Introduction
Breast cancer is the leading cause of
cancer-associated mortality among females worldwide, accounting for
~1.7 million cases and 521,900 mortalities in 2012 (1), and invasive ductal carcinoma is the most
common pathological type (1). The
relative five-year survival rate of invasive ductal carcinoma
ranges from 12% in parts of Africa to ~90% in the United States,
Australia and Canada (2). At Hubei
Cancer Hospital (Wuhan, China), the patients with breast cancer
often present with a painless mass in the breast and the most
commonly used examination method is mammary ultrasonography.
Currently, the therapeutic methods used for breast cancer include
surgery, chemotherapy, radiotherapy, endocrine therapy and targeted
therapy (3). Fibroadenomas are a type
of benign tumor that occur in younger women below the age of 35
years old. The tumors are the second most common type of tumor
after fibrocystic disease (4). The
chance of a carcinoma arising in a fibroadenoma is 0.1–0.3%
(5). Previous studies have reported
that fibroadenomas can evolve into different types of malignancy,
such as lobular intraepithelial neoplasia, lobular carcinoma in
situ, malignant phyllodes tumors and microinvasive lobular
carcinoma (4,6–9). However,
to the best of our knowledge, the present study is the first to
report a case of bilateral primary breast cancer with a unilateral
invasive ductal carcinoma within a fibroadenoma. Lumpectomy is the
most frequent treatment for fibroadenoma, with a good prognosis in
most cases (10–12). The current case of breast carcinoma
within a fibroadenoma is indeed a rare mammary tumor. Written
informed consent was obtained from the patient for the present
study.
Case report
A 48-year-old female presented with a 3.0-cm
palpable, well-circumstanced, rough, stiff lump in the upper outer
quadrant of the left breast, and a 2.0-cm palpable, smooth and
mobile lump in the upper inner quadrant of the right breast.
Clinical examination for other palpable masses in the breasts was
negative, and there was no axillary lymphadenopathy. Breast
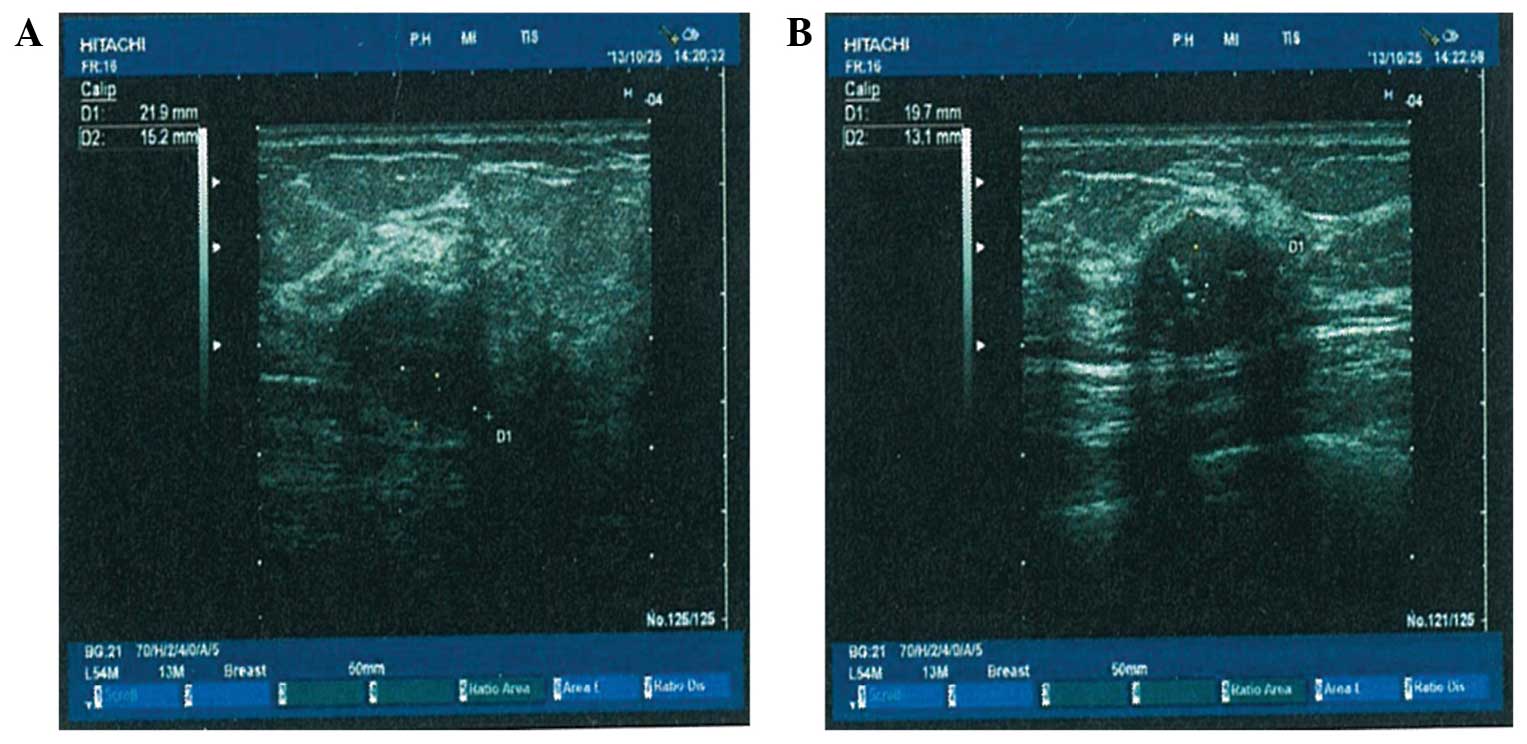
ultrasonography revealed a poorly-defined palpable solid lesion
(3.0 cm in diameter) in the left breast with the sonographic
