Introduction
Alveolar soft part sarcoma (ASPS) is a rare soft
tissue tumor that accounts for ~0.5–1.0% of all soft tissue
sarcomas (1). ASPS was first
described in 1952, and has rarely been reported since (2). ASPS involves several locations,
particularly muscles and deep soft tissues of the body (3). In adults, ASPS is often localized in the
lower extremities, while the head and neck are the predominant
sites for ASPS in children (4). Park
et al reported six cases of primary ASPS of bone in 1999,
and demonstrated the bone origin of this condition based on their
radiological findings (5). To date,
the number of published studies reporting cases of ASPS is limited
(3,6,7).
Primary lymphoma of bone (PLB) is an extranodal
lymphoma that arises from the medullary cavity and manifests as a
localized, solitary lesion (8). PLB
represents 3% of all primary malignant bone tumors, and 1% of all
malignant lymphomas (8). First
reported by Oberling in 1928 (9), PLB
has been described as a malignant, lymphoid infiltrate within bone,
with or without cortical invasion or soft tissue extension, and
without concurrent involvement of regional lymph nodes or distant
viscera (10). Non-Hodgkins lymphoma
constitutes the majority of PLBs, and the most common subtype is
diffuse large B-cell lymphoma (11,12), while
T-cell PLB is rare (13).
Second primary malignances (SPMs) are newly
developed malignant neoplasms that present synchronously or
metachronously in a patient with a known malignant disease
(14). The incidence of SPM is not
rare (15–18). However, a limited number of cases of
primary intraosseous ASPS and PLB have been reported in the
literature thus far. To the best of our knowledge, the present
report is the first case of intraosseous ASPS and PLB occurring
concomitantly in the same patient. Written informed consent was
obtained from the patient.
Case report
A 42-year-old woman presented to the Department of
Radiology of Zhongnan Hospital of Wuhan University (Wuhan, China)
with continuous pain in her right hip and occasional pain in her
left leg, in addition to dizziness and heart palpitations. The
patient had been experiencing these symptoms during the two months
prior to the date of admission to the hospital in June 2010.
The results of a blood routine test performed prior
to the date of admission suggested anemia, and the patient had been
