Introduction
Ewing's sarcoma of the bone is the second most
frequently occurring malignant bone tumor in children and
adolescents. It is a member of the Ewing's sarcoma family of
tumors, which also includes primitive neuroectodermal tumors,
Ewing's soft tissue sarcomas and Askin's tumors. The Ewing's
sarcoma family of tumors are high-grade aggressive lesions that
most commonly originate in the bone, and are associated with large
soft tissue masses and frequent metastases. The majority of Ewing's
sarcomas of the bone are located in the lower extremities and
pelvic girdle, but occasionally arise in the ulna (1). Previous treatments for Ewing's sarcomas,
such as surgery (alone), radiotherapy or mono-chemotherapy, have
failed to achieve ideal results. The majority of patients succumbed
within two years, and the five-year survival rate was <20%
(2). However, with progress in
chemotherapy, the prognosis for patients with Ewing's sarcoma has
improved considerably during the past three decades (3). Currently, chemotherapy and surgery are
the standard treatment for Ewing's sarcomas (4). The ulna is an uncommon site for these
malignant and aggressive tumors. Thus, the surgical options for
reconstruction of the elbow are limited and technically challenging
(4–8).
The current study presents the case of a successful sub-total
resection and reconstruction using a non-vascularized, autogenous
fibular graft and hernia mesh in a 29-year-old male with Ewing's
sarcoma of the ulna. Written informed consent was obtained from the
patient.
Case report
A 29-year-old male presented to the Second
Affiliated Hospital (Hangzhou, Zhejiang, China) with a 3-month
history of repeated left forearm pain. The initial consultation was
performed on September 10, 2012. A plain radiograph demonstrated an
osteolytic lesion with cortical destruction involving the proximal,
middle and distal ulna (Fig. 1).
Magnetic resonance imaging demonstrated an intramedullary tumor
that involved nearly the full length of the ulna, with the
exception of the proximal olecranon (Fig.
2). The surrounding cortex was partially involved, and the
soft-tissue components around the tumor appeared patchy and
hyperintense on T2-weighted images. The elbow and wrist joints were
tumor free. The patient underwent an open biopsy, and frozen
section examination demonstrated proliferation of small round cells
with round-to-oval nuclei. Subsequently, immunohistochemistry
revealed that the cell membrane was strongly positive for vimentin
and cluster of differentiation 99. Thus, analysis of the tumor
biopsy supported a diagnosis of Ewing's sarcoma. A bone scan
revealed uptake only at the left ulna, and chest computed
tomography showed no evidence of metastatic disease. Therefore, the
patient was classified as having stage IIB according to the
Enneking surgical staging system (5).
On the following day, the patient received two 6-week courses of
neoadjuvant chemotherapy, including 2.9 g ifosfamide (days 1–5 and
11–15), 150 mg cisplatin (day 22) and 95 mg doxorubicin (day 24).
Restaging magnetic resonance imaging indicated tumor regression
(Fig. 2), which confirmed the
efficacy of the chemotherapy.
