committee of
Fudan University Affiliated Eye, Ear, Nose and Throat Hospital, and
written informed consent was obtained from the patient and the
patient's family.
Discussion
In general, NA primarily affects adolescent males,
and is therefore considered to be a juvenile disease. However, NA
has been observed in at least three patients over the age of 70
(Table I), consisting of a
79-year-old male (7), a 71-year-old
female (8) and a 70-year-old male
(9). These patients were treated by
traditional open surgical approaches and the diagnoses were lacking
in immunohistochemical evidence. According to Patrocinio et
al (10), immunohistochemical
analyses are required for the diagnosis of atypical NA cases,
particularly those with atypical clinical manifestations. The
immune profile is extremely useful during the process of
pathological differential diagnosis.
 | Table I.Three patients over the age of 70
diagnosed with nasopharyngeal angiofibroma. |
Table I.
Three patients over the age of 70
diagnosed with nasopharyngeal angiofibroma.
| First author
(ref.) | Gender | Age, years | Surgical
approach |
|---|
| Conley et al
(7) | Male | 79 | Transpalatine or
lateral rhinotomy approach |
| Ewing and Shively
(8) | Female | 71 | Right lateral
rhinotomy and antrotomy |
| Shaheen (9) | Male | 70 | Moure's lateral
rhinotomy incision |
The present study reported a rare case of NA in a
72-year-old male, which was confirmed by histopathological and
immunohistochemical analysis. With the exception of age, the
patient demonstrated typical presentation, clinical examination and
radiological findings (Fig. 1).
Histologically and immunohistochemically, the tumor was composed of
proliferating vasculature in a fibrous stroma. The presence of
red-colored regions following Van-Gieson staining and a strong
positivity to vimentin indicated that the majority of the stromal
cells were fibrocytes (11). Positive
immunohistochemical staining for the endothelial markers CD31 and
CD34 supported true endothelial differentiation (Fig. 3) (12).
This typical presentation was of significant value for the
diagnosis of NA.
The etiology and pathogenesis of NA remains unclear.
It has been reported that no abnormalities in the serum levels of
dihydrotestosterone, testosterone and estradiol-17 B are detected
in NA patients (13). To a certain
extent, the occurrence of NA in the elderly may support the
hypothesis that serum androgen levels do not affect the development
of NA, since low serum androgen levels are present in older men
(14,15).
Large NAs continue to present a considerable
surgical challenge (1,6). The optimal treatment for these tumors is
gross total resection. However, open approaches require external
and internal incisions, which results in extensive soft-tissue
dissection and multiple osteotomies (3). Improvements in pre-operative assessment
and preparation, in addition to operative techniques and
instrumentation, may enable the endoscopic removal of the majority
of juvenile NAs (16). If the
location or extension of the tumor is too lateral or inferior to be
effectively resected by an endoscopic approach, a combination of
endoscopic and open approaches may be considered (17,18). It
has previously been reported that an endoscopic-assisted sublabial
and buccolabial incision is an optional approach for the removal of
an NA with extensive infratemporal fossa extension in youths
(6). The present case confirmed that
this modified surgery is well tolerated by the elderly. Due to a
firm connection with surrounding structures, the tumor may break
during surgery, leaving remnants in the surgical cavity, which
poses a challenge for effective treatment. As a result of tumor
extension and massive intraoperative hemorrhage, complete resection
of the tumor was unsuccessful following the first
endoscopic-assisted sublabial and buccolabial incision approach in
the current case. Therefore, a revision surgery was considered.
Image-guided navigation systems are useful for the localization of
deep located tumors (19). In the
present study, radiographical analysis revealed that the tumor had
been completely resected following image-guided surgery. This
counter example illustrated the value of the image-guided
navigation system.
The present study confirmed the occurrence of NA in
the elderly and highlighted the potential of an image-guided
endoscopic-assisted sublabial and buccolabial incision approach for
the treatment of NA in the elderly. In addition, the present study
established that image-guided navigation systems are useful for the
localization of deep NA lesions.
Acknowledgements
The authors would like to thank the patient for his
contribution to this work. This work was supported by the National
Natural Science Foundation of China (grant no. 81371077) and by
Shanghai Municipal Hospitals' Rising and Leading Technology Program
(grant no. SHDC12013121).