features of a malignant tumor, and a well-defined solid lesion (2.0
cm in diameter) with the sonographic features of a hypoechoic mass
and calcification in the right breast (Fig. 1). The patient underwent surgery,
during which the lesions were removed, and the frozen tissue
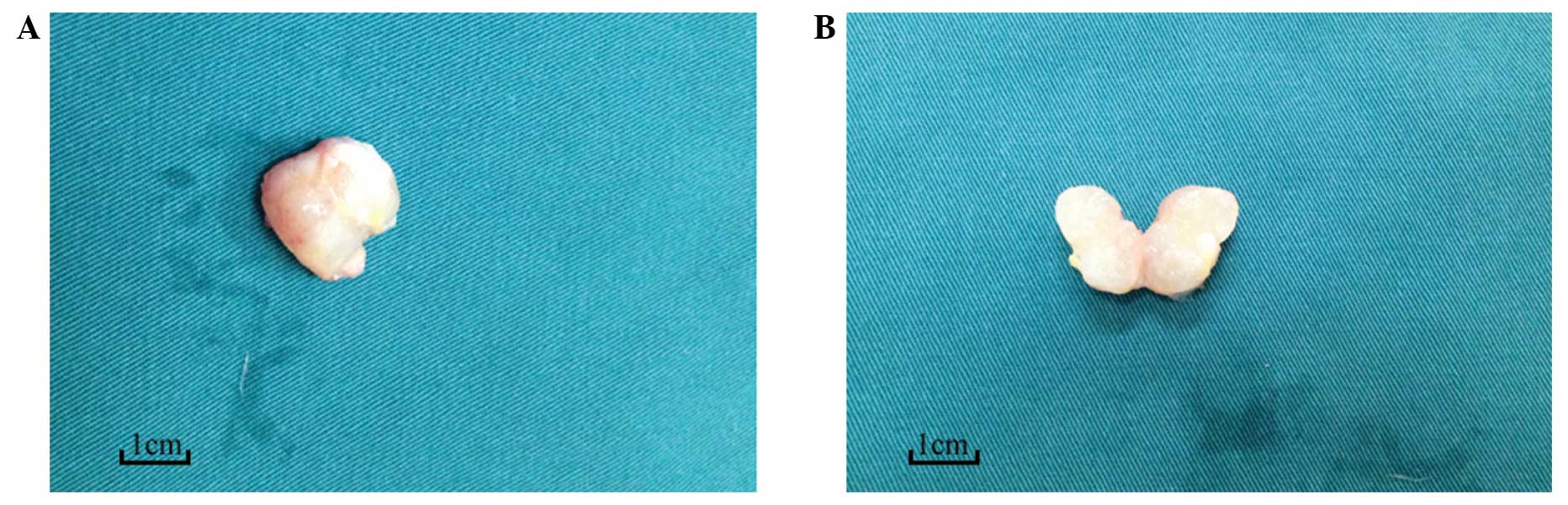
sections were pathologically examined. Gross examination of the
mass of the right breast revealed a smooth mass with a clear
capsule, with the traits of a benign tumor (Fig. 2). The intraoperative histopathology
revealed bilateral breast carcinoma; therefore, a bilateral
mastectomy was performed and the axillary lymph nodes of each side
were excised. The final pathological report revealed an invasive
2×3-cm2 lobular carcinoma of the left breast, without
metastasis to the axillary lymph nodes (0/14). According to the
American Society of Clinical Oncology/College of American
Pathologists Guideline Recommendations for Immunohistochemical
Testing (13,14), immunohistochemical assay of the tumor
in the left breast revealed the following: Estrogen receptor
(ER)(−), progesterone receptor (PR)(−), human epidermal growth
factor receptor 2 (HER2)(3+) and a Ki-67 labeling index (LI) of
60%. However, a 1.5×2-cm2 carcinoma was present within a
fibroadenoma on the right breast (mixed with invasive ductal
carcinoma, grade II, without metastasis to the axillary lymph
nodes) (0/16). Microscopically, the elements of fibroadenoma and
carcinoma could be observed in the pathological tissue slides
(Fig. 3). A second
immunohistochemical assay of the tumor in the right breast showed
the following: ER(+), PR(+), HER2(+) and a Ki-67 LI of 50%. The
patient received 4 cycles of chemotherapy (epirubicin, 60
mg/m2 and cyclophosphamide, 600 mg/m2) every
21 days and then following four cycles chemotherapy of docetaxel
(100 mg/m2) every 21 days. The patient then received
endocrine therapy (tamoxifen, 20 mg, twice daily) as maintenance
for 19 months. The patient had follow-up reviews once every 3
months, and has not exhibited any signs of recurrence up to the
latest follow-up appointment on May 10, 2015.
Discussion
Carcinoma arising within a fibroadenoma is a rare
and unique subtype of mammary cancer, which was reported by
Buzanowski-Konakry et al in 1975 (15). To date, <130 cases have been