receiving treatment for anemia during one month at her local
hospital, but the pain in her right hip worsened. Therefore, the
patient was referred to the Zhongnan Hospital of Wuhan University.
Physical examination identified a firm mass with a poorly
delineated margin that was palpable in the right hip. The left leg
examinations did not indicate any abnormalities. The red blood cell
count was 2.23×1012 cells/l, and the levels of
hemoglobin were 66.20 g/l. The patients initial pelvic radiograph
revealed a large right proximal femur osteolytic process with
cortical disruption (Fig. 1).
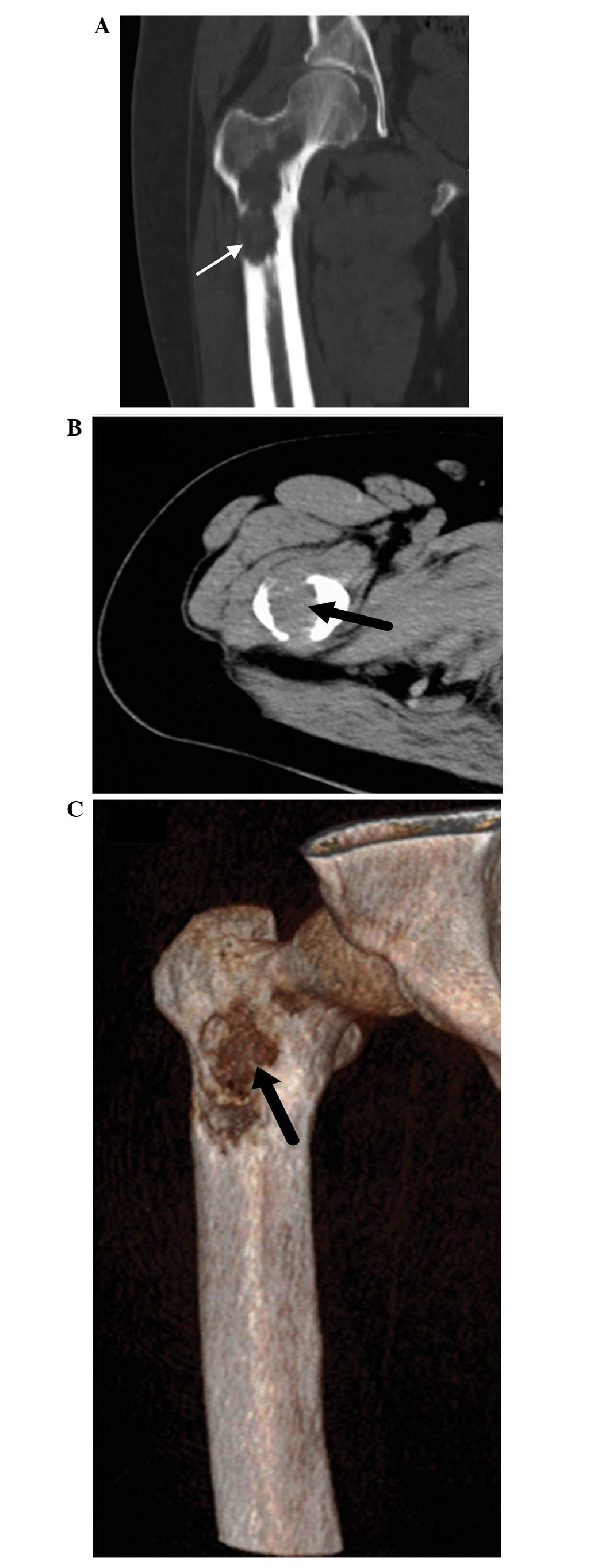
Computed tomography (CT) confirmed the presence of a large
non-matrix producing soft tissue lesion in the right proximal
femur, which was accompanied of cortical destruction, but did not
exhibit surrounding sclerosis or associated periosteal reaction
(Fig. 2).
Following tumor resection, the patient received bone
cement and was subjected to internal fixation. Microscopic
examination of the tumor specimen by hematoxylin and eosin stain
(ZSGB-BIO, Beijing, China) revealed proliferation of large
polygonal cells separated by thin fibrous septa. The cells
presented round nuclei, were disposed centrally, and contained
abundant granular eosinophilic cytoplasm. A small number of normal
mitoses were also observed (Fig. 3).
On immunohistochemistry, the tumor cells were diffusely positive
for myoglobin and cytokeratin, focally positive for Ki-67, and
negative for cluster of differentiation (CD)138, CD79a, CD20, CD3,
CD30, anaplastic lymphoma kinase and chromogranin A (CgA).
Consequently, the patient was diagnosed with ASPS of the right
proximal femur.
The patient initiated chemotherapy treatment with
adriamycin (A) and ifosfamide (I) at 20 days post-surgery. The AI
protocol consisted of 4-day administration of ifosfamide at a dose
of 3 g/m2, and 3-day administration of adriamycin at a
dose of 60 mg/m2. In addition, the patient received
adequate mesna for protection and hydration. The treatment was
effective in treating the symptoms, and the patient achieved IV
degree of bone marrow suppression. The second round of chemotherapy
started three weeks later, and following four weeks, the patient
accepted radiotherapy with total doses of 60 Gy/200 cGy/30
fraction/40 day. During this period, the patient complained of
persistent pain in the left leg.
The subsequent X-ray examination was normal
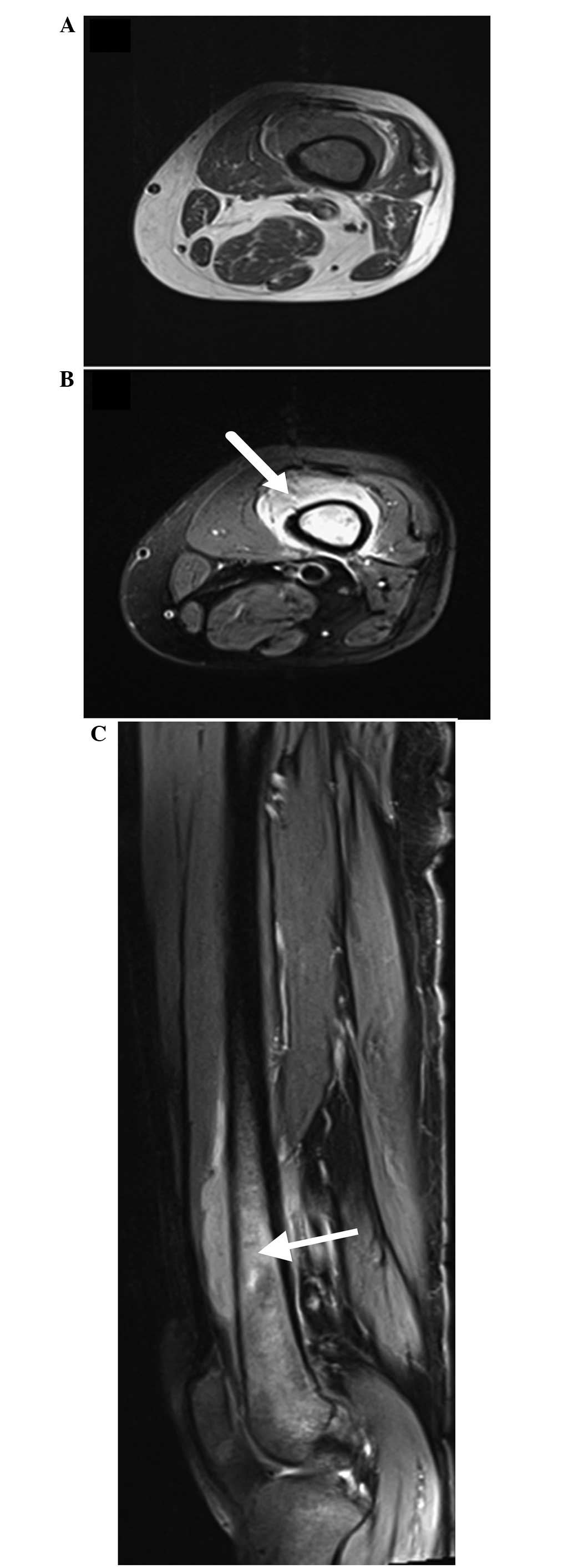
(Fig. 4), but plain CT scan revealed
a focus of marrow replacement, surrounded by a soft tissue mass
without cortical bone destruction (Fig.
5). The soft tissue mass displayed homogeneous texture, sharp
margins and mild enhancement surrounding the right femoral cava,
while the marrow replacement exhibited heterogeneous enhancement
upon administration of contrast medium (Fig. 6). Magnetic resonance imaging (MRI)
demonstrated a clearer lesion extent of marrow replacement, which
presented equal signal intensity on T1-weighted imaging and bright
signal intensity on T2-weighted imaging. The surrounding soft
tissue mass displayed the same signal intensity (Fig. 7).
According to the clinical manifestations and
radiological features, second primary tumor of bone rather than
metastatic tumor was hypothesized. Following limb salvage
treatment, microscopic examination of the specimen revealed that
the tumor cells aligned diffusely with remarkable heteromorphism
(Fig 8), and the adjacent striated
muscles were invaded. Immunohistochemical examination demonstrated
the tumor to be leukocyte common antigen+,
CD99+, vimentin−, desmin−,
melanoma−, synaptophysin−,
pancytokeratin−, CgA−, CD3−,
CD43+, CD20− and CD79a−. The
pathological diagnosis was established to be peripheral T-cell
lymphoma with the invasion of adjacent striated muscles.
According to the clinical manifestation and
pathological results, the final diagnosis was ASPS of the right
femur and PLB of the left femur. The patient then received
radiotherapy, and was followed up for 4 years. To date, there is no
evidence of bone marrow aspiration or abnormal laboratory
results.
