Introduction
Meningioma is a common intracranial tumour,
accounting for 13–19% of all primary brain tumors (1). This tumor is generally encapsulated and
benign (2). The symptoms of
meningioma depend on the pressure of the tumor on the brain or
spinal cord and the intracranial location of the tumor (3). Symptoms, such as seizures, single or
multiple muscle twitches, spasms, loss of control of body
functions, change in sensation and partial or total loss of
consciousness, are associated with the different locations of the
mass (1,4). Meningiomas accounted for ~33.8% of all
the primary brain and central nervous system tumors reported in the
United States between 2002 and 2006 (2). Furthermore, in recent decades, increased
exposure to risk factors has determined an increase in the
incidence of primary brain tumors, inclusive of meningioma, in
several countries (5). The
predominant risk factor identified is the exposure to ionizing
radiation; however, other risk factors may be associated with the
risk of meningioma, including elevated estrogen and/or progesterone
hormone levels (2,6,7), head
trauma (2), cell phone use (2,8), breast
cancer (2), occupation (2), diet (2).
Notably, a significant inverse correlation has been identified
between meningioma and allergies (2,9); Linos
et al (10) revealed that
individuals with a history of allergy exhibited a lower risk of
developing brain tumours than individuals with no history of
allergy. Meningiomas have a higher incidence rate among female
individuals, with a female to male ratio of ~2:1 (5). In addition, age-specific incidence rates
indicate that risk increases with age. Prevalence rates for
non-Hispanic individuals of African descent are marginally higher
(6.67 per 100,000 persons) compared with Caucasian non-Hispanic and
Hispanic individuals (5.90 and 5.94 per 100,000 persons,
respectively) (2,4). The primary treatment strategy for
meningiomas is total resection surgery if the tumor is benign and
in an area of the brain where it can be safely and completely
removed. Subsequently, radiation therapy is applied for the most
malignant cases of meningioma or when surgery is not feasible due
to the meningioma location.
Extracranial meningiomas are uncommon (accounting
for <2% of meningiomas) (11),
particularly those extending into the middle ear. The present study
described a rare case of meningioma extending into the middle ear
from the middle cranial fossa through the tegmen tympani. Written
informed consent was obtained from the patient.
Case report
In May 2004, a 56-year-old woman presented to the