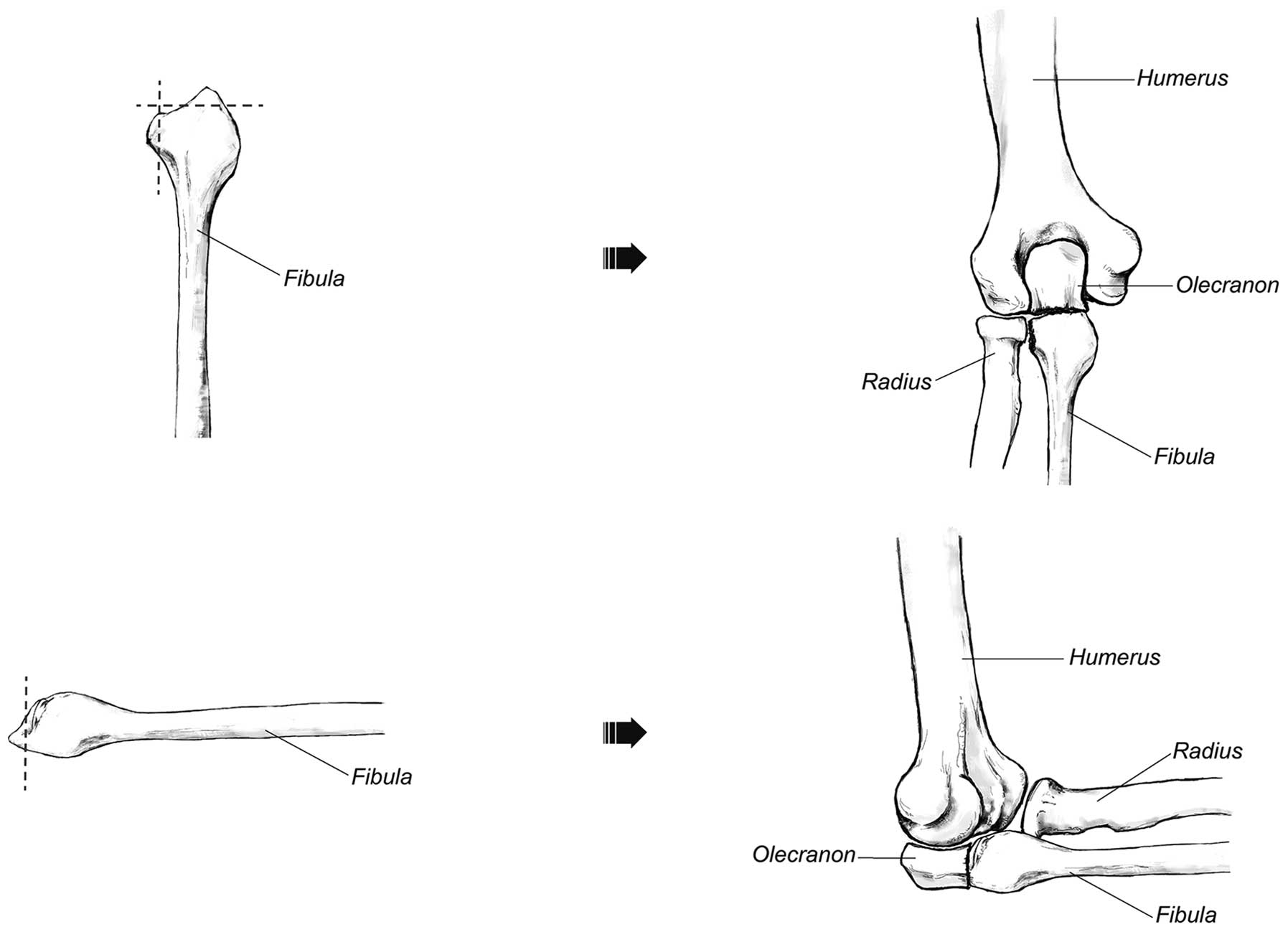
As the tumor involved nearly the full length of the
ulna, the patient underwent a sub-total resection of the ulna
(except for half of the olecranon process). Intraoperative frozen
sections revealed a negative tumor margin. Reconstruction of the
bony defect was performed using a non-vascularized, autologous,
fibular graft harvested from the ipsilateral leg. The length of the
harvested fibula, including the fibular head, was 15 cm. The
fibular graft was drilled and wrapped with hernia mesh to recreate
the forearm interosseous ligament (Fig.
