Introduction
As a minimally invasive surgical technique,
laparoscopic radical gastrectomy is associated with advantages
including reduced injury and postoperative pain, lower impact on
immune function, milder morbidity and rapid recovery of
gastrointestinal function with a short hospital stay (1–3).
Laparoscopic gastrectomy is commonly performed in Taizhou Hospital,
China, for the treatment of early and advanced gastric cancer. With
the advances in technology and surgical techniques, totally
laparoscopic distal gastrectomy may now be performed
intra-abdominally using only endoscopic linear staplers. Totally
laparoscopic distal gastrectomy has been defined as a method to
intracorporeally perform resection and anastomosis using a
laparoscopic technique (4–7). Totally laparoscopic distal gastrectomy
has several advantages over laparoscopy-assisted distal
gastrectomy, including reduced injury and a lower degree of
invasiveness (4).
Here, we present our initial experience with the
first patient who underwent totally laparoscopic D2 radical distal
gastrectomy using Billroth II anastomosis in our institution. We
evaluated the effectiveness of totally laparoscopic D2 radical
distal gastrectomy using Billroth II anastomosis in terms of
minimal invasiveness, technical feasibility and safety for the
resection of early gastric cancer.
Case report
Patient
A 55-year-old male patient was admitted to our
hospital due to upper abdominal discomfort accompanied with
belching for three years. Gastroscopic biopsy confirmed the
presence of adenocarcinoma of the gastric antrum (well
differentiated). Abdominal computed tomography (CT) scan revealed
the location of the gastric tumor (Fig.
1). No evidence of distant metastasis was observed during the
preoperative abdominal CT scan. The preoperative
tumor-node-metastasis (TNM) stage was cT2N0M0.
Surgical procedure
Following the administration of general anesthesia,
the patient was placed in the supine position with the head
elevated and legs apart. During the surgery, five trocars were
inserted. CO2 pneumoperitoneum of 12 to 14 mmHg was
established. Standing on the left side of the patient, the surgeon
divided the stomach and duodenum using an ultrasonic scalpel
(Ultracision Harmonic scalpel; Johnson & Johnson, Cincinnati,
OH, USA), and dissected the associated lymph nodes according to the
2002 edition of the Gastric Cancer Treatment Guidelines in Japan
(8). In brief, firstly, the left side
of the gastrocolic ligament was dissected near the transverse colon
through to the lower splenic pole and the pancreatic tail. Next,
the origins of the left gastroepiploic vessels were ligated. The
aim was to dissect station number 4 sb and 4 d lymph nodes. Then,
the right side of the gastrocolic ligament was cut near the
transverse ligament through to the hepatic flexure, and the hepatic
flexure of the colon was separated from the duodenal bulb and the
surface of the pancreatic head. In this way, the gastrocolic trunk
formed by the right gastroepiploic vein, right colic vein and their
confluence was completely revealed. Next, the right gastroepiploic
vessels were transected. The aim was to dissect station number 6
lymph nodes. Next, the gastroduodenal artery was exposed and the
right gastric artery was transected. The aim was to dissect station
number 12a and 5 lymph nodes. Then, the three branches of the
celiac trunk were divided and the left gastric artery was
transected. The aim was to dissect station number 7, 8a, 9 and 11p
lymph nodes. Finally, the hepatogastric ligament and the anterior
lobe of the hepatoduodenal ligament were transected close to the
lower edge of the liver, and the right side of the cardia and the
lesser curvature were fully separated. The aim was to dissect
station number 1 and 3 lymph nodes.
