Introduction
Despite the ‘war on cancer’ propagated by the World
Health Organisation (WHO) and the US government in the 1980s,
cancer remains a serious threat to health worldwide, particularly
in Western countries (1). While the
number of cases of certain types of cancer, such as
gastrointestinal cancer, have declined, others such as breast
cancer are on the rise. As a result, cancer is the second most
common cause of premature mortality in Western countries and the
third most common worldwide (2). In
2014, the WHO predicted that the incidence of cancer will
approximately duplicate over the proceeding 2 decades. It also
estimated that ≥30% of those cases are preventable through public
health strategies to combat the leading causes, the most notable of
which are a high body mass index (BMI), a diet lacking natural
antioxidants and the abuse of alcohol and tobacco (3). This brings dietary interventions into
focus for the prevention and possible treatment of cancer (4,5). Although
extensive studies and resources have been invested into cancer
research and diagnosis, the survival rates have barely altered for
certain types of cancer (6–9).
In recent years, attention was drawn to the fact
that diet-associated factors may be involved in the development and
progression of cancer. The Harvard Alumni Health Study demonstrated
an association between low BMI at early adulthood and late
mortality from cancer, with an increased risk of 11% for each
standard deviation unit of increased BMI at 18 years of age. This
association was valid regardless of the tumour site (10). The European Prospective Investigation
into Cancer and Nutrition Study observed a 36% reduction in the
risk of cancer mortality for people living a healthy lifestyle,
which included exercise, maintaining a healthy weight, no smoking
and following a healthy diet (11).
This reduction was higher for specific types of cancer (12). According to Donaldson (13) and Bao et al (14), the consumption of foods rich in
antioxidants and healthy combinations of fats and carbohydrates
such as nuts may protect against cancer mortality.
Therefore, it is not surprising that in recent
years, the potential of a ketogenic diet as an adjunct to standard
cancer care has raised interest among researchers. In a ketogenic
diet, the energy requirements of the organism are met by a diet
rich in proteins and fats with comparatively few carbohydrates,
normally in a ratio of 3 parts fats and proteins to ≤1 part
carbohydrates (3,15). This is a nutritional approach that
mimics physiological fasting, which may be beneficial in the
treatment of cancer, if it is moderate and not prolonged, as
suggested by animal models and clinical experience (16). During fasting, the body converts
triglycerides from fat stores into ketone bodies, including
acetoacetate, acetone and β-hydroxybutyrate, which can be used as
an energy supply by the majority of cells, including muscle cells
and neurons (15). For those cells
that require sugar, gluconeogenesis can generate sugar de
novo from the glycerol that is produced during lipolysis, and
thus, the levels of sugar in blood stay within the normal range
during ketosis (4,15). It is noteworthy that a therapeutic
ketogenic diet is physiologically close to the ‘paleolithic diet’
that is currently discussed as potentially beneficial for weight
loss (17–19). A ketogenic diet has been demonstrated
to be therapeutically useful for the treatment of epilepsy
(15) and cardiovascular diseases
(4).
In 1924, Otto Warburg discovered that cancer cells
can generate energy from sugar without oxidation, regardless of the
presence of oxygen, and named this phenomenon ‘aerobic glycolysis’
(20,21). Glycolysis is an inefficient way to
generate energy, since it converts 1 glucose molecule into 2
molecules of pyruvate, and the energy released is then used to
produce 2 molecules of ATP, whereas through oxidation the yield of
1 molecule of glucose is ~38 molecules of ATP (22,23).
Glycolysis is present in primitive organisms such as bacteria that
can exist without oxygen, and is possibly one of the oldest
mechanisms providing organisms with energy (24). Glycolysis is used by human cells and
neurons (25) under high stress or
anaerobic conditions (26). Cells
normally oxidise sugar because it provides them with more energy
than glycolysis does, but, in contrast to glycolysis, oxidation
produces free radicals that must be buffered, since they may damage
cells and cellular structures. This is the rationale behind
numerous cancer treatments that increase oxidative stress (26). Warburg hypothesized that cancer cells
switch to glycolysis, as their mitochondria are dysfunctional.
However, this was demonstrated to be wrong, and in consequence,
Warburg's hypothesis was rejected (27). A more modern and enlightened view
proposes that cancer cells switch to glycolysis, despite oxygen
being present, as they can thereby escape the apoptotic mechanisms
that are induced by free radicals (23,26,28), and
it facilitates the incorporation of other components necessary for
cell growth (22). However, this
process creates a heavy demand on glucose supply, since the growth
of cancer cells exclusively occurs if there is enough glucose
provision. Furthermore, cancer cells appear to be able to use
ketone bodies for energy production under certain restricted
conditions, and solely if enough oxygen is present, which is not
the case at those sites where the tumour grows rapidly (29,30). Thus,
depriving cancer cells of glucose may reinstate apoptosis in cancer
cells (31). Furthermore, high
fasting insulin levels that lead to insulin resistance has been
associated with a 2.4-fold risk of developing breast cancer in
post-menopausal women (32).
Therefore, the use of a ketogenic diet as a supportive strategy for
patients with tumours is a rational and empirically supported
approach. This type of diet provides daily ~1 g carbohydrates/kg
body weight (28,33), combined with unsaturated fatty acids,
particularly Ω-3, short- and medium-chain fatty acids. A good
supply of plant-derived antioxidants, such as polyphenols, and a
lactate drink to buffer acidity are also important. Brochures and
books regarding the use of ketogenic diet for patients with cancer
have been available in Germany for several years (34,35).