References
|
1
|
Sun XC, Wang DH, Yu HP, et al: Analysis of
risk factors associated with recurrence of nasopharyngeal
angiofibroma. J Otolaryngol Head Neck Surg. 39:56–61.
2010.PubMed/NCBI
|
|
2
|
Boghani Z, Husain Q, Kanumuri VV, et al:
Juvenile nasopharyngeal angiofibroma: A systematic review and
comparison of endoscopic, endoscopic-assisted and open resection in
1047 cases. Laryngoscope. 123:859–869. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Huang Y, Liu Z, Wang J, et al: Surgical
management of juvenile nasopharyngeal angiofibroma: Analysis of 162
cases from 1995 to 2012. Laryngoscope. 124:1942–1946. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tang IP, Shashinder S, Gopala Krishnan G
and Narayanan P: Juvenile nasopharyngeal angiofibroma in a tertiary
centre: Ten-year experience. Singapore Med J. 50:261–264.
2009.PubMed/NCBI
|
|
5
|
Paris J, Guelfucci B, Moulin G, et al:
Diagnosis and treatment of juvenile nasopharyngeal angiofibroma.
Eur Arch Otorhinolaryngol. 258:120–124. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sun XC, Li H, Liu ZF, et al:
Endoscopic-assisted sublabial and buccolabial incision approach for
juvenile nasopharyngeal angiofibroma with extensive infratemporal
fossa extension. Int J Pediatr Otorhinolaryngol. 76:1501–1506.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Conley J, Healey WV, Blaugrund SM and
Erzin KH: Nasopharyngeal angiofibroma in the juvenile. Surg Gynecol
Obstet. 126:825–837. 1968.PubMed/NCBI
|
|
8
|
Ewing JA and Shively EH: Angiofibroma: a
rare case in an elderly female. Otolaryngol Head Neck Surg.
89:602–603. 1981.PubMed/NCBI
|
|
9
|
Shaheen HB: Nasopharyngeal fibroma. J
Laryngol Otol. 45:259–264. 1930. View Article : Google Scholar
|
|
10
|
Patrocínio JA, Patrocínio LG, Borba BH, et
al: Nasopharyngeal angiofibroma in an elderly woman. Am J
Otolaryngol. 26:198–200. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bornemann A and Schmalbruch H:
Anti-vimentin staining in muscle pathology. Neuropathol Appl
Neurobiol. 19:414–419. 2009. View Article : Google Scholar
|
|
12
|
Pusztaszeri MP, Seelentag W and Bosman FT:
Immunohistochemical expression of endothelial markers CD31, CD34,
von Willebrand factor, and Fli-1 in normal human tissues. J
Histochem Cytochem. 54:385–395. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Farag MM, Ghanimah SE, Ragaie A and Saleem
TH: Hormonal receptors in juvenile nasopharyngeal angiofibroma.
Laryngoscope. 97:208–211. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ferrini RL and Barrett-Connor E: Sex
hormones and age: a cross-sectional study of testosterone and
estradiol and their bioavailable fractions in community-dwelling
men. Am J Epidemiol. 147:750–754. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Laughlin GA, Barrett-Connor E and
Bergstrom J: Low serum testosterone and mortality in older men. J
Clin Endocrinol Metab. 93:68–75. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Douglas R and Wormald PJ: Endoscopic
surgery for juvenile nasopharyngeal angiofibroma: Where are the
limits? Curr Opin Otolaryngol Head Neck Surg. 14:1–5. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Khalifa MA and Ragab SM: Endoscopic
assisted antral window approach for type III nasopharyngeal
angiofibroma with infratemporal fossa extension. Int J Pediatr
Otorhinolaryngol. 72:1855–1860. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gallia GL, Ramanathan M Jr, Blitz AM and
Reh DD: Expanded endonasal endoscopic approach for resection of a
juvenile nasopharyngeal angiofibroma with skull base involvement. J
Clin Neurosci. 17:1423–1427. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Farhadi M, Jalessi M, Sharifi G, et al:
Use of image guidance in endoscopic endonasal surgeries: A 5-year
experience. B-ENT. 7:277–282. 2011.PubMed/NCBI
|