3). Next, the mesh was sutured to the remnant interosseous
ligament of the radius to hold the graft in position. The fibular
head was modified to match the remaining olecranon process and the
articular surface at the ulnotrochlear and proximal radioulnar
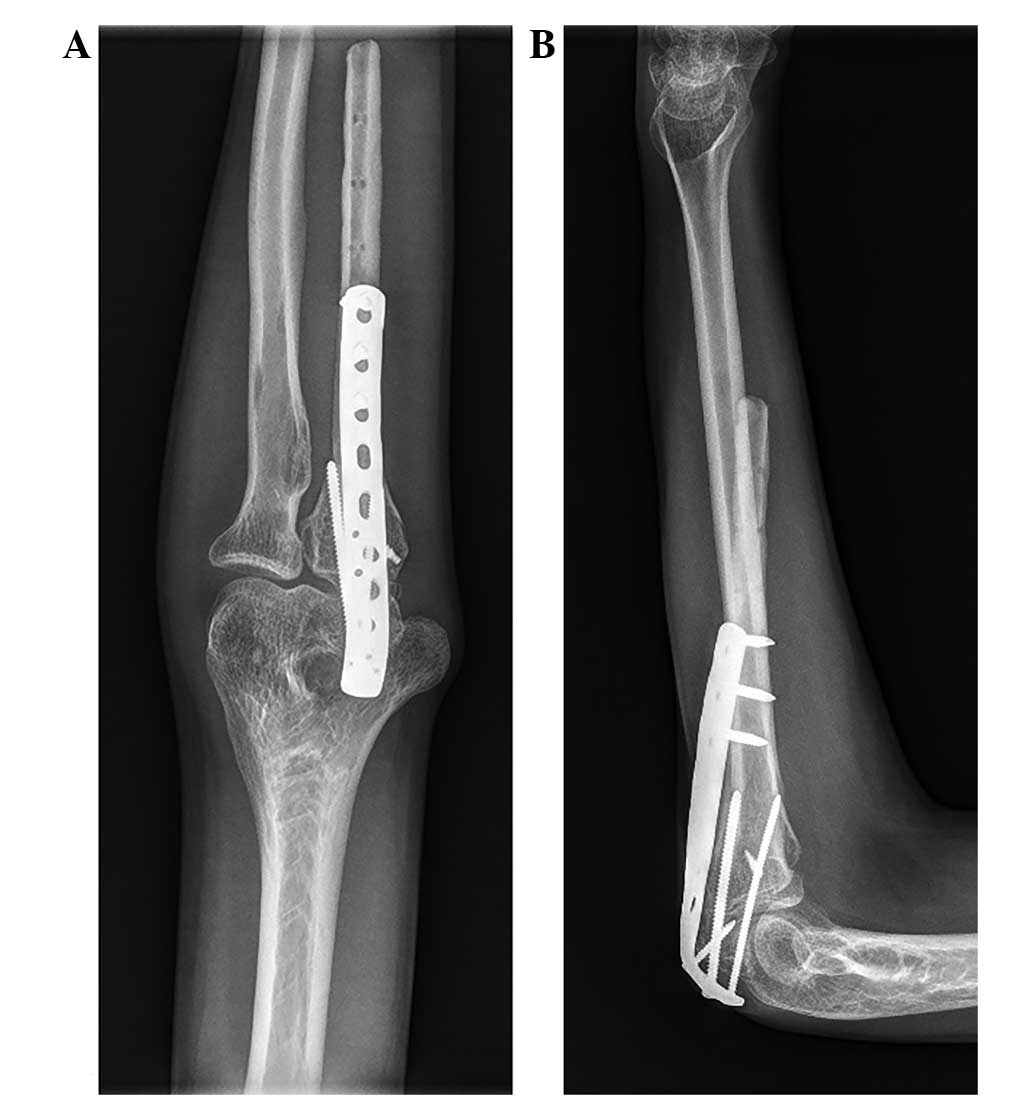
joints to reconstruct the elbow joint (Fig. 4). This was fixed to the remnant
olecranon process with a plate and screws. To stabilize the elbow
joint, a Kirschner wire was used to fix the head of the radius and
fibula. In addition, the medial collateral ligament and capsule of
the elbow were fixed to the fibular head by an anchor.
Post-operative chemotherapy was continued, and the Kirschner wire
was removed 4 weeks after surgery. To protect the reconstructed
elbow joint, 4 weeks of full immobilization with a gypsum cast at
90° flexion was applied after surgery, followed by an additional 4
weeks of passive- and active-assisted flexion and extension of the
left elbow.
At the 2-year follow-up, there was no evidence of
local recurrence or distant metastasis (Fig. 5). The fibular graft was united with
the olecranon proximally, and the functional recovery was
satisfactory, with active movement of the elbow from 0° to 135°,
forearm pronation to 30°, supination to 85° and full hand function
(Fig. 6). The grip power of the left
hand was 36 kg, which was 86% of the contralateral side (42 kg). No
morbidity in the donor site was observed in the leg where the
fibula was harvested and the functional capability of the leg was
good. Furthermore, the patient had been able to return to his
previous occupation.