reported in the literature (16–19).
According to the known diagnostic criteria, the
present case conforms to the diagnosis of sychronous bilateral
primary breast cancer. However, the case is particularly unusual,
as unilateral breast invasive ductal carcinoma arising within a
fibroadenoma also occurred. Compared with the cases reported in the
abovementioned literature that included carcinoma in situ
and invasive lobular carcinoma arising within a fibroadenoma
(9,15,16), the
current case presented invasive ductal carcinoma arising within a
fibroadenoma with contralateral invasive lobular carcinoma. To the
best of our knowledge, no such case has been reported previously in
the literature. In the present case, two mutually separated
cancerous nodes existed in the bilateral breast, and each possessed
different pathological traits. While the tumor on the left was an
invasive lobular carcinoma, the tumor on the right was a carcinoma
within a fibroadenoma mixed with invasive ductal carcinoma. Gross
examination revealed that the mass on the right possessed most of
the traits of a benign tumor, which was misdiagnosed as
fibroadenoma by a clinical doctor. Therefore, the breast masses
could not be identified by physical and gross examinations alone.
Further imaging tests and an excision were necessary to obtain a
clear diagnosis. The patient was administered routine therapy
regimens, which is the same treatment method as that used for the
other breast cancer patients. Few studies have reported the
prognosis of this type of breast cancer (20). The present patient has been closely
followed up for 19 months and has not exhibited any signs of
recurrence.
There are no rules guiding the therapy of a
carcinoma within a fibroadenoma. Thus, it is essential to
accumulate further case studies like the present study in order to
be able to treat such cases with evidence-based medicine.
Acknowledgements
The current study was supported by grants from the
Key Project of Health and Family Planning Commission of Hubei
Province, China (grant no. WJ2015MA016) and the Training Plan of
Young and Middle-Aged Backbone Talents of Medicine of Health and
Family Planning Commission of Wuhan, Hubei Province, China (March,
2014).