The transketolase-like-1 (TKTL1) gene was identified
as a mutation of the transketolase gene. The TKTL1 enzyme and its
associated proteins have been associated with switching the cell
into aerobic glycolysis as a secondary pathway to generate energy
(36,37). TKTL1 seems to boost the glucose
metabolism of cancer cells (38), and
its activity has been associated with anaerobic glycolysis in
cancer cells and with low survival rates (39). By contrast, the inhibition of TKTL1
expression has been observed to be associated with reduced
proliferation in a hepatoma cell model (40). Previous studies have demonstrated that
TKTL1 is an independent oncogenic marker, possibly associated with
an enhanced glucose metabolism, and that increased serum levels of
TKTL1 are associated with the recurrence of cancer in patients with
oral squamous cell carcinoma, breast cancer and prostate cancer
(39,41–43). TKTL1
can be reliably measured using a novel immunological assay, termed
the epitope detection in monocyte (EDIM) test, with 94% sensitivity
and 82% specificity. The EDIM test presents a positive predictive
value of 87%, and correlates 90% with the current standard
procedure, a positron emission tomography (PET) scan to measure
radioactive glucose incorporation into cancer cells (44). In one clinical case, it was observed
that the levels of TKTL1 were increased in a patient following
resection of colon cancer, and prior to the appearance of
clinically visible metastases, thus demonstrating the practical use
and sensitivity of TKTL1 as a marker (45). Although negative findings have also
been reported (46), collectively,
these observations indicate that TKTL1 may act as a genetic switch,
enabling cancer cells to perform aerobic glycolysis in order to
meet their increased demand on glucose supply required for
proliferation. In addition, Apo10 overexpression has been detected
in different types of tumors. It is assoctiated with the inhibition
of of apoptosis and is indicative of abnormal cell proliferation.
As of 2010, it has also been possible to measure Apo10 levels using
the EDIM blood test (47).
It is plausible to assume that a ketogenic diet
operates on this basis, and therefore bears certain promise.
Previous pilot and feasibility trials have established the
potential of a ketogenic diet as supportive treatment against
cancer. In a small pilot study with 16 patients with cancer, the
ketogenic diet was accepted well by 9 patients, and 5 of them
completed the study. In those 5 patients who were able to adhere to
the diet, the disease was stable without further progress, and
their emotional function and sleep improved (33). In a small feasibility study in 10
patients with advanced cancer, 4 patients were unable to adhere to
the diet, and 5 of those that were able to follow the 4-week diet
reached physiological ketosis and experienced a remission or a
retardation of progression of the disease. In these patients, the
level of ketosis was significantly associated with reduced insulin
levels (48). In another study, 20
patients with recurrent glioblastoma were administered a ketogenic
diet (50). Those who reached ketosis
experienced slower tumour progression. Overall, the diet was well
received, although the blood sugar levels did not reduce as
markedly as was anticipated, which was assumed by the authors to be
due to steroid treatment. Taken together, these results are
encouraging, and require further confirmation in larger randomised
studies.
However, general practitioners, who have the task of
caring for patients once standard tumour treatment has been
provided, are frequently challenged by patients who want to
contribute to the maintenance of a tumour-free status or avoid
recurrence or metastatic development. Often, these patients possess
a certain notion of the ketogenic diet, instilled by popular
literature. In the present study, the effects of a ketogenic diet
in a prospective cohort of tumour patients in general practice was
studied in order to evaluate whether the levels of TKTL1 are
associated with tumour status and progression, and are affected by
a ketogenic diet, and whether adherence to a ketogenic diet is
associated with a better prognosis in patients with cancer.
Materials and methods
Patient cohort
The present study was designed as a systematic,
prospective cohort study in general practice. A total of 78
patients that had been diagnosed with any type of cancer since
January 2001 were eligible for the study. The patients were
examined in the private practice clinic of Heilbronn
(Baden-Württemberg, Germany) between November 2010 and December
2011. The patients were screened and included in the present
observational study if they had been diagnosed with any type of
tumour, or had experienced the recurrence of a tumour or
metastasising disease during the 10 years previous to the
initiation of the study. There were no exclusion criteria. For all
patients, except 1 that declined testing, the levels of TKTL1 were
measured using the EDIM test, according to previously published
procedures (44,45), and controlled every ~3 months. The
patients were followed-up in general practice until the end of
2011.
Treatment and patient follow-up
For the corresponding analyses, 3 ml venous blood
was extracted and preserved in a vial containing EDTA. Blood
samples were stored at room temperature and sent by courier to the
laboratory (Biovis Diagnostik MVZ GmbH, Limburg an der Lahn,
Germany), where they were processed within 24 h. The recommended
precautions were followed, including not testing during
immunosuppressive therapy with antibiotics or cortisone, or during
the 4 weeks subsequent to surgery, chemotherapy or radiation
therapy. Patients were instructed regarding the potential benefit
of a ketogenic diet, particularly those patients whose TKTL1 levels
were above the standard laboratory norms. For ease of
implementation, patients were informed about the company Tavarlin
(Frankfurt, Germany), which specialises in producing and mailing
food that meets the requirements of a ketogenic diet, including
oil, fat, snacks, bread, protein and energy drinks (35). Every 3 months, the patients were
questioned regarding their eating habits in a clinical interview,
and classified accordingly into 3 different groups (no ketogenic
diet; partially ketogenic diet; or strict ketogenic diet),
following a conservative criteria of classification: If the
patients adhered fully to a ketogenic diet, they were classified as
fully ketogenic. If they adhered partially to a ketogenic diet, or
switched during the observational period from no ketogenic diet to
ketogenic diet or vice versa, they were classified as
partially ketogenic. All other patients were classified as not
ketogenic.
Patients were also distributed, using their
oncologists' reports, into the following categories: Preoperative;
curative; palliative with improvement; palliative with stable
disease; or palliative with progressing disease. As certain
categories contained very few patients, the preoperative and
curative categories were collapsed into curative, palliative with
improvement and palliative with stable disease were collapsed into
palliative, and palliative with progressing disease was renamed
endstage.
The variation in TKTL1 scores was calculated from
the end of the observation period to baseline. Thus, negative
scores corresponded to a reduction in TKTL1 values, while positive
scores represented an increase over time. Patients were then
grouped according to the following criteria: Those patients that
did not initiate a ketogenic diet or returned to their ordinary
diet; those that adhered partially to a ketogenic diet; and those
that completely embraced a ketogenic diet. Patients were
categorised according to their variation in tumour status from the
beginning to the end of the observation period, by subtracting the
initial category from the last one available. Thus, a negative
score indicated an improvement in tumour status over time (for
example, from palliative with progress to palliative stable, or
from palliative to curative), while a positive score corresponded
to a deterioration of the disease. All the categories of
deterioration were collapsed into 1 category to facilitate the
analysis and representation of the results.
Statistical analysis
Robust non-parametric, descriptive statistics and
graphical analysis were used to display the data. Yates' correction
for continuity was applied to tables with small cells. Statistical
analyses were performed using Statistica software, version 8
(StatSoft, Ltd., Bedford, UK). Due to the absence of systematic
knowledge from previous studies, all data, tests and significances
in the present study must be interpreted with caution, and
considered as orienting and exploratory. P<0.05 was considered
to indicate a statistically significant difference.
Results
Correlation between TKTL1 values,
patient adherence to ketogenic diet and disease progression
A total of 78 patients with different types of
tumours were included in the present study. The characteristics of
the patients, including age, gender, BMI, smoking habits, maximum
values of TKTL1 and Apo10, time since diagnosis, tumour stage, type
of cancer and adherence to a ketogenic diet, are presented in
Tables I and II. Maximum values of TKTL1 and Apo10 were
determined by measuring every 3 months, and the maximum value was
selected as the cancer is considered to be most aggressive at this
point.
 | Table I.Description of the patient
cohort. |
Table I.
Description of the patient
cohort.
| A, Variables
measured during the patients follow-up |
|
|
|---|
|
|---|
| Variable | Mean ± standard
deviation | Range |
|---|
| Age (years) | 68.3±13.1 | 21.0–92.0 |
| Time since
diagnosis (years) | 6.5±5.8 |
1.0–25.0 |
| Body mass
index | 24.4±4.6 | 16.3–36.7 |
| TKTL1 max | 150.83±44.90 |
98.0–323.0 |
| Apo10 max | 15.9±17.2 |
9.0–66.6 |
| Smoking habits
(pack years) | 16.32±25.30 |
0–120 |
| Number of
sessions | 4.02±2.80 |
1.0–19.0 |
| Duration between
sessions (days) | 163.26±136.10 |
31–684 |
|
| B, Characteristics
of the patients |
|
| Characteristic
(n=78) | Frequency | Percentage (%) |
|
| Gender |
|
|
|
Female | 35 | 44.90 |
|
Male | 43 | 55.10 |
| Smoking habits
(pack years) |
|
|
| 0 | 31 | 43.66 |
|
1–20 | 22 | 30.98 |
|
21–40 | 7 |
9.85 |
|
41–60 | 9 | 11.26 |
|
61–120 | 3 |
4.20 |
| Missing
data | 7 |
9.80 |
| Tumour status |
|
|
|
Curative | 56 | 71.80 |
|
Palliative/lethal | 22 | 28.20 |
| Type of cancer |
|
|
|
Breast | 18 | 23.10 |
|
Prostate | 16 | 20.51 |
|
Colon | 9 | 11.53 |
|
Melanoma | 2 |
2.56 |
|
Lung | 5 |
6.41 |
|
Otolaryngeal | 5 |
6.41 |
|
Other | 23 | 29.48 |
| Diet during the
observation period |
|
|
| Not
ketogenic | 65 | 83.33 |
|
Partially ketogenic | 6 |
7.69 |
| Fully
ketogenic | 7 |
8.97 |
 | Table II.Number and percentage of patients
with different stages of cancer that adopted a ketogenic diet. |
Table II.
Number and percentage of patients
with different stages of cancer that adopted a ketogenic diet.
| Diet | Curative stage, n
(%) | Palliative stage, n
(%) | Endstage, n
(%) | Total, n (%) |
|---|
| Not ketogenic | 50 (74) | 9 (11) | 6 (8) | 65 (83) |
| Partially
ketogenic | 3 (4) | 2 (2) | 1 (1) | 6 (8) |
| Fully
ketogenic | 3 (4) | 4 (5) | 0 (−) | 7 (9) |
| Total | 56 (72) | 15 (19) | 7 (9) | 78
(100) |
Of the 78 patients included in the study, 18
presented with breast cancer, 16 with prostate cancer, 9 with colon
cancer, 2 with melanoma, 5 with lung cancer, 5 with
otolaryngological cancer and 23 with other types of cancer. In
these patients, 56 (72%) cases were classified as being at a
curative stage, 15 (19%) at a palliative stage, and 7 (9%) at an
endstage. The correlations between the maximum values of TKTL1 and
Apo10, tumour stage and adherence to a ketogenic diet are displayed
in Table III.
 | Table III.Nonparametric (Spearman's rank)
correlations between TKTL1 max, Apo10 max, type of diet (no,
partially or fully ketogenic) and the tumour stage (curative,
palliative or endstage). |
Table III.
Nonparametric (Spearman's rank)
correlations between TKTL1 max, Apo10 max, type of diet (no,
partially or fully ketogenic) and the tumour stage (curative,
palliative or endstage).
|
Characteristics | TKTL1 max | Apo10 max | Ketogenic diet |
|---|
| Tumour status | 0.47a | 0.32a | 0.26a |
| TKTL1 max | – | 0.34a | 0.33a |
| Apo10 max | – | – | 0.08 |
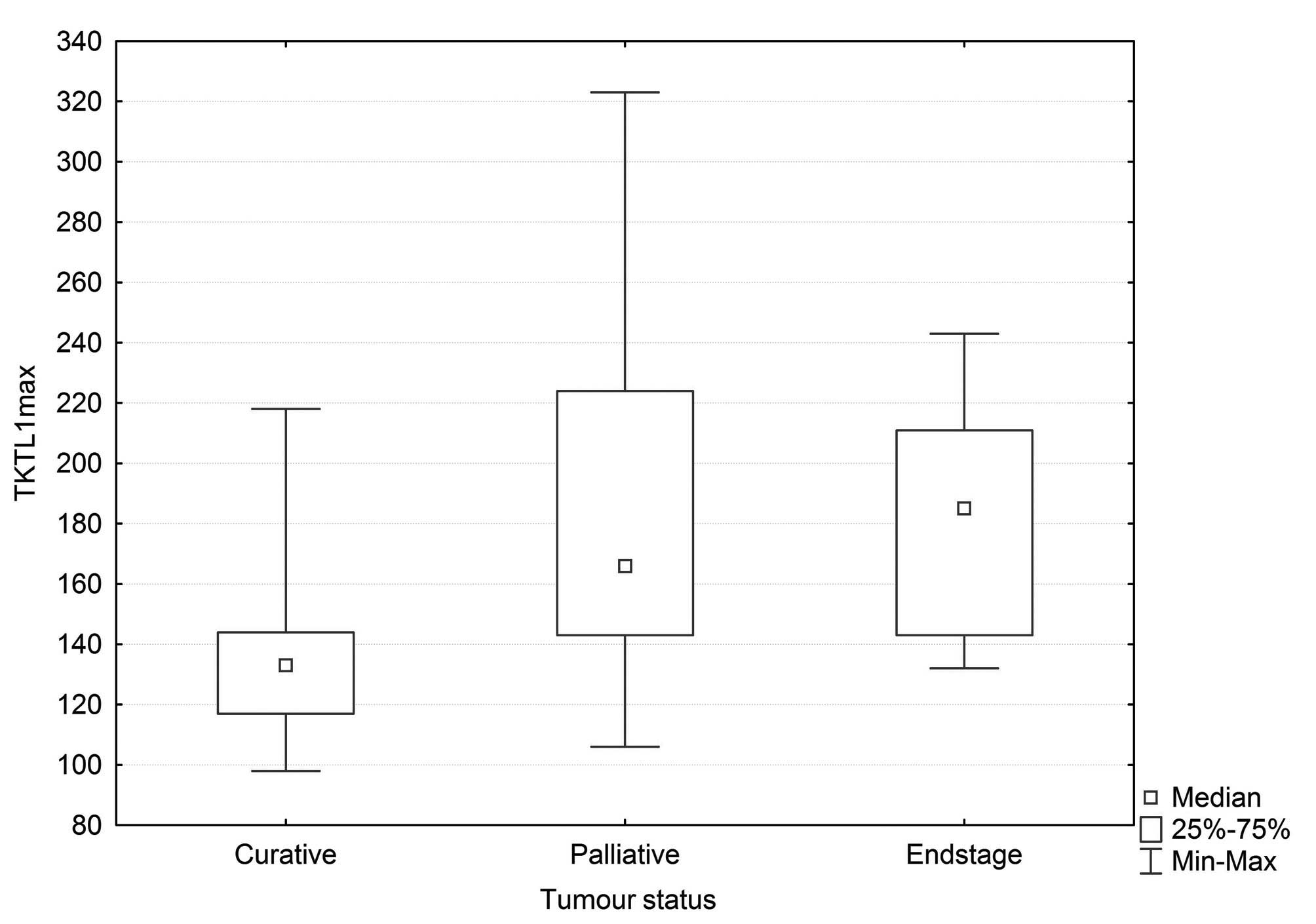
The distribution of TKTL1 values across the 3 groups
of tumour stages is presented in Fig.
1. Significant differences were observed between these groups
(Kruskal-Wallis, P=0.0002). Since the levels of TKTL1 depend on the
activity of the immune system, which is often dysfunctional in
late-stage cancer, the levels of TKTL1 were comparatively low in
endstage patients, although the general trend was still visible.
Fig. 2 presents the distribution of
TKTL1 values according to the type of diet. Significant differences
between the groups were observed (Kruskal-Wallis, P=0.0045).
Of the 78 patients, 13 (17%) had adopted a ketogenic
diet, 6 of them partially (8%) and 7 in full (9%). As indicated in
Table II, none of the patients in
endstage cancer adopted the diet fully, and 1 patient adhered
partially to it. Of the 4 palliative patients that adopted a strict
ketogenic diet, 1 patient with metastatic breast cancer, who had
embraced a strict ketogenic diet since 2009, experienced a full
remission of all metastases in the lung and bones. This was
verified by fludeoxyglucose-PET analysis, which demonstrated no
active metastases and 1 inactive metastasis in the thoracic region
of the spine. In another palliative patient, who was diagnosed with
cancer of the ovary in 1996 and had previously experienced cancer
of the left and right breast in 1987 and 1998, respectively,
followed by a recurrence of the carcinoma on the left side in 2006
and another recurrence in 2009, no further recurrences were
detected during the observation period. A third patient with
astrocytoma experienced a progression of the disease despite the
ketogenic diet, although the high-dose corticosteroid therapy that
the patient had received may have impacted their glucose
metabolism. The fourth patient who adhered to a ketogenic diet did
not undergo follow-up testing. Those patients who had started on a
strict ketogenic diet, but then stopped it, experienced initially a
remission of the disease or the metastases, which rebounded once
they had stopped the diet, frequently with lethal consequences. A
breakdown of the numbers of patients with modifications in diet by
alteration in tumour status is displayed in Table IV. As indicated in the table, a
correlation was observed between an improvement of the disease and
having adopted the ketogenic diet in full (χ2=33.26;
df=4; P=0.00001). Fig. 3 demonstrates
that a reduction in TKTL1 score from baseline to the final
measurement was associated with ketogenic diet and improvement in
cancer status. It should be noted that, due to the insufficient
number of cases available for statistical evaluation, this
association is simply displayed for visual inspection.
 | Table IV.Number of patients who modified their
diet and experienced a variation in tumour status over time. |
Table IV.
Number of patients who modified their
diet and experienced a variation in tumour status over time.
| Diet | Improvement | No alteration | Worsening | Total |
|---|
| Not ketogenic | 1 | 56 | 10 | 67 |
| Switch to partial
ketogenic diet | 0 | 5 | 1 | 6 |
| Switch to full
ketogenic diet | 3 | 2 | 0 | 5 |
| Total | 4 | 63 | 11 | 78 |
Statistical analysis
In a logistic regression analysis, with endstage and
palliative stage collapsed into 1 category, and where cancer stage
was considered to be the dependent variable, whereas the value of
TKTL1 and the adherence to a ketogenic diet were treated as the
independent variables, the influence of these variables was
estimated. The model was observed to be significant (χ2,
22.7; P=0.00001), with a parameter estimate for TKTL1 of −0.034
(95% CI=-0.014 to −0.054; P=0.001) and OR=0.96 (95% CI=0.95–0.99)
for the unit variation, which implies that for every 0.034 unit
reduction in TKTL1 values there is a 4% probability of improvement
in tumour status, from palliative or lethal to curative stage.
Other variables, including the duration of diagnosis or the maximum
values of Apo10, were not significant predictors.
Discussion
To the best of our knowledge, the present study is
the first to describe the effects of a ketogenic diet in patients
with cancer in primary care. All patients who presented in a
primary care clinic with cancer were documented, and the adherence
to a ketogenic diet and the variation in status of the tumour were
monitored. The levels of TKTL1 were measured continuously in the
patients. TKTL1 is a novel marker that is supposedly associated
with tumour progression and switching of the tumour cells to
aerobic glycolysis (49). The results
from the present study support the following conclusions: i) TKTL1
is associated with a more active disease and a worse prognosis; ii)
a ketogenic diet reduces the levels of TKTL1; and iii) increased
levels of TKTL1 predict the development of endstage disease.
In view of the biochemical knowledge discussed in
the present report, and the preliminary findings from previous
studies, it can be proposed that patients with a diagnosis of
cancer (except those with endstage disease) can adopt a ketogenic
diet and benefit from it, since those patients who embraced a
ketogenic diet in the present study were observed to experience a
halt in the progression of the disease or complete remission.
Nonetheless, these results should be viewed with the
appropriate caution, since they derive from a cohort of patients in
primary care, which implies that, despite being treated to the best
current oncological standards (which are high in Germany), patients
who are disease-free often suffer from metastases or recurrences,
as was the case in a number of patients in the present cohort. In
addition, patients frequently want to know whether they can
contribute to their health or boost their immune system. Thus, if
they are informed that no alternative treatment is available other
than waiting for a potential recurrence, patients are likely to
consult with different practitioners (51). By contrast, offering the patients a
diet which is comparatively natural and can be implemented by
themselves strengthens their self-efficacy and expectancy of
success, which, based on the current knowledge, may be an important
variable in non-specific therapeutic effectiveness (52–56).
The present study was not a randomised study, but a
study in general practice. The patients are likely to be
representative of patients with cancer in the general population,
since the clinic participates in the statutory German reimbursement
system. However, since there is no control condition or control
group matched for important predictors, it is difficult to preclude
that the effects observed are not confounded. In fact, they
possibly are, since patients with more progressed disease are less
likely to adhere to the diet. Thus, the next important step would
be to launch a large-scale randomised study to validate the effects
of a ketogenic diet in the treatment of cancer.
In the present study, patients were offered the
ketogenic diet that is provided by a company for ease of
implementation, but this is not a requirement. Self-help books and
brochures with recipes regarding ketogenic diet are available
(34,35), and certain patients may favour a more
vegetarian type of ketogenic diet, which was not the focus of the
current study (4,57,58).
One of the aims of the present study was to
investigate the effects of the novel marker TKTL1, which has been
hypothesised to be a marker of switching of cells, particularly
cancer cells, into a metabolic mode whereby they use glycolysis
rather than oxidation for energy supply, in order to protect
themselves from free radicals and to foster growth under anaerobic
conditions such as those experienced by tumours growing at distant
sites (36). While the present study
was not intended to validate this hypothesis, the results obtained
suggest that there is a positive link between the expression of
TKTL1 and cancer progression, and a negative link between ketogenic
diet and TKTL1 expression. This also explains why a ketogenic diet
may be useful in patients with cancer, since cancer cells rarely
use or are unable to use ketone bodies. Thus a ketogenic diet would
withdraw the nutrients and energy requirements of a growing tumour,
but not of the physiological functioning of the body. Therefore,
reduced expression levels of TKTL1, which are a negative predictor
of cancer progression, may reflect the effect of a ketogenic diet.
To the best of our knowledge, the use of the EDIM test for
detecting and measuring TKTL1 is not widespread. However, since the
measurement is standardised, it may be useful to adopt the EDIM
test more commonly as a predictor of disease processes where a
ketogenic diet may be beneficial. In the present study, the
correlation between ketogenic diet and TKTL1 was observed to be
moderate in size and significant, explaining 22% of the common
variance. However, it should be noted that in endstage disease, the
marker loses its predictive value.
The positive correlation between ketogenic diet and
tumour stage observed in the current study is likely to be
artificial and due to the fact that more patients in a progressed
stage of the disease were willing to adopt the diet. Naturally,
they are also the patients who were most likely to benefit from it,
as the data in Table IV and Fig. 3 suggest. The length of time that the
diet needs to be maintained for is currently unknown. The present
study covers an observation period of ~2 years, and a number of
patients were able to follow the diet over the whole period.
Clinical experience teaches that it is beneficial to maintain a
ketogenic diet with active cancer (59,60).
The results of the present study regarding the
association between the modification of diet and the variation in
tumour status must be considered with caution, since the number of
observations for the majority of the variables reported is
insufficient to perform a reliable statistical analysis, and hence,
all the statistical estimations may be affected by error. Instead,
they are intended to be taken as guidance and to encourage further
research.
In summary, the present study has demonstrated that
a ketogenic diet is feasible and likely beneficial for patients
with cancer in primary care, who have been treated for their
primary cancer, since it altered the expression of TKTL1, a novel
and potentially useful marker to monitor the metabolic state of the
body regarding aerobic glycolysis, and to evaluate the potential
progression of non-endstage tumour disease. Therefore, the design
of rigorous randomised studies to validate these observations is
required.
Acknowledgements
The authors are grateful to Miss Majella Horan MSc,
the native speaker editor who improved the style of the manuscript.
The present study was a requirement of the PhD degree awarded to Dr
Natalie Jansen, who holds shares in Tavarlin, a company that offers
ketogenic products.
References
|
1
|
Sporn MB: The war on cancer. Lancet.
347:1377–1381. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cancer in Germany 2009/2010. (9th).
Contributions to the Health Reporting of the Federal Republic
(Berlin). Robert Koch Institut. 2013.(In German).
|
|
3
|
Cancer. Fact Sheet 297. Geneva: World
Health Organisation. 2014.
|
|
4
|
Paoli A, Rubini A, Volek JS and Grimaldi
KA: Beyond weight loss: A review of the therapeutic uses of
very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr.
67:789–796. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ornish D, Weidner G, Fair WR, Marlin R,
Pettengill EB, Raisin CJ, Dunn-Emke S, Crutchfield L, Jacobs FN and
Barnard RJ: Intensive lifestyle changes may affect the progression
of prostate cancer. J Urol. 174:1065–1070. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Berrino F, De Angelis R, Sant M, Rosso S,
Bielska-Lasota M, Coebergh JW and Santaquilani M: Eurocare Working
group: Survival for eight major cancers and all cancers combined
for European adults diagnosed in 1995–99: Results of the EUROCARE-4
study. Lancet Oncol. 8:773–783. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
De Angelis R, Sant M, Coleman MP,
Francisci S, Baili P, Pierannunzio D, Trama A, Visser O, Brenner H,
Ardanaz E, et al: EUROCARE-5 Working Group: Cancer survival in
Europe 1999–2007 by country and age: Results of EUROCARE-5 - a
population-based study. Lancet Oncol. 15:23–34. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hölzel D and Engel J: We cannot neglect
experiences from clinical practice. The example of metastasising
colon tumour shows how clinical registers can help contribute to
the evaluation of benefits of medications. Dtsch Arztebl.
109:A424–A425. 2012.(In German).
|
|
9
|
Schlesinger-Raab A, Eckel R, Engel J,
Sauer H, Löhrs U, Molls M and Hölzel D: Metastasising breast
cancer: No prolongation of life since 20 years. Dtsch Arztebl.
102:A2706–A2714. 2005.(In German).
|
|
10
|
Gray L, Lee IM, Sesso HD and Batty GD:
Association of body mass index in early adulthood and middle age
with future site-specific cancer mortality: The Harvard Alumni
Health Study. Ann Oncol. 23:754–759. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ford ES, Bergmann MM, Kröger J,
Schienkiewitz A, Weikert C and Boeing H: Healthy living is the best
revenge: Findings from the European Prospective Investigation Into
Cancer and Nutrition - Potsdam study. Arch Intern Med.