Ear Nose and Throat Unit of Santa Maria delle Grazie Hospital
(Naples, Italy) with an intense headache associated with vertigo
that was treated with intravenous administration of 10% glycerol
and 8 mg dexamethasone, with no results. After approximately two
months, the patient had developed generalized seizure episodes.
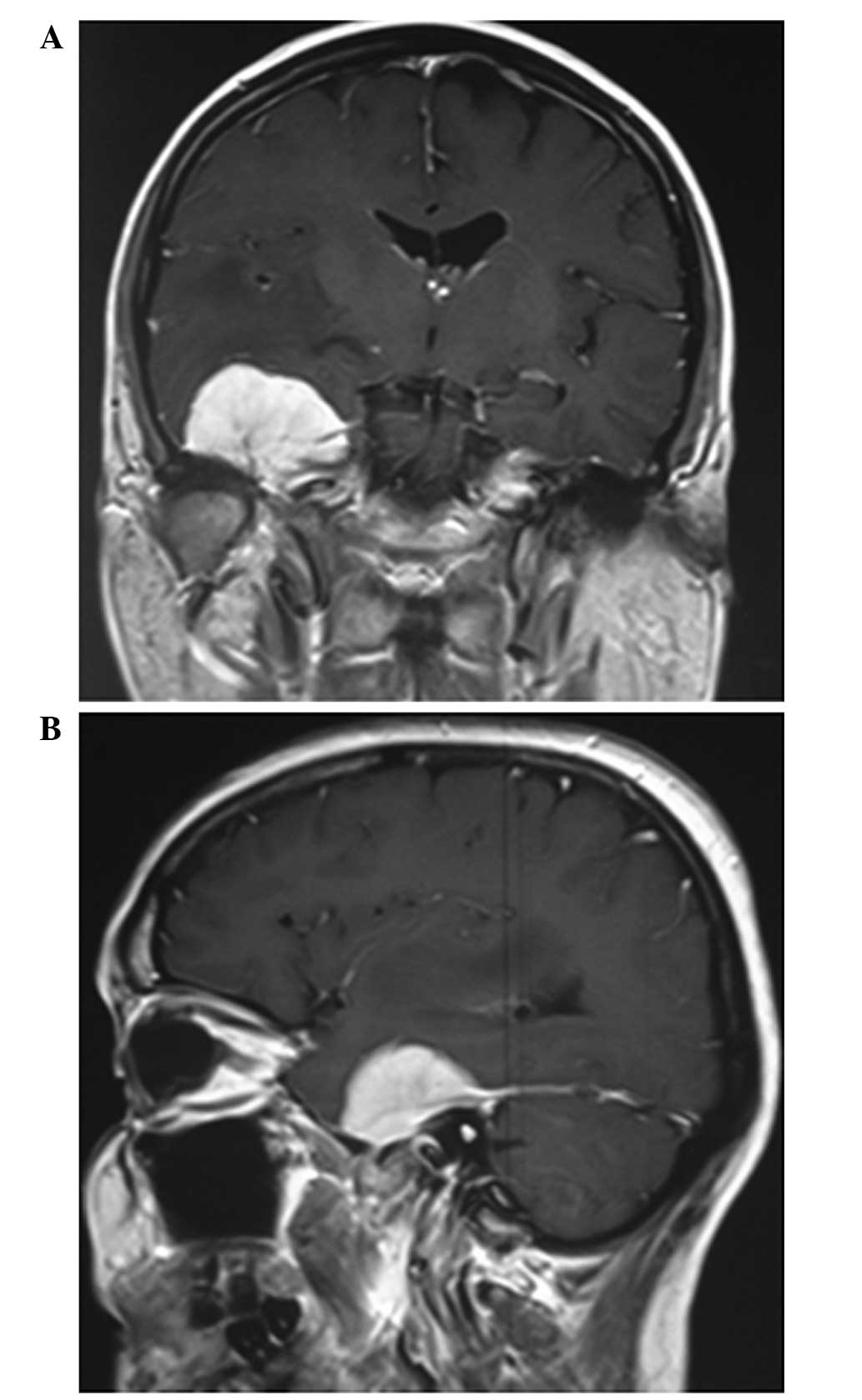
Brain magnetic resonance imaging (MRI) with gadolinium revealed the
presence of a large (37×40×25 mm), T1-hypointense lesion widely
invading the right middle cranial fossa with compression of the
adjacent structures and dislocation of the middle cerebral artery.
In addition, the lesion exhibited high contrast enhancement and a
dural tail (Fig. 1A and B). Based on
these radiological features of the lesion, a diagnosis of
meningioma was determined. A right pterional craniotomy with
partial extirpation of the lesion was performed, since the tumor
presented a large and deep implantation base on the tentorial dura
of the petrous bone roof.
The postoperative course was uneventful.
Histopathological examination of the excised tumor determined a
diagnosis of transitional meningioma. Subsequently, the patient
underwent postoperative stereotactic radiotherapy (200 cGy, six
days a week) for five weeks, to treat the residual tumor, and
clinico-radiological follow-up.
In March 2006, two years after surgery, the patient
underwent appositional transtympanic drainage in the right ear due
to right chronic otitis media with effusion at the Complex Unit of
Otolaryngology and Neck Surgery of Monaldi Hospital (Naples,
Italy); however, no substantial clinical improvement occurred. The
patient experienced progressive worsening of right-ear hearing
loss, otorrhea and otalgia, despite frequent antibiotic therapies
(with quinolones and cephalosporins). Therefore, the patient
underwent petrous bone computed tomography (CT). The CT scan
identified an intratympanic mass that enveloped the ossicular chain
without erosion and thickening of the tegmen tympani (Fig. 2A and B).
In January 2010, the patient was admitted to the Ear
Nose and Throat Unit of Santa Maria delle Grazie Hospital with
right otalgia, otorrhea, vertigo and increasing right hypoacusis,
which had occurred intermittently for the past 20 years. A right
otomicroscopy identified granulation tissue in the drainage tube
and the hyperemic, bulging and everted tympanic membrane. A pure
tone audiogram determined right anacusis and left-sided
sensorineural hearing loss. In addition, pre-operative brain MRI
confirmed the presence of a hyperintense tissue mass, occupying the
tympanic cavity (Fig. 3).