Discussion
In the present study, the case of a 42-year-old
woman diagnosed with ASPS and PLB is reported. The patient
underwent en bloc surgical resection, chemotherapy and
radiotherapy, and remains currently alive.
The ASPS was located in the right femur, and had
invaded the surrounding muscle. This is an unusual location for
this tumor in an adult, according to previous reports (3,5). Certain
clinical signs and symptoms exhibited by the patient were also
considered unusual, such as the results of blood routine test,
which suggested anemia.
The microscopic features of tumor cells do not tend
to vary from tumor to tumor, and this uniformity is one of the
characteristics of ASPS (19). The
radiological features of primary bone manifestations of ASPS have
been previously described by Park et al (5). A common feature in all the cases of ASPS
reported by these authors was the detection of bone destruction
with poorly defined tumor margins and epicenter located in the
bone, indicating that the tumors occurred primarily in bone.
Previous studies have demonstrated that ASPS is distinguishable at
equal or slightly increased signal intensity relative to skeletal
muscle on T1-weighted MRI, and displays high and heterogeneous
signal intensity on T2-weighted MRI. In addition, the
administration of intravenous contrast medium results in strong,
uniform enhancement of tumor imaging (20). Tumor hypervascularity is characterized
by findings such as serpentine flow voids, due to peripheral
feeding and intratumoral vessels (20). In the present case report, X-ray
examination revealed a large right proximal femur osteolytic
process with cortical disruption, and CT scan confirmed the
presence of a large non-matrix producing soft tissue lesion of the
right proximal femur, which exhibited cortical destruction, but no
surrounding sclerosis or associated periosteal reaction were
observed. Cross-sectional imaging demonstrated that the epicenter
was located in the right femur, and the intraosseous soft tissue
mass was similar in size to the extraosseous component (19). This evidence supported the hypothesis
that the tumor originated in bone.
In conclusion, the clinical symptoms of ASPS
experienced by the patient of the present case report were not
typical, and imageological diagnosis was the fastest way of
confirming the disease, since MRI is the most effective method to
determine the dimension of bone destruction and hypervascularity
(20). Therefore, ASPS should be
considered in the differential diagnosis of bone-originating highly
vascularized soft tissue masses.
Currently, there is no consent definition or
diagnostic criteria for PLB (10–12,21–25).
It has been previously proposed that there may be lymph node
involvement if there is a 6-month window between the time of
diagnosis of the primary bone focus and the emergence of lymph node
disease (21). The diagnosis of PLB
may be challenging, since, it is often difficult to differentiate
clinically PLB and lymphomatous involvement of bone as a component
of extraosseous lymphoma (22,23). The
patient of the present case report presented a primary focus in a
single bone, which was confirmed histologically. However, there was
no evidence of distant lymph node or metastasis to meet the
diagnosis criterion. In the present case, the most typical symptom
of PLB displayed by the patient was bone pain not relieved by rest,
which was insidious and intermittent, similarly to a previous case
reported in the literature (21).
PLB is mainly of B-cell origin (10). However, the pathological diagnosis of
the patient in the present case report was established to be
peripheral T-cell lymphoma of the left femur. Although T-cell PLB
has been previously described, its incidence is rare, with the
exception of Japan and Hong Kong, where the disease is more common,
possibly due to the higher overall incidence of T-cell lymphoma in
these countries (24).
The radiological features of PLB are variable and
nonspecific (20–22). Conventional radiography typically
reveals an osteolytic pattern of bone destruction, but may instead
reveal a sclerotic or mixed lytic and sclerotic pattern, or may be
normal in 5% of the cases. In the present case, the results of
X-ray examination were normal. Previous studies have reported that
periosteal reaction is typically minimal in PLB, despite extreme
medullary infiltration (20–22). In addition, the presence of soft
tissue masses is common in PLB, but these are better detected by
cross-sectional imaging (24), since
CT may reveal soft tissue extension, cortical involvement, or
marrow invasion suggestive of malignancy, but these findings are
nonspecific (20–22). Radionuclide bone scans are abnormal in
the majority of patients with PLB (98%), demonstrating mild to
marked increased uptake (22).
Positron emission tomography may be aid in staging or detecting
residual disease following treatment, but does not contribute to
the initial diagnostic examination of suspected PLB (25). In MRI, the characteristic signals of
PLB tend to be heterogeneous and variable, and the majority of
lesions appear isointense or hypointense compared with muscle on
T1, and hypo, iso or hyperintense compared with subcutaneous fat on
T2 (20,23,26). The
low intensity of the lesion signals on T1 and T2 is speculated to
be associated with a high content of fibrous tissue in patients
with PLB (26). Furthermore,
enhancement patterns in PLB are usually heterogeneous (26). Soft tissue extension is present in the
majority of cases of PLB, and generally exhibits the same signal
intensity than the bone lesion (26).
Intramedullary extension is best assessed on MRI, since a clear
line of demarcation with normal marrow is usually observed
(23). PLB is rarely confined to the
periosteum or cortex with diffuse cortical thickening without
medullary involvement (23).
With the development of effective oncological
treatments, surgery is no longer required in the management of PLB
(11). Therefore, an accurate
diagnosis is required in order to avoid unnecessary surgical
procedures. Biopsy and imaging studies are effective for the
diagnosis of PLB, since MRI is the most sensitive technique for the
detection of intraosseous tumors (23).
In summary, the case of a 42-year-old woman with SPM
has been reported in the present study. To the best of our
knowledge, this is the first case of ASPS in the right femur and
PLB in the left femur occurring concomitantly in the same patient
to date. These two types of tumors present different inherent
imageology characteristics. The review of the literature conducted
in the present study identified that the incidence of SPMs is not
rare (15–18). Therefore, when the radiographic signs
are unexpected, the possibility of a second primary tumor should be
considered.
References
|
1
|
Weiss SW and Goldblum: Malignant soft
tissue tumors of uncertain type. Enzinger and Weisss Soft Tissue
Tumors (5th). (Philadelphia). Mosby Elsevier. 1182–1191. 2008.
|
|
2
|
Christopherson WM, Foote FW and Stewart
FW: Alveolar soft-part sarcomas; structurally characteristic tumors
of uncertain histogenesis. Cancer. 5:100–111. 1952. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhu FP, Lu GM, Zhang LJ, Wang JD, An XJ
and Dong YC: Primary alveolar soft part sarcoma of vertebra: A case
report and literature review. Skeletal Radiol. 38:825–829. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
van Ruth S, van Coevorden F, Peterse JL
and Kroon BB: Alveolar soft part sarcoma. A report of 15 cases. Eur
J Cancer. 38:1324–1328. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Park YK, Unni KK, Kim YW, Han CS, Yang MH,
Wenger DE, Sim FH, Lucas DR, Ryan JR, Nadim YA, et al: Primary
alveolar soft part sarcoma of bone. Histopathology. 35:411–417.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yavuz A, Göya C, Bora A and Beyazal M:
Primary alveolar soft part sarcoma of the scapula. Case Rep Oncol.
6:356–361. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zadnik PL, Yurter A, DeLeon R, Molina CA,
Groves ML, McCarthy E and Sciubba DM: Alveolar soft-part sarcoma in
the sacrum: A case report and review of the literature. Skeletal
Radiol. 43:115–120. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Singh T, Satheesh CT, Lakshmaiah KC,
Suresh TM, Babu GK, Lokanatha D, Jacob LA and Halkud R: Primary
bone lymphoma: A report of two cases and review of the literature.
J Cancer Res Ther. 6:296–298. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Oberling C: Les reticulosarcomes et les
reticuloendotheliosarcomes de la moelle osseuse (sarcomes dEwing).
Bull Assoc Fr Etud Cancer. 17:259–296. 1928.(In French).
|
|
10
|
Jawad MU, Schneiderbauer MM, Min ES,
Cheung MC, Koniaris LG and Scully SP: Primary lymphoma of bone in
adult patients. Cancer. 116:871–879. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ramadan KM, Shenkier T, Sehn LH, Gascoyne
RD and Connors JM: A clinicopathological retrospective study of 131
patients with primary bone lymphoma: A population-based study of
successively treated cohorts from the British Columbia Cancer
Agency. Ann Oncol. 18:129–135. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Power DG, McVey GP, Korpanty G, Treacy A,
Dervan P, OKeane C and Carney DN: Primary bone lymphoma: Single
institution case series. Ir J Med Sci. 177:247–251. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lones MA, Sanger W, Perkins SL and
Medeiros LJ: Anaplastic large cell lymphoma arising in bone: Report
of a case of the monomorphic variant with the t(2;5)(p23;q35)
translocation. Arch Pathol Lab Med. 124:1339–1343. 2000.PubMed/NCBI
|
|
14
|
Dong M, Wei H, Hou JM, Gao S, Yang DZ, Lin
ZH, Jia Y, Ren XP and Gao MH: Possible prognostic significance of
p53, cyclin D1 and Ki-67 in the second primary malignancy of
patients with double primary malignancies. Int J Clin Exp Pathol.
7:3975–3983. 2014.PubMed/NCBI
|
|
15
|
Vaslamatzis M, Alevizopoulos N, Petraki C,
Vrionis E, Zoumblios C, Stassinopoulou P, et al: Second primary
neoplasms (SPN) in cancer patients. Proc ASCO. 22:35812003.
|
|
16
|
Morgenfeld EL, Tognelli GF, Deza E,
Santillan D, Ares S, Morgenfeld E, et al: Synchronous and
metachronous second (ST) and third (TT) primary tumors (PT) in a
large patient population. Proc ASCO. 22:31522003.
|
|
17
|
Hulikal N, Ray S, Thomas J and Fernandes
DJ: Second primary malignant neoplasms: A clinicopathological
analysis from a cancer centre in India. Asian Pac J Cancer Prev.
13:6087–6091. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Irimie A, Achimas-Cadariu P, Burz C and
Puscas E: Multiple primary malignancies - epidemiological analysis
at a single tertiary institution. J Gastrointestin Liver Dis.
19:69–73. 2010.PubMed/NCBI
|
|
19
|
Wakely PE Jr, McDermott JE and Ali SZ:
Cytopathology of alveolar soft part sarcoma: A report of 10 cases.
Cancer. 117:500–507. 2009.PubMed/NCBI
|
|
20
|
Iwamoto Y, Morimoto N, Chuman H, Shinohara
N and Sugioka Y: The role of MR imaging in the diagnosis of
alveolar soft part sarcoma: A report of 10 cases. Skeletal Radiol.
24:267–270. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mulligan ME, McRae GA and Murphey MD:
Imaging features of primary lymphoma of bone. AJR Am J Roentgenol.
173:1691–1697. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
O'Neill J, Finlay K, Jurriaans E and
Friedman L: Radiological manifestations of skeletal lymphoma. Curr
Probl Diagn Radiol. 38:228–236. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Heyning FH, Kroon HM, Hogendoorn PC,
Taminiau AH and van der Woude HJ: MR imaging characteristics in
primary lymphoma of bone with emphasis on non-aggressive
appearance. Skeletal Radiol. 36:937–944. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gill P, Wenger DE and Inwards DJ: Primary
lymphomas of bone. Clin Lymphoma Myeloma. 6:140–142. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Takahashi T, Tsukuda H, Itoh H, Kimura H,
Yoshimoto M and Tsujisaki M: Primary and isolated adult T-cell
leukemia/lymphoma of the bone marrow. Intern Med. 50:2393–2396.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hermann G, Klein MJ, Abdelwahab IF and
Kenan S: MRI appearance of primary non-Hodgkins lymphoma of bone.
Skeletal Radiol. 26:629–632. 1997. View Article : Google Scholar : PubMed/NCBI
|