169:1355–1362. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gonzalez CA and Riboli E: Diet and cancer
prevention: Contributions from the European Prospective
Investigation into Cancer and Nutrition (EPIC) study. Eur J Cancer.
46:2555–2562. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Donaldson MS: Nutrition and cancer: A
review of the evidence for an anti-cancer diet. Nutrit J.
20:192004.
|
|
14
|
Bao Y, Han J, Hu FB, Giovannucci EL,
Stampfer MJ, Willett WC and Fuchs CS: Association of nut
consumption with total and cause-specific mortality. N Engl J Med.
369:2001–2011. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ruskin DN and Masino SA: The nervous
system and metabolic dysregulation: Emerging evidence converges on
ketogenic diet therapy. Front Neurosci. 6:332012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fontana L and Klein S: Aging, adiposity,
and calorie restriction. JAMA. 297:986–994. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Henderson ST: High carbohydrate diets and
Alzheimer's disease. Med Hypotheses. 62:689–700. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Eaton SB and Konner M: Paleolithic
nutrition: A consideration of its nature and current implications.
N Engl J Med. 312:283–289. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mellberg C, Sandberg S, Ryberg M, Eriksson
M, Brage S, Larsson C, Olsson T and Lindahl B: Long-term effects of
a papaeolithic-type diet in obese postmenopausal women: A 2-year
randomized trail. Eur J Clin Nutr. 68:350–357. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Warburg O, Posener K and Negelein E: On
tumour metabolism. Biochem Z. 152:319–344. 1924.(In German).
|
|
21
|
Zhivotovsky B and Orrenius S: The Warburg
Effect returns to the cancer stage. Semin Cancer Biol. 19:1–3.
2009.(Editorial). View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Van der Heiden MG, Cantley LC and Thompson
CB: Understanding the Warburg effect: The metabolic requirements of
cell proliferation. Science. 324:1029–1033. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Garber K: Energy boost: The Warburg effect
returns in a new theory of cancer. J Natl Cancer Inst.
96:1805–1806. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Romano AH and Conway T: Evolution of
carbohydrate metabolic pathways. Res Microbiol. 147:448–455. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Newington JT, Pitts A, Chien A, Arseneault
R, Schubert D and Cumming RC: Amyloid β resistance in nerve cell
lines is mediated by the Warburg effect. PLoS One. 6:e191912011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gogvadze V, Zhivotovsky B and Orrenius S:
The Warburg effect and mitochondrial stability in cancer cells. Mol
Aspects Med. 31:60–74. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Weinhouse S: The Warburg hypothesis fifty
years later. Z Krebsforsch Klin Onkol. 87:115–126. 1976. View Article : Google Scholar
|
|
28
|
Holm E and Kämmerer U: Fat and
carbohydrates in diets for tumour patients. Aktuel Ernahrungsmed.
36:286–298. 2011.(In German). View Article : Google Scholar
|
|
29
|
Klement RJ and Kämmerer U: Is there a role
for carbohydrate restriction in the treatment and prevention of
cancer? Nutr Metab (Lond). 8:752011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Otto C, Klingelhöffer C, Biggemann L,
Melkus G, Mörchel P, Jürgens C, Gahn S and Kämmerer U: Experimental
studies on the metabolism of keton bodies and lactate by tumour
cells of the gastrointestinal duct. Aktuel Ernahrungsmed. 39:51–59.
2014.(In German).
|
|
31
|
Vaughn AE and Deshmukh M: Glucose
metabolism inhibits apoptosis in neurons and cancer cells by redox
inactivation of cytochrome c. Nat Cell Biol. 10:1477–1483. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gunter MJ, Hoover DR, Yu H,
Wassertheil-Smoller S, Rohan TE, Manson JE, Li J, Ho GY, Xue X,
Anderson GL, et al: Insulin, insulin-like growth factor-I, and risk
of breast cancer in postmenopausal women. J Natl Cancer Inst.
101:48–60. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Schmidt M, Pfetzer N, Schwab M, Strauss I
and Kämmerer U: Effects of a ketogenic diet on the quality of life
in 16 patients with advanced cancer: A pilot trial. Nutr Metab
(Lond). 8:542011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kämmerer U: Ketogenic diet for cancer
patients. Würzburg, Germany: The University Hospital Würzburg.
2010.(In German).
|
|
35
|
Coy JF and Franz M: The new anti-cancer
diet: How you can stop the cancer gene. 1:(1st). Munich: Gräfe und
Unzer. 2009.
|
|
36
|
Coy JF, Dressler D, Wilde J and Schubert
P: Mutations in the transketolase-like gene TKTL1: Clinical
implications for neurodegenerative diseases, diabetes and cancer.
Clin Lab. 51:257–273. 2005.PubMed/NCBI
|
|
37
|
Langbein S, Zerilli M, Zur Hausen A,
Staiger W, Rensch-Boschert K, Lukan N, Popa J, Ternullo MP,
Steidler A, Weiss C, et al: Expression of transketolase TKTL1
predicts colon and urothelial cancer patient survival: Warburg
effect reinterpreted. Br J Cancer. 94:578–585. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sun W, Liu Y, Glazer CA, Shao C, Bhan S,
Demokan S, Zhao M, Rudek MA, Ha PK and Califano JA: TKTL1 is
activated by promoter hypomethylation and contributes to head and
neck squamous cell carcinoma carcinogenesis through increased
aerobic glycolysis and HIF1α stabilization. Clin Cancer Res.