References
|
1
|
Torre LA, Bray F, Siegel RL, et al: Global
cancer statistics, 2012. CA Cancer J Clin. 65:87–108. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Youlden DR, Cramb SM, Dunn NA, et al: The
descriptive epidemiology of female breast cancer: An international
comparison of screening, incidence, survival and mortality. Cancer
Epidemiol. 36:237–248. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hurvitz SA, Hu Y, O'Brien N and Finn RS:
Current approaches and future directions in the treatment of
HER2-positive breast cancer. Cancer Treat Rev. 39:219–229. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Limite G, Esposito E, Sollazzo V, Ciancia
G, Formisano C, Di Micco R, De Rosa D and Forestieri P: Lobular
intraepithelial neoplasia arising within breast fibroadenoma. BMC
Res Notes. 6:2672013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Stafyla V, Kotsifopoulos N, Grigoriades K,
Kassaras G and Sakorafas GH: Lobular carcinoma in situ of the
breast within a fibroadenoma. A case report. Gynecol Oncol.
94:572–574. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ooe A, Takahara S, Sumiyoshi K, Yamamoto
H, Shiba E and Kawai J: Preoperative diagnosis of ductal carcinoma
in situ arising within a mammary fibroadenoma: A case report. Jpn J
Clin Oncol. 41:918–923. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hayes BD and Quinn CM: Microinvasive
lobular carcinoma arising in a fibroadenoma. Int J Surg Pathol.
21:419–421. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Monsefi N, Nikpour H, Safavi M,
Lashkarizadeh MR and Dabiri S: Mucinous subtype of invasive ductal
carcinoma arising within a fibroadenoma. Arch Iran Med. 16:366–368.
2013.PubMed/NCBI
|
|
9
|
Pacchiarotti A, Selman H, Gentile V,
Pacchiarotti A, Milazzo GN, Lanzilotti G, Lofino S and Frati P:
First case of transformation for breast fibroadenoma to high-grade
malignant phyllodes tumor in an in vitro fertilization patient:
Misdiagnosis of recurrence, treatment and review of the literature.
Eur Rev Med Pharmacol Sci. 17:2495–2498. 2013.PubMed/NCBI
|
|
10
|
Nio Y, Iguchi C, Tsuboi K and Maruyama R:
Ductal carcinoma in situ arising within a benign phyllodes
tumor: A case report with a review of the literature. Oncol Lett.
2:223–228. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Smith GE and Burrows P: Ultrasound
diagnosis of fibroadenoma-is biopsy always necessary? Clin Radiol.
63:511–515; discussion 516–517. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wilkinson S and Forrest AP: Fibro-adenoma
of the breast. Br J Surg. 72:838–840. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hammond ME, Hayes DF, Dowsett M, et al:
American Society of Clinical Oncology/College Of American
Pathologists guideline recommendations for immunohistochemical
testing of estrogen and progesterone receptors in breast cancer. J
Clin Oncol. 28:2784–2795. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lambein K, Van Bockstal M, Denys H and
Libbrecht L: 2013 update of the American Society of Clinical
Oncology/College of American Pathologists guideline for human
epidermal growth factor receptor 2 testing: Impact on
immunohistochemistry-negative breast cancers. J Clin Oncol.
32:1856–1857. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Buzanowski-Konakry K, Harrison EG Jr and
Payne WS: Lobular carcinoma arising in fibroadenoma of the breast.
Cancer. 35:450–456. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Diaz NM, Palmer JO and McDivitt RW:
Carcinoma arising within fibroadenomas of the breast. A
clinicopathologic study of 105 patients. Am J Clin Pathol.
95:614–622. 1991.PubMed/NCBI
|
|
17
|
Fukuda M, Nagao K, Nishimura R, Matsuda M,
Baba K, Ueno Y, Morinaga H, Omachi H and Hamada T: Carcinoma
arising in fibroadenoma of the breast-a case report and review of
the literature. Jpn J Surg. 19:593–596. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yoshida Y, Takaoka M and Fukumoto M:
Carcinoma arising in fibroadenoma: Case report and review of the
world literature. J Surg Oncol. 29:132–40. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tanaka A, Hirano M, Sakai Y, Ichikawa T,
Nitta N and Henmy K: Fibroadenoma, mastopathy, intraductal
papilloma: Relationship to carcinoma-a case report of carcinoma of
the breast arising in fibroadenoma. Nihon Geka Hokan. 52:232–243.
1983.(In Japanese). PubMed/NCBI
|
|
20
|
Gashi-Luci LH, Limani RA and Kurshumliu
FI: Invasive ductal carcinoma within fibroadenoma: A case report.
Cases J. 2:1742009. View Article : Google Scholar : PubMed/NCBI
|