Consequently, a right canal-wall-down (CWD)
tympanoplasty was performed. A granulomatous-like mass invading the
tympanic cavity, mastoid antrum and oval window was removed
(Fig. 4). Histological analysis
confirmed the lesion to be transitional meningioma with identical
histology to the previous tumor and thus, it was considered to be a
section of the tumor that was resected in 2004.
The patient underwent clinico-radiological follow-up
and, five years later, exhibited no evidence of middle ear tumor
recurrence (Fig. 5).
Discussion
Meningioma is a common intracranial tumor,
accounting for 13–19% of all the primary brain tumors (1). Meningiomas are slow-growing and
originate from the arachnoid villi of the meninges (11). Extracranial meningioma are uncommon
(accounting for <2% of meningiomas) (11), particularly those extending into the
middle ear. Furthermore, the majority of intracranial meningiomas
are benign (90%), with atypical (6%) and malignant forms (2%)
occurring less frequently (12).
Meningiomas are typically diagnosed in adults aged
>60 years and the incidence rate increases with age. In
addition, these tumors occur more often in women than in men
(13). Depending on the location of
the tumor, patients can present with a variety of neurological
symptoms, including headaches, speech problems, visual
disturbances, cognitive deficits, motor deficits and epilepsy
(4). In cases of temporal bone
meningioma, otalgia is the most common feature, although hearing
loss (conductive, mixed or sensorineural) (14), facial palsy and tinnitus are also
common (15). A lower proportion of
patients present with other cranial nerve palsies or vestibular
symptoms (16).
In the current case, the patient exhibited a middle
fossa meningioma that presented with epileptic seizures and
symptoms of chronic otitis media. Chronic otitis media has been
reported to occur in 16% of intratympanic meningiomas (17), possibly due to the obstruction of the
Eustachian tube upon extension of the tumor into the middle ear
cavity. Temporal bone meningioma scans follow multiple extension
pathways: The tegmen tympani, the jugular foramen and the internal
auditory canal (16). Based on their
imaging characteristics, meningiomas are stratified into three
groups with different primary locations and vectors of spread. The
jugular foramen and tegmen tympani meningiomas are characterized by
spread to the middle ear cavity. By contrast, internal auditory
canal meningiomas spread to the intralabyrinthine structures
(18). In the present case,
meningioma primary to the tegmen tympani arose from the floor of
the middle cranial fossa and spread inferomedially into the middle
ear cavity. A number of radiological features (including thickening
of the tegmen tympani, absence of bone and ossicular erosion and
contrast enhancement of the lesion) (18) helped to distinguish meningioma from
cholesteatoma in the current study. Furthermore, the jugular
foramen, internal acoustic canal and labyrinthic area appeared
healthy and free of disease.
Four histological subtypes of meningioma have been
reported thus far: Meningotheliomatous, transitional, fibrous and
angioblastic. Extracranial meningiomas are more often transitional
or meningotheliomatous (19). In the
present case, the extracranial lesion was diagnosed as a
transitional meningioma.
Surgery is the treatment of choice for meningioma,
with overall survival rates of 85, 75 and 70% at 5, 10 and 15
years, respectively. However, complete resection is often not
considered to be possible, particularly in large tumors (20). Furthermore, in contrast to their
intracranial counterparts, meningiomas involving the temporal bone
do not often exhibit well-demarcated tumor margins (21).
The role of radiotherapy in the treatment of
meningiomas remains controversial and is generally reserved for the
adjuvant treatment of non-radically removed or recurrent
meningiomas (19). Thus, in the
present case, the patient underwent neurosurgical therapy with
successive radiotherapy. Due to the persistence of the residual
tumor in middle fossa for a number of years, the patient underwent
a CWD tympanoplasty for the middle ear tumor.
In conclusion, temporal bone meningioma involving
the middle ear is uncommon. Due to presenting similar symptoms with
chronic otitis media, diagnosing meningioma is often difficult.
However, imaging techniques can facilitate distinguishing between
meningioma tumors and other diseases of the middle ear. In
particular, in cases of hyperplastic chronic otitis media in
patients with a previous meningioma, a temporal bone CT and MRI
with gadolinium should be performed. Furthermore, treatment
typically requires sequential neurosurgical and otosurgical
approaches, followed by postoperative radiotherapy in cases of
partial exeresis.
References
|
1
|
Prayson RA: Middle ear meningiomas. Ann
Diagn Pathol. 14:149–153. 2000. View Article : Google Scholar
|
|
2
|
Wiemels J, Wrensch M and Claus EB:
Epidemiology and etiology of meningioma. J Neurooncol. 99:307–314.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
American Society of Clinical
Oncology:Meningioma: Symptoms and Signs. http://www.cancer.net/cancer-types/meningioma/symptoms-and-signsAccessed.
January 13–2015.
|
|
4
|
vanAlkemade H, de Leau M, Dieleman EM,
Kardaun JW, van Os R, Vandertop WP, van Furth WR and Stalpers LJ:
Impaired survival and long-term neurological problems in benign
meningioma. Neuro Oncol. 14:658–666. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Central Brain Tumor Registry of the United
States, . CBTRUS Statistical Report: Primary Brain and Central
Nervous System Tumors Diagnosed in Eighteen States in
2002–2006CBTRUS. Hinsdale, IL: pp. 13–26. 2009–2010
|
|
6
|
Claus EB, Black PM, Bondy ML, Calvocoressi
L, Schildkraut JM, Wiemels JL and Wrensch M: Exogenous hormone use
and meningioma risk: what do we tell our patients? Cancer.
110:471–476. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vadivelu S, Sharer L and Schulder M:
Regression of multiple intracranial meningiomas after cessation of
long-term progesterone agonist therapy. J Neurosurg. 112:920–924.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Inskip PD, Tarone RE, Hatch EE, Wilcosky
TC, Shapiro WR, Selker RG, Fine HA, Black PM, Loeffler JS and Linet
MS: Cellular-telephone use and brain tumors. N Engl J Med.
344:79–86. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schoemaker MJ, Swerdlow AJ, Hepworth SJ,
van Tongeren M, Muir KR and McKinney PA: History of allergic
disease and risk of meningioma. Am J Epidemiol. 165:477–485. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Linos E, Raine T, Alonso A and Michaud D:
Atopy and risk of brain tumors: A meta-analysis. J Natl Cancer
Inst. 99:1544–1550. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
George M, Ikonomidis C, Pusztaszeri M and
Monnier P: Primary meningioma of the middle ear: case report. J
Laryngol Otol. 124:572–574. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rowland LP: Tumors of the
meningesMerritt's Neurology. 10th. Lippincott Williams and Wilkins;
Philadelphia, PA: pp. 250–253. 2000
|
|
13
|
Ozbayir T, Malak AT, Bektas M, Ilce AO and
Celik GO: Information needs of patients with meningiomas. Asian Pac
J Cancer Prev. 12:439–441. 2011.PubMed/NCBI
|
|
14
|
Thompson LD, Bouffard JP, Sandberg GD and
Mena H: Primary ear and temporal bone meningiomas: a
clinicopathologic study of 36 cases with a review of the
literature. Mod Pathol. 16:236–245. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pankhania M, Rourke T and Draper MR: The
middle ear mass: a rare but important diagnosis. BMJ Case Rep. Dec
2–2011.(Epub ahead of print). View Article : Google Scholar
|
|
16
|
Chang CY, Cheung SW and Jackler RK:
Meningiomas presenting in the temporal bone: the pathways of spread
from an intracranial site of origin. Otolaryngol Head Neck Surg.
119:658–664. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Batsakis JG: Pathology consultation.
Extracranial meningiomas. Ann Otol Rhinol Laryngol. 93:282–283.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hamilton BE, Salzman KL, Patel N, Wiggins
RH III, Macdonald AJ, Shelton C, Wallace RC, Cure J and Harnsberger
HR: Imaging and clinical characteristics of temporal bone
meningioma. AJNR Am J Neuroradiol. 27:2204–2209. 2006.PubMed/NCBI
|
|
19
|
Tsunoda R and Fukaya T: Extracranial
meningioma presenting as a tumour of the external auditory meatus:
a case report. J Laryngol Otol. 111:148–151. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Marosi C, Hassler M, Roessler K, Reni M,
Sant M, Mazza E and Vecht C: Meningioma. Crit Rev Oncol Hematol.
67:153–171. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rietz DR, Ford CN, Kurtycz DF, Brandenburg
JH and Hafez GR: Significance of apparent intratympanic
meningiomas. Laryngoscope. 93:1397–1404. 1983. View Article : Google Scholar : PubMed/NCBI
|