16:857–866. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Schwaab J, Horisberger K, Ströbel P, Bohn
B, Gencer D, Kähler G, Kienle P, Post S, Wenz F, Hofmann WK, et al:
Expression of Transketolase like gene 1 (TKTL1) predicts
disease-free survival in patients with locally advanced rectal
cancer receiving neoadjuvant chemoradiotherapy. BMC Cancer.
11:3632011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang S, Yang JH, Guo CK and Cai PC: Gene
silencing of TKTL1 by RNAi inhibits cell proliferation in human
hepatoma cells. Cancer Lett. 253:108–114. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Grimm M, Schmitt S, Teriete P, Biegner T,
Stenzl A, Hennenlotter J, Muhs HJ, Munz A, Nadtotschi T, König K,
et al: A biomarker based detection and characterization of
carcinomas exploiting two fundamental biophysical mechanisms in
mammalian cells. BMC Cancer. 13:5692013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kayser G, Sienel W, Kubitz B, Mattern D,
Stickeler E, Passlick B, Werner M and Zur Hausen A: Poor outcome in
primary non-small cell lung cancers is predicted by transketolase
TKTL1 expression. Pathology. 43:719–724. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lange C, Tisch-Rottensteiner J, Böhringer
D, Martin G, Schwartzkopff J and Auw-Haedrich C: Enhanced TKTL1
expression in malignant tumors of the ocular adnexa predicts
clinical outcome. Ophthalmology. 119:1924–1929. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Feyen O, Coy JF, Prasad V, Schierl R,
Saenger J and Baum RP: EDIM-TKTL 1 blood test: A noninvasive method
to detect upregulated glucose metabolism in patients with
malignancies. Future Oncol. 8:1349–1359. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Jansen N and Coy JF: Diagnostic use of
epitope detection in monocytes blood test for early detection of
colon cancer metastasis. Future Oncol. 9:605–609. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Mayer A, Von Wallbrunn A and Vaupel P:
Glucose metabolism of malignant cells is not regulated by
transketolase-like (TKTL)-1. Int J Oncol. 37:265–271. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Rotmann AR, Hofmann HA and Coy JF: Apo10 -
a new biomarker for early detection of disorders of cell
proliferation and solid tumours. Abstracts of XX FIGO World
Congress of Gynecology and Obstetrics. Int J Gynecol Obstet.
119(Suppl 3): S4662012. View Article : Google Scholar
|
|
48
|
Fine EJ, Segal-Isaacson CJ, Feinman RD,
Herszkopf S, Romano MC, Tomuta N, Bontempo AF, Negassa A and
Sparano JA: Targeting insulin inhibition as a metabolic therapy in
advanced cancer: A pilot safety and feasibility dietary trial in 10
patients. Nutrition. 28:1028–1035. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wanka C, Steinbach JP and Rieger J:
Tp53-induced glycolysis and apoptosis regulator (TIGAR) protects
glioma cells from starvation-induced cell death by up-regulating
respiration an dimproving cellular redox homeostasis. J Biol Chem.
287:33436–33446. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Rieger J, Bähr O, Maurer GD, Hattingen E,
Franz K, Brucker D, Walenta S, Kämmerer U, Coy JF, Weller M and
Steinbach JP: ERGO: A pilot study of ketogenic diet in recurrent
glioblastoma. Int J Oncol. 44:1843–1852. 2014.PubMed/NCBI
|
|
51
|
Guethlin C, Walach H, Naumann J, Bartsch
HH and Rostock M: Characteristics of cancer patients using
homeopathy compared with those in conventional care: A
cross-sectional study. Ann Oncol. 21:1094–1099. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Segar J: Complementary and alternative
medicine: Exploring the gap between evidence and usage. Health
Lond. 16:366–381. 2012.
|
|
53
|
Walach H: Spiritual and alternative cancer
therapies: Strange theories, perhaps wrong, but useful. Breast Care
(Basel). 2:190–192. 2007. View Article : Google Scholar
|
|
54
|
Chvetzoff G and Tannock IF: Placebo
effects in oncology. J Natl Cancer Inst. 95:19–29. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Walach H: Placebo effects in Complementary
and Alternative Medicine: The selfhealing response. Placebo and
Pain: From Bench to Bedside (Amsterdam). Elsevier-Academic Press.
189–202. 2013. View Article : Google Scholar
|
|
56
|
Walach H: Placebo controls: Historical,
methodological and general aspects. Philos Trans R Soc London B
Biol Sci. 366:1870–1878. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Fontana L, Partridge L and Longo VD:
Extending healthy life span - from yeast to humans. Science.
328:321–326. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Mutter J: Healthy instead of chronically
ill! The holistic path: prevention instead of treatment. Fit fürs
Leben Verlag (Weil der Stadt). 2009.(In German).
|
|
59
|
Ho V, Leung K, Hsu A, Luk B, Lai Jm Shen
SY, Minchinton AI, Waterhouse D, Bally MB, Lin W, et al: A low
carbohydrate, high protein diet slows tumor growth and prevents
cancer initiation. Cancer Res. 71:4484–4492. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Masko EM, Thomas JA, Antonelli JA, Lloyd
JC, Phillips TE, Poulton SH, Dewhirst MW, Pizzo SV and Freedland
SJ: Low-carbohydrate diets anmd prostate cancer: How low is ‘low
enough’? Cancer Prev Res (Phila). 3:1124–1131. 2010. View Article : Google Scholar : PubMed/NCBI
|