Discussion
Malignant and aggressive tumors located within the
ulna are relatively rare, although there have been reports of
osteosarcoma, primary giant cell tumors and Ewing's sarcoma of the
ulna. Salvaging the limb following an ulnar tumor resection poses a
complex, reconstructive challenge (6,7,9–11). Various
options have been reported for the reconstruction of the elbow
joint following ulnar tumor resections, such as radius
neck-to-humerus trochlea transposition, endoprosthetic
reconstruction, allografts, vascularized fibular grafts and
extracorporeal irradiation (6,7,9,10). Due to
the location of the tumors, previous studies primarily involved
reconstructions of partial ulna defects, and the remnant ulna
provided the basis for bone grafts or prosthesis implantation.
However, malignant and aggressive tumors invading nearly the full
length of the ulna have rarely been reported. Thus, the present
patient presented a unique surgical challenge. Sułko (6) reported a patient with Ewing's sarcoma
who underwent radius neck-to-humerus trochlea transposition
following an extensive resection of the proximal portion of the
ulna. The technique of radius neck-to-humerus trochlea
transposition was a good candidate for reconstruction of the elbow
joint following wide resection of the ulna. However, the functional
rotation of the forearm may be unsatisfactory. Duncan et al
(7) performed this procedure in 2
adult patients. One patient achieved 20° pronation, but no
supination, and the second patient achieved 10° pronation and
limited supination ability (9).
Therefore, in the present study, it was proposed that the elbow
joint would be reconstructed using a non-vascularized, autogenous
fibular graft and hernia mesh. The functional recovery was
satisfactory, particularly for functional forearm rotation. The
patient achieved forearm pronation to 30° and supination to
85°.
In the present case, as a sub-total resection of the
ulna was performed, disruption of the forearm interosseous membrane
was inevitable. The forearm interosseous membrane is a dynamic and
complex fibrous structure that maintains the stability of the
longitudinal forearm and transmits forces between the radius and
the ulna (8). To reconstruct the
forearm interosseous membrane, a hernia mesh, which has biological
properties to provide mechanical constraint, was applied in the
present study. However, the purpose of reconstructing the forearm
interosseous membrane was not only to restore its own function, but
also to maintain the function of the forearm and elbow joint. This
was very important in three ways. First, the mesh assisted in
holding the fibular graft in position. Second, it repaired the
connection between the radius and ulna to maintain the stability of
the elbow joint; the stability of the elbow joint is highly
dependent on the integrity of the interosseous membrane and the
balance between the radius, ulna and humerus. Additionally, the
hernia mesh may provide a biocompatible scaffold for soft tissue
ingrowth. Third, it may improve active movement of the elbow and
functional rotation of the forearm. Following a sub-total resection
of the ulna, the flexor apparatus of the elbow was primarily
dependent on the biceps tendon for normal movement; the
reconstruction of the interosseous membrane can transmit forces
from the radius to the ulna to drive elbow flexion. Similarly, the
force transmission between the radius and ulna by the interosseous
membrane can also aid in restoring the functional forearm rotation.
This method of reconstruction of the forearm interosseous membrane
has not been previously reported, but the use of synthetic mesh
during limb salvage surgery is not rare. Marulanda et al
(12) suggested that the application
of a synthetic vascular mesh for a reconstruction of the proximal
humerus may reduce the number of dislocations and aid in soft
tissue attachment. In the present case, the elbow and forearm
rotation was satisfactory, and no complications were observed.
Preservation of the proximal half of the olecranon
during excision has been performed for the treatment of proximal
ulna tumors. Goyal et al (11)
reported a case of a desmoplastic fibroma of the proximal ulna that
was treated with excision and reconstruction of the olecranon with
a fibular graft. Bone-to-bone repair is often successful when a
small region of the proximal olecranon may be preserved in
continuity with the tendon insertion. This maintains a certain
degree of integrity of the extensor apparatus of the elbow,
resulting in useful elbow function and providing stability to the
elbow joint. This technique was also adopted in the present study
patient. To maintain stability in the elbow joint, a Kirschner wire
was used to fix the fibular head and radius. Furthermore, an anchor
was used to fix the medial collateral ligament, as its primary
function is to resist elbow valgus overload.
Complications that could occur following
reconstructive surgery include non-union, infection, joint
degeneration and tumor recurrence. In the present patient, the
non-vascularized, autogenous fibula was used as the bone graft. A
free vascularized fibula may be a better choice for elbow
reconstruction. For the irregular shape of the fibular head, it was
hard to match the articular surface at the ulnotrochlear and
proximal radioulnar joints. Therefore, the fibular head was
modified to reconstruct the elbow joint. Moreover, a two-year
follow-up may be insufficient, and a longer follow-up is required
to focus on oncological surveillance and long-term functional
outcomes.
Additionally, the distal end of the ulna was not
reconstructed in the present case, as a previous study demonstrated
that routine reconstruction of this bone defect is not necessary
following en bloc resection of tumors of the distal end of the ulna
(13). Furthermore, the current
patient was satisfied with the function and appearance of the upper
extremity.
In conclusion, Ewing's sarcoma of the ulna is rare
and the surgical options for reconstruction are technically
challenging. In the present case, a successful sub-total resection
of the ulna and reconstruction using a non-vascularized, autogenous
fibular graft and hernia mesh was performed. This case indicates
that using hernia mesh to reconstruct the interosseous membrane of
the forearm may maintain the stability of the elbow joint and
improve functional rotation of the forearm.
References
|
1
|
Moore DD and Haydon RC: Ewing's sarcoma of
bone. Cancer Treat Res. 162:93–115. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Widhe B and Widhe T: Initial symptoms and
clinical features in osteosarcoma and Ewing sarcoma. J Bone Joint
Surg Am. 82:667–674. 2000.PubMed/NCBI
|
|
3
|
Cotterill SJ, Ahrens S, Paulussen M,
Jürgens HF, Voûte PA, Gadner H and Craft AW: Prognostic factors in
Ewing's tumor of bone: Analysis of 975 patients from the European
intergroup cooperative Ewing's Sarcoma study group. J Clin Oncol.
18:3108–3114. 2000.PubMed/NCBI
|
|
4
|
Wunder JS, Paulian G, Huvos AG, Heller G,
Meyers PA and Healey JH: The histological response to chemotherapy
as a predictor of the oncological outcome of operative treatment of
Ewing sarcoma. J Bone Joint Surg Am. 80:1020–1033. 1998.PubMed/NCBI
|
|
5
|
Enneking WF: A system of staging
musculoskeletal neoplasms. Clin Orthop Relat Res. 204:9–24.
1986.PubMed/NCBI
|
|
6
|
Sułko J: Elbow reconstruction following an
extensive resection of the proximal part of the ulna in a patient
with Ewing Sarcoma. A case report. JBJS Case Connect.
3:e1112013.
|
|
7
|
Duncan SF, Athanasian EA and Healey JH:
Radius neck-to-humerus trochlea transposition for elbow
reconstruction after resection of the proximal ulna: Report of 2
cases. J Hand Surg Am. 33:1384–1387. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
McGinley JC and Kozin SH: Interosseous
membrane anatomy and functional mechanics. Clin Orthop Relat Res.
383:108–122. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sewell MD, Hanna SA, Pollock RC, Aston WJ,
Skinner JA, Blunn GW, Cannon SR and Briggs TW: Proximal ulna
endoprosthetic replacement for bone tumours in young patients. Int
Orthop. 36:1039–1044. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ogose A, Hotta T, Shibata M, Kawashima H
and Endo N: Combined use of free vascularised fibula graft and
extracorporeally irradiated osteochondral graft for osteosarcoma of
the proximal ulna. Oncol Lett. 1:133–135. 2010.PubMed/NCBI
|
|
11
|
Goyal T, Rastogi S and Tripathy SK:
Desmoplastic fibroma of ulna: Excision and reconstruction of
olecranon with a fibular graft. Indian J Orthop. 47:207–210. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Marulanda GA, Henderson E, Cheong D and
Letson GD: Proximal and total humerus reconstruction with the use
of an aortograft mesh. Clin Orthop Relat Res. 468:2896–2903. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cooney WP, Damron TA, Sim FH and Linscheid
RL: En bloc resection of tumors of the distal end of the ulna. J
Bone Joint Surg Am. 79:406–412. 1997.PubMed/NCBI
|