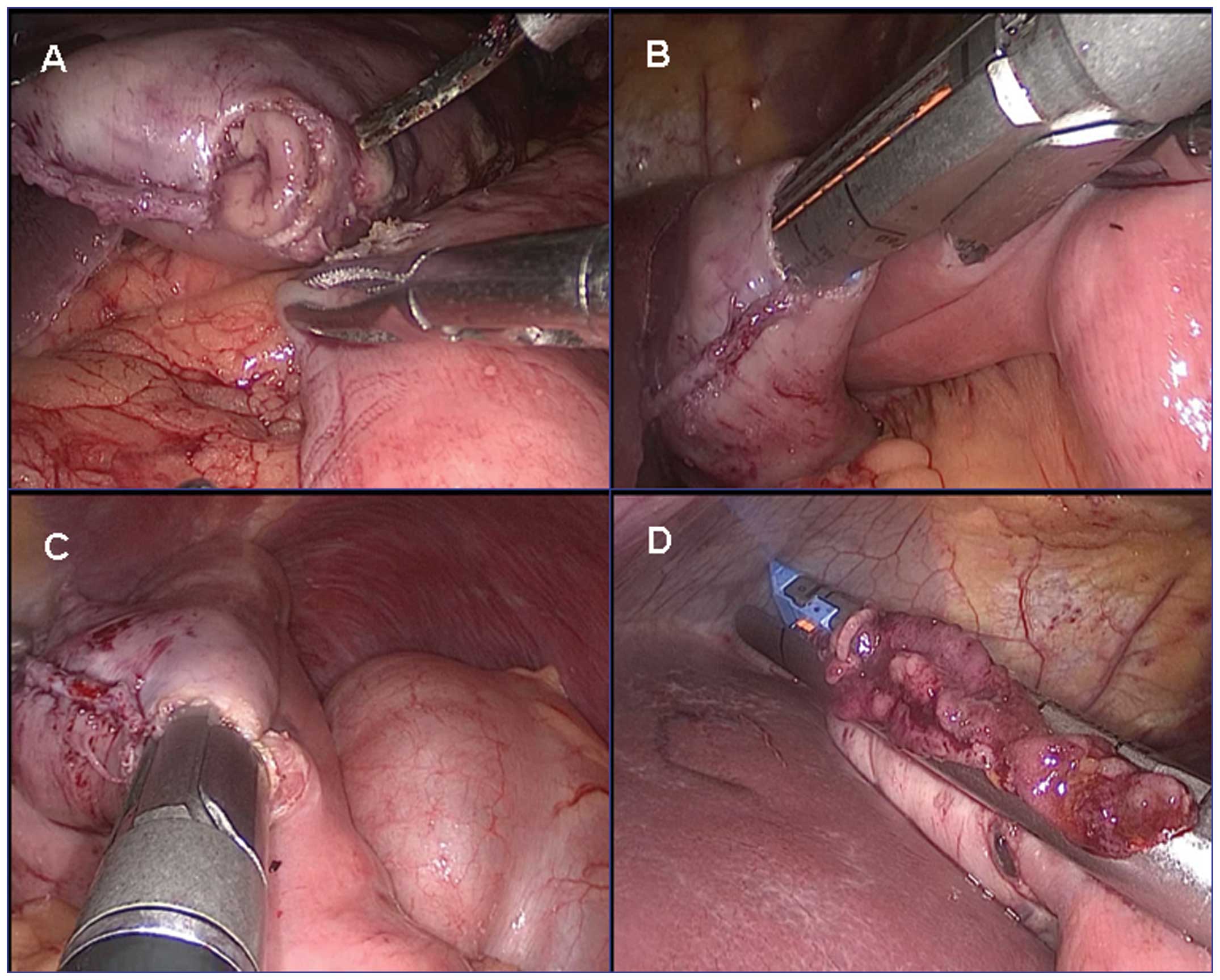
Following mobilization of the gastroduodenum, a
45-mm gastroscopic linear stapler was inserted through the left
upper trocar, positioned across the duodenum in the ventrodorsal
direction and fired (Fig. 2A and B).
Consequently, the transection line was rotated ~90 degrees from the
usual position. The stomach was then transected by successively
transecting from the greater curvature to the lesser curvature with
two 60-mm linear staplers (Fig. 2C and
D). The resected specimen including the stomach and the
surrounding tissue were placed into a large plastic bag and placed
beneath the umbilicus.
A small incision was created on the greater
curvature side of the remnant stomach and in the jejunum, 15 cm
away from the ligament of Treitz, respectively (Fig. 3A), by the ultrasonic scalpel. The
upper and lower anvils of a 60-mm linear stapler were inserted into
one end to close the posterior walls of the stomach and the
jejunