Introduction
Primary carcinomas of ectopic breast tissue have
been reported in only a small number of cases and the axilla was
the most frequent site of the primary tumor (1). Evans et al (2) reported that 71% of ectopic breast
cancers were located in the axilla. Marshall et al (3) reported that 58% occurred in the axilla,
18.5% in the parasternal, 8.6% in the subclavicular, 8.6% in the
submammary, and 4% in the vulvar; 94.7% of patients were women, and
only 5.3% were men. Breast tissues develop from the ectodermal
ridges, also known as the milk lines, on the ventral surface of the
body, which extend from the axillae to the inguinal regions and end
on the medial aspect of the thighs on each side of the body
(4). Embryologically, ectopic breast
tissue develops as a result of failed resolution of the mammary
ridge, an ectodermal thickening that extends from the axilla to the
groin (5). Ectopic breast tissue may
appear at any site along the milk line, but it occurs most commonly
in the axill; less commonly, it may appear in locations outside of
the mammary ridge, including the face, middle back, buttock,
posterior neck, chest, vulva, hip, posterior, flank and/or lateral
thigh, shoulder and upper extremities (4,6).
The diagnostic procedures and therapeutic management
of accessory breast carcinoma are not definitively established. The
present study aimed to perform an analysis of a series of patients
with accessory breast cancer that were treated exclusively with
combination chemotherapy and radiotherapy, as well as to review the
medical literature with regard to the clinical features, treatment
methods and prognosis of this disease. The present study reports 11
such cases, with the goal of contributing valuable information
about this unusual tumour to the current literature.
Materials and methods
Patients
The records of 11 patients treated for accessory
breast cancer between January 2002 and June 2014 at Shandong Cancer
Hospital and Institute (Jinan, Shandong, China) were
retrospectively evaluated. The diagnosis for all patients was
histologically confirmed by biopsies. All clinical data were
obtained by reviewing the patients' medical records and
communicating with the identified patients through telephone
conversations and outpatient follow-up visits prior to June 2014.
The follow-up period was defined as the duration between the date
of the definitive diagnosis and the final visit. Written consent
was obtained from all patients and the study was approved by the
Ethics Committee of Shandong Cancer Hopsital and Institute.
Clinical features
Out of the 11 patients, 5 initially noticed a small
subcutaneous nodule in the left axillary area, while the other 6
initially noticed a nodule in the right axillary area. In addition,
8 patients (72.8%) were premenopausal, and 3 patients (27.2%) were
post-menopausal. The duration of disease was 3–24 months, with a
median time of 12 months. The tumour size, as determined by
ultrasound, computed tomography (CT) or magnetic resonance imaging
(MRI), ranged between 0.5×1.0 and 5.0×6.0 cm. The tumours were
immobile and solid with irregular boundaries. Also, 1 patient
presented with enlarged ipsilateral axillary lymph nodes and 7
patients presented with the complaint of a painful tumour that was
localised in the axilla.
Pre-operative examination
In total, 10 patients had undergone mammography, and
4 of these patients had no mammogram-detectable abnormalities. In
the remaining patients, mammograms identified left breast lesions
considered to be cancer in 3 patients and right breast cancer
lesions considered to be cancer in another 3 patients. Breast and
axillary ultrasonography was performed in 9 patients, which
identified enlarged right axillary lymph nodes in 3 patients, right
axillary accessory breast tumours in 3 patients, left axillary
accessory breast tumours with axillary lymph node enlargement in 2
patients, and extremely hypoechoic nodules of the left breast with
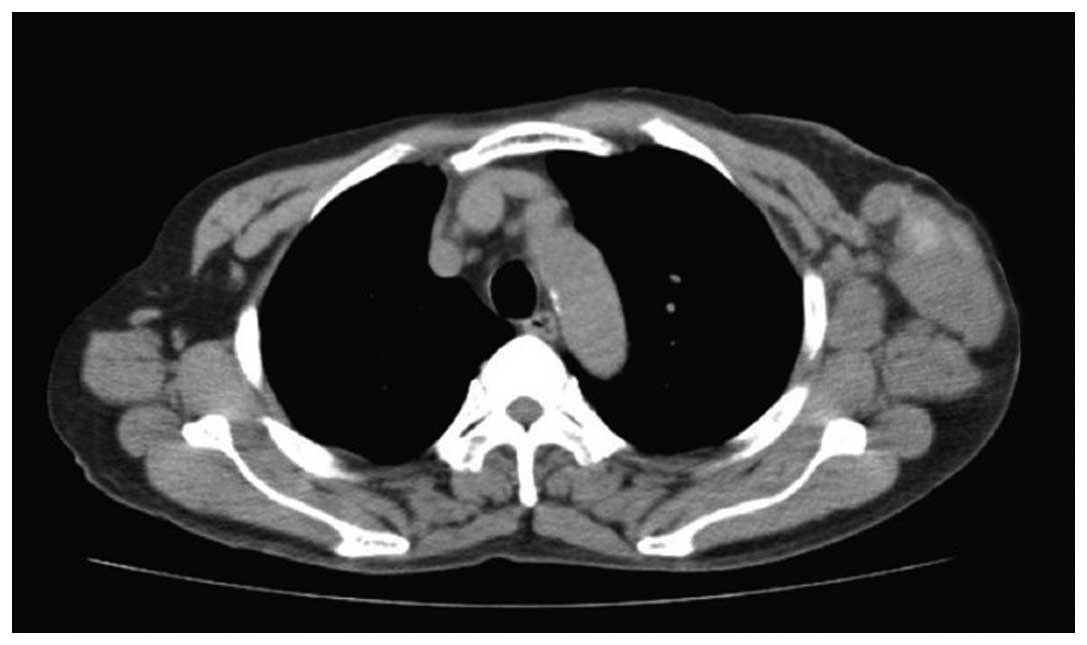
left axillary hypoechoic nodules in 1 patient. CT scans were
performed on 6 patients (Fig. 1),
with 2 patients demonstrating post-operative breast changes, 2
patients possessing right breast nodules, and 2 patients being
considered to possess right occult breast cancer with right
axillary lymph node metastasis. MRI examinations were performed on
4 patients, with 1 patient exhibiting post-operative breast
changes, 2 patients demonstrating left axillary lymph node
enlargement, and 1 patient being considered to possess a right
accessory breast tumour. In 2 patients, positron emission
tomography (PET)/CT demonstrated no evidence of any malignant or
occult primary lesions except for the axillary tumour. Axillary
tumour excision biopsy was performed in 3 patients, and
pathological examination confirmed the diagnosis of accessory
breast cancer. Axillary mass fine needle aspiration biopsies were
performed on 8 patients, and cytological examination revealed
cancer cells in all these patients.
Admitting diagnosis
According to the clinical and imaging features, 8
patients were preliminarily diagnosed with accessory breast cancer,
2 patients with breast cancer and 1 patient with ipsilateral
axillary breast cancer recurrence.
Statistical analysis
SPSS 15.0 statistical software (SPSS Inc., Chicago,
IL, USA) was used to compare the overall survival time, as
calculated from the date of surgery, using the χ2 test.
P<0.05 was considered to indicate statistical significance.
Results
Patients
A summary of the clinical and laboratory data of the
11 patients with accessory breast carcinoma is presented in
Tables I and II. All 11 patients were female, and the
patient ages ranged between 27 and 48 years, with a median age of
38 years. The patients were followed up for a period ranging
between 4 months and 4 years, 6 months. The median follow-up time
was 20 months.
 | Table I.Patient and disease characteristics,
treatment in accessory breast carcinoma. |
Table I.
Patient and disease characteristics,
treatment in accessory breast carcinoma.
| Patient | Age, years | Gender | Disease sites | Histopathology | Stage | Primary
treatment | Follow-up,
months | Metastasis |
|---|
| 1 | 45 | Female | Left axilla | ILC | I | CAF | 40 | No |
| 2 | 48 | Female | Right axilla | ILC | I | CEF | 54 | No |
| 3 | 30 | Female | Right axilla | IDC | II | CEF | 37 | Liver |
| 4 | 27 | Female | Left axilla | IDC | II | CAF | 10 | No |
| 5 | 42 | Female | Left axilla | IDC | III | CAF | 13 | Axillary lymph
node |
| 6 | 38 | Female | Right axilla | IDC | III | AC-T | 4 | No |
| 7 | 35 | Female | Left axilla | IDC | III | CAF | 36 | Liver, bone |
| 8 | 48 | Female | Left axilla | ILC | II | CAF-T | 37 | No |
| 9 | 28 | Female | Right axilla | IDC | II | EC-T | 20 | No |
| 10 | 46 | Female | Right axilla | IDC | IV | CAF | 5 | Liver |
| 11 | 32 | Female | Right axilla | IDC | III | CAF | 16 | Brain |
 | Table II.Clinical characteristics and
laboratory examinations of accessory breast carcinoma (n=11). |
Table II.
Clinical characteristics and
laboratory examinations of accessory breast carcinoma (n=11).
| Characteristic | Incidence, % |
|---|
| Systemic
symptoms |
|
|
Fever | 36.3 |
|
Weak | 54.5 |
| Weight
loss | 45.4 |
|
Mass | 100 |
| Nipple
discharge | 27.2 |
|
Edema | 45.4 |
| Receptor
expression | 11 |
|
ER(+) | 81.8 |
|
PR(+) | 63.6 |
|
HER2(+) | 63.6 |
The patients exhibited systemic symptoms including
fever, weight loss, night sweats, weakness, hepatosplenomegaly and
lower limb oedema. Of the 11 reported patients, routine blood
chemistry analyses included haematic cell analysis, electrolyte
levels, liver function studies and haemograms, which revealed no
abnormalities.
Perioperative management
Surgery was performed by a team of breast surgeons.
The responsibilities and tasks of each surgeon were clearly defined
prior to surgery. The breast surgeon was responsible for the
ablative procedure, including tumour resection and sentinel node
biopsy. Wide local excision with the removal of adjacent lymph
nodes was the treatment of choice, and the breast was only removed
if any suspicious nodules were palpable within the breast tissue.
If a contralateral procedure was required, the procedure was
performed simultaneously with the ablative procedures to minimise
time in the operating theatre.
Treatment
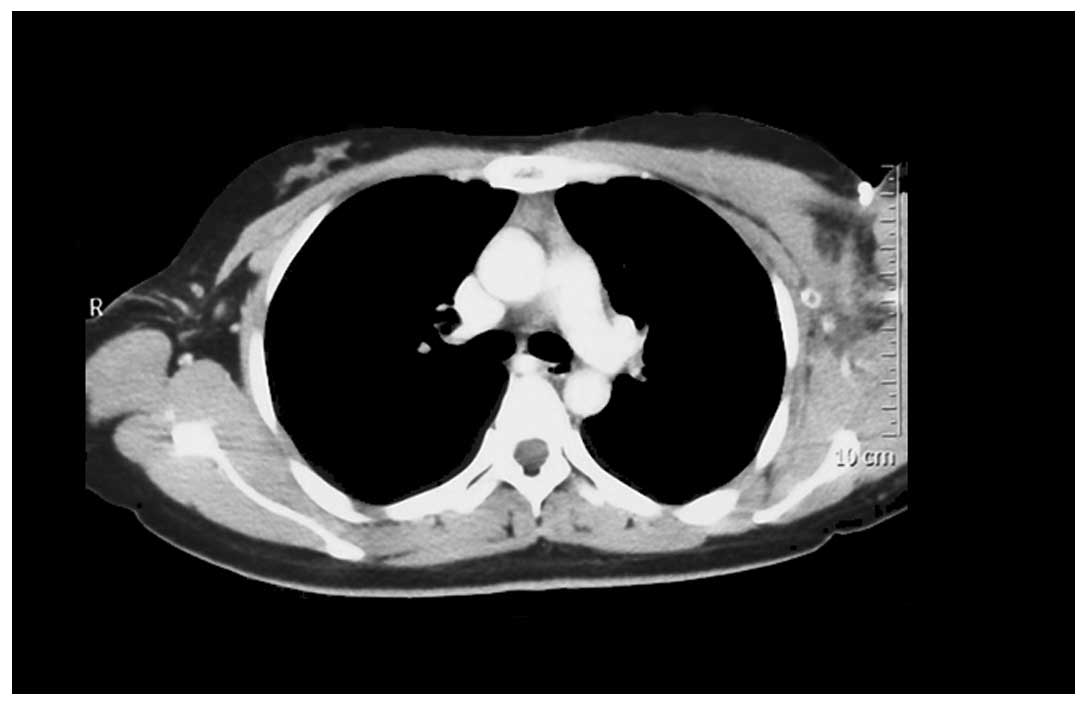
Modified radical mastectomies were performed on 2
patients, and enlarged accessory breast resections and axillary
lymph node dissection were performed on 6 patients (Fig. 2). The surgical specimen consisted of
the post-excision skin, subcutaneous tissue and a portion of the
thoracic wall. For 3 patients, the axillary tumour was regarded as
locally advanced accessory breast cancer that was challenging to
resect completely, and neoadjuvant chemotherapy was planned.
The resected tissue was frozen and examined
pathologically to ensure tumour-free margins. The specimen was
subsequently evaluated by routine histological methods. In order to
avoid contamination, the surgical fields were kept strictly
separated in cancer and non-cancer regions, including the use of
separate instruments.
Post-operative treatment
All patients underwent 2–8 courses of chemotherapy
following surgery. On average, six chemotherapy courses were
administered (Table I). In total, 6
patients (54.5%) were treated with the cyclophosphamide,
doxorubicin and fluorouracil regimen, 2 patients (18.1%) were
treated with the cyclophosphamide, epirubicin and fluorouracil
regimen, 1 patient (9.1%) received the doxorubicin,
cyclophosphamide and paclitaxel regimen, 1 patient (9.1%) received
the epirubicin, cyclophosphamide and paclitaxel regimen, and 1
patient (9.1%) was treated with the cyclophosphamide, doxorubicin,
fluorouracil and paclitaxel regimen. In addition, 3 patients
received post-operative radiotherapy at a dose of 6,000 cGy.
Following chemotherapy, 5 patients began treatment with hormone
therapy, consisting of 20 mg/day tamoxifen.
Pathological and immunohistochemical
characteristics
Histological evaluation identified 8 cases (72.7%)
of invasive ductal carcinoma and 3 cases (27.2%) of invasive
lobular carcinoma. Pathological staging, which was performed
according to the American Joint Committee on Cancer staging of
breast cancer, revealed 2 patients with stage I disease, 4 patients
with stage II disease, 4 patients with stage III disease and 1
patient with stage IV disease. Metastasis was identified in the
axillary lymph nodes of 5 patients, who possessed 6, 11, 14, 23 and
24 involved lymph nodes, respectively. In all cases, the oestrogen
receptor (ER) and progesterone receptor (PR) status was determined,
which revealed 9 of these tissues to be positive for ER and 7 for
PR. Human epidermal growth factor receptor type 2 (HER2) status was
also determined in all cases, and 4 patients did not express HER2.
The proliferation factor Ki67 was measured in 4 cases, all of which
were expressed Ki67.
Outcome
In 7 of the reported cases (64%), a local relapse or
metastasis of the neoplasm occurred following excision (Table I). In total, 2 patients experienced
recurrence and had succumbed to accessory breast cancer, with 1
patient succumbing at 20 months and the other at 40 months. Also, 1
stage III patient experienced axillary lymph node metastasis within
1 year following surgery, 1 stage III patient experienced brain
metastasis within 1 year following surgery and another stage III
patient experienced extensive tumour metastasis within 2 years of
surgery. In addition, 1 stage II patient experienced liver
recurrence ~2 years following surgery and one stage IV patient
experienced liver recurrence within 4 months of tumour excision.
The 2-year actuarial distant metastases rate was 36.4% (4/11). Out
of the 5 patients that experienced metastasis, 4 patients succumbed
subsequent to the initial diagnosis due to distant metastases. The
other patient was alive with the disease at the end of follow-up.
The remaining 4 patients were all alive at the end of follow-up.
Patient survival duration ranged between 5 and 54 months, with a
median survival time of 20 months. The three-year overall survival
rate was 54.5% (6/11).
Discussion
Breast tissue generally develops along the embryonic
mammary ridge, also termed the milk line, which extends from the
axilla to the groin area and appears in the sixth week of gestation
(6,7).
The milk line normally disappears, with the exception of the
mammary ridge of the thoracic region, where normal breast tissue
develops. However, accessory mammary tissue may develop due to an
incomplete embryological regression of the mammary ridge, which is
composed of a portion of the galactic band that runs from the
axilla to the groin (5). The presence
of accessory breast tissue is uncommon, with an overall incidence
range of 0.22 to 6.00% in the general population (8,9). Women are
reported to exhibit a increased incidence of accessory breast
tissue compared with men. The most common location of ectopic
breast tissue is the axilla. Other less common locations are the
face, thighs, perineum, groin, vulva and shoulders (10,11).
Ectopic breast tissue may consist of the breast parenchyma, areola,
nipple or any combination of these three components (12). This breast tissue is subject to
hormonal influences and undergoes physiological changes (13). In addition, a number of different
neoplasms, benign and malignant, have been found in axillary breast
tissue (14). The most common of
these tumours reported in the literature is the fibroadenoma, and
there are scattered case reports of other tumours, including
phyllodes tumour and mammary carcinoma (14).
Accessory mammary carcinoma is extremely rare,
constituting 0.3–0.6% of all breast cancer cases, generally
occurring as an axillary tumour (15). Primary breast carcinoma arising in
accessory breast tissue of the axilla is the most common clinical
presentation, comprising 60–70% of all ectopic breast tumours
(16,17). The most common pathology of accessary
breast tissue carcinoma, as with normal breast carcinoma, is
invasive ductal carcinoma (18). The
most common physical manifestation of this carcinoma is a palpable
mass. Oedema, tenderness, breast pain and non-specific discomfort
are observed less often (19).
Diagnostic procedures and therapeutic management of
patients with accessory breast cancer are not unequivocally
established (20). The diagnosis of
accessory breast cancer is not always considered and is, therefore,
often delayed (21). Generally, a
diagnosis of accessory breast cancer requires a pathological
demonstration of cancerous tissue adjacent to normal breast ducts
or lobules that are not connected to the proper mammary gland. It
is also necessary to exclude the possibility of a metastatic lesion
from another primary cancer (18). An
accurate diagnosis of axillary accessory breast carcinoma is
important, as it can provide precise staging information for
patients with concurrent ipsilateral breast cancer (7). However, this diagnosis can be extremely
challenging, if not impossible, since primary breast cancer
frequently extends to the axillary tail and metastatic carcinoma
may completely replace the involved lymph nodes (19). The differential diagnosis must include
other subcutaneous masses, such as fibroadenomas, lipomas,
hidradenitis and follicular cysts, as well as lymphadenopathy
associated with benign or malignant disease, since aberrant breast
tissue is most commonly found in the axilla (22). Therefore, axillary tail breast cancer,
axillary lymph node tumour metastasis, occult breast cancer and
lymphoma must be excluded prior to a firmly established diagnosis
of accessory breast cancer (22).
In the current study, systemic examinations,
including CT, MRI, ultrasonography and positron emission
tomography/CT, revealed no primary malignant or occult lesions,
only the axillary tumour. The presence of a hypoechoic, not
well-defined heterogeneous mass, which is differentially diagnosed
as a sebaceous cyst, without signs of inflammation, such as in
hydradenitis, is considered to be accessory breast cancer (20). Mammography may contribute additional
information, such as for the evaluation of the axillae, for
micro-calcifications, and the breasts (23). In the case of a suspicious lesion,
fine-needle aspiration biopsy or core biopsy of the axillary mass
should be performed to harvest cells or tissue for histological
diagnosis (8). Since the accessory
breast tissue in the present study was found in the axilla, far
from the pectoral breast parenchyma, the diagnosis of accessory
breast carcinoma was favoured. The identification of normal breast
tissue adjacent to the invasive carcinoma in the axilla strongly
suggested invasive carcinoma arising in the ectopic breast tissue.
The absence of accompanying lymphoid tissue further disfavoured a
diagnosis of tumour metastasis in the axillary lymph node from
breast cancer. Notably, accessory breast cancer may be
macroscopically similar to a lymph node with metastatic carcinoma
(20). Therefore, histological
examination should be performed for all tissue nodules in the
axilla.
Similarly to primary breast cancer, accessory breast
cancer is treated surgically, which is supplemented with pre- or
post-operative chemotherapy, radiotherapy and endocrine therapy. It
is controversial as to whether the breast located on the same side
as the accessory breast cancer should be removed as well (22,24).
Certain studies have recommended radical mastectomy of the
ipsilateral breast if the regional lymph nodes are diagnosed with
carcinoma (11,24). However, Cogwells and Czerny reported
that ipsilateral mastectomy does not result in an improved
prognosis for patients with ectopic breast carcinoma (25). Evans and Guyton suggested that radical
or modified radical surgery offered no advantage over local
excision combined with axillary dissection or radiation with
respect to outcome (2). It has been
proposed that the surgical procedure of choice for ectopic breast
carcinoma involves a wide resection of the tumour with surrounding
tissue, including the skin and regional lymph nodes (3,26).
Mastectomy is not indicated if clinical examination, mammography
and ultrasonography of the anatomic breast reveal no signs of
disease, but should be performed when differential diagnosis is
challenging (17,27). If mastectomy is not performed,
particularly careful follow-up is necessary to exclude any later
manifestations of an occult primary neoplasm in the breast.
The present study hypothesizes that, when the
accessory breast tissue is closely connected to normal breast
tissue, the indications for surgery should be the same as those for
a tumour anatomically situated in the breast. By contrast, when the
accessory gland constitutes a separate anatomical structure, the
resection of normal breast tissue appears to be unnecessary. There
have been few studies on neoadjuvant chemotherapy as a treatment
for locally advanced accessory breast cancer (20,28).
Chemotherapy with anthracycline and taxane is generally recommended
for the treatment of locally advanced accessory breast cancer, as
it is for the usual form of breast cancer (7). The principles of post-operative
treatment are also the same as those for normal breast carcinoma
(9). External radiotherapy of the
tumour site must be performed to enable increased local control.
However, radiation of the homolateral anatomic breast is not
systematically performed (29). In
the present study, 3 patients were administered with radiation
therapy subsequent to surgery, while the safety and predictability
have not yet been elucidated. In addition, there is a lack of
evidence assessing the middle- and long-term efficacy of radiation
therapy. Systemic adjuvant therapy is more frequently required due
to the common occurrence of lymph node disease and is performed
following the same guidelines as those used for anatomic breast
carcinoma treatment (17).
In breast cancer, homolateral axillary and internal
mammary nodes are considered possible sites of lymphatic metastasis
(5). The lymphatic spread of axillary
breast cancer is likely to only occur towards the homolateral
axillary nodes and then towards the supraclavicular nodes, as this
is the normal lymphatic drainage pathway of the subcutaneous and
cutaneous tissues of the armpit (8).
It has been reported that 37% of cases occurred prior to the age of
45 years, and due to early metastatic spread, demonstrated an even
higher incidence of lymph node involvement (59–88%) compared with
primary breast carcinoma located in the external superior sector
(51%) (7). The prognosis of accessory
breast carcinoma is challenging to establish, primarily due to
absent or limited follow-up data as well as small sample sizes. In
addition, it is challenging to identify a clear histopathological
and clinical distinction between accessory and normal breast
carcinoma (23). Certain studies have
hypothesized that accessory breast tissue is more prone to
malignancy compared with the normal breast parenchyma (30,31).
Marshall et al reported that the poorer outcomes in ectopic
breast cancer relative to general breast cancer reflected less
effective clinical disease management compared with the disease
process itself (3). Certain studies
have reported that the outcomes of ectopic breast cancer are poorer
than those of normal breast cancer as the tumour is located near
the axillary lymph nodes and is therefore associated with early
metastasis to these nodes (32).
Follow-up data is provided for a limited number of
patients, indicating a four-year post-treatment survival of 9.4%,
which has been calculated in a meta-analysis (2). At the time of diagnosis, the majority of
patients with accessory breast carcinoma were in an advanced
clinical stage, with nodal metastases or an unresectable tumour due
to size (20,28). Thus, the prognosis of accessory breast
cancer may be worse compared with the prognosis of breast cancer
arising in the proper mammary gland, although no long-term
follow-up data regarding the prognosis of accessory breast cancer
are available (15).
The present study reported the cases of 11 patients
with rare breast carcinoma that arose in an accessory mammary
gland. Due to the rarity of this disease and the consequential lack
of clinical awareness, the administration of appropriate disease
management is often delayed. The possibility of accessory mammary
carcinoma should be considered even in male patients with neoplasms
located in the axilla. The correct identification of accessory
breast tissue is an important factor in the differential diagnosis
of axillary tumours. Recognition of this disease by clinicians and
pathologists and close communication between the two are important
to prevent a misdiagnosis of malignancy and performing
unnecessarily extensive surgery.
References
|
1
|
Gao YG, Zhang SH and Wang Y: A case of
accessory mammary cancer in a male patient and a literature review.
Eur J Gynaecol Oncol. 35:452–455. 2014.PubMed/NCBI
|
|
2
|
Evans DM and Guyton DP: Carcinoma of the
axillary breast. J Surg Oncol. 59:190–195. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Marshall MB, Moynihan JJ, Frost A and
Evans SR: Ectopic breast cancer: Case report and literature review.
Surg Oncol. 3:295–304. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hao JY, Yang CC, Liu FF, et al: Accessory
breast cancer occurring concurrently with bilateral primary
invasive breast carcinomas: A report of two cases and literature
review. Cancer Biol Med. 9:197–201. 2012.PubMed/NCBI
|
|
5
|
Howard BA and Gusterson BA: Human breast
development. J Mammary Gland Biol Neoplasia. 5:119–137. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pathak S and Preston J: A rare case of
multiple accessory breast tissue in the axillae, lower abdomen and
vulval areas. J Obstet Gynaecol. 27:531–533. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Visconti G, Eltahir Y, Van Ginkel RJ, Bart
J and Werker PM: Approach and management of primary ectopic breast
carcinoma in the axilla: Where are we? A comprehensive historical
literature review. J Plast Reconstr Aesthet Surg. 64:e1–11. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schmidt H: Supernumerary nipples:
Prevalence, size, sex and side predilection - a prospective
clinical study. Eur J Pediatr. 157:821–823. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scanlan KA and Propeck PA: Accessory
breast tissue in an unusual location. AJR Am J Roentgenol.
166:339–340. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Basu S, Bag T, Saha SK and Biswas PC:
Accessory breast in the perineum. Trop Doct. 33:2452003.PubMed/NCBI
|
|
11
|
Chan NG, Penswick JL, Labelle E and Driman
DK: Ectopic breast tissue presenting as an anal polyp. Can J Surg.
50:E23–E24. 2007.PubMed/NCBI
|
|
12
|
Page RN, Dittrich L, King R, Boulos F and
Page DL: Syringomatous adenoma of the nipple occurring within a
supernumerary breast: A case report. J Cutan Pathol. 36:1206–1209.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yoon HJ, Sung SH, Moon BI and Kim BS:
Invasive ductal carcinoma arising from dense accessory breast
visualized with 99mTc-MIBI breast-specific γ imaging. Clin Nucl
Med. 39:717–720. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Devine C, Courtney CA, Deb R and Agrawal
A: Invasive lobular carcinoma arising in accessory breast tissue.
World J Surg Oncol. 11:472013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yamamura J, Masuda N, Kodama Y, Yasojima
H, Mizutani M, Kuriyama K and Sekimoto M: Male breast cancer
originating in an accessory mammary gland in the axilla: A case
report. Case Rep Med. 2012.286210PubMed/NCBI
|
|
16
|
Amsler E, Sigal-Zafrani B, Marinho E and
Aractingi S: Ectopic breast cancer of the axilla. Ann Dermatol
Venereol. 129:1389–1391. 2002.(In French). PubMed/NCBI
|
|
17
|
Youn HJ and Jung SH: Accessory breast
carcinoma. Breast Care (Basel). 4:104–106. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yerra L, Karnad AB and Votaw ML: Primary
breast cancer in aberrant breast tissue in the axilla. South Med J.
90:661–662. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pardo M, Silva F, Jiménez P and Karmelic
M: Mammary carcinoma ine ectopic breast tissue. A case report. Rev
Med Chil. 129:663–665. 2001.(In Spanish). PubMed/NCBI
|
|
20
|
Madej B, Balak B, Winkler I and Burdan F:
Cancer of the accessory breast - a case report. Adv Med Sci.
54:308–310. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang RR, Bevan S, Sun P, Lu JZ and Peng
Y: Unusual presentation of multiple fibroadenomas in bilateral
breasts and axillary accessory breast. Breast Cancer (Auckl).
6:95–99. 2012.PubMed/NCBI
|
|
22
|
Matsuoka H, Ueo H, Kuwano H, Sugimachi K
and Inokuchi K: A case of carcinoma originating from accessory
breast tissue of the axilla. Gan No Rinsho. 30:387–391.
1984.PubMed/NCBI
|
|
23
|
Nakao A, Saito S, Inoue F, Notohara K and
Tanaka N: Ectopic breast cancer: A case report and review of the
Japanese literature. Anticancer Res. 18:3737–3740. 1998.PubMed/NCBI
|
|
24
|
Tjalma WA and Senten LL: The management of
ectopic breast cancer - case report. Eur J Gynaecol Oncol.
27:414–416. 2006.PubMed/NCBI
|
|
25
|
Cogswell H and Czerny EW: Carcinoma of
aberrant breast of the axilla. Am Surg. 27:388–390. 1961.PubMed/NCBI
|
|
26
|
Livesey JR and Price BA: Metastatic
accessory breast carcinoma in a thoracic subcutaneous nodule. J R
Soc Med. 83:799–800. 1990.PubMed/NCBI
|
|
27
|
Markopoulos C, Kouskos E, Kontzoglou K,
Gogas G, Kyriakou V and Gogas J: Breast cancer in ectopic breast
tissue. Eur J Gynaecol Oncol. 22:157–159. 2001.PubMed/NCBI
|
|
28
|
Takeyama H, Takahashi H, Tabei I, Fukuchi
O, Nogi H, Kinoshita S, Uchida K and Morikawa T: Malignant neoplasm
in the axilla of a male: Suspected primary carcinoma of an
accessory mammary gland. Breast Cancer. 17:151–154. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Routiot T, Marchal C, Verhaeghe JL,
Depardieu C, Netter E, Weber B and Carolus JM: Breast carcinoma
located in ectopic breast tissue: A case report and review of the
literature. Oncol Rep. 5:413–417. 1998.PubMed/NCBI
|
|
30
|
Ghosn SH, Khatri KA and Bhawan J:
Bilateral aberrant axillary breast tissue mimicking lipomas: Report
of a case and review of the literature. J Cutan Pathol. 34:(Suppl
1). 9–13. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Francone E, Nathan MJ, Murelli F, Bruno
MS, Traverso E and Friedman D: Ectopic breast cancer: Case report
and review of the literature. Aesthetic Plast Surg. 37:746–749.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Copeland MM and Geschickter CF: Diagnosis
and treatment of premalignant lesions of the breast. Surg Clin
North Am. 30:1717–1741. 1950.PubMed/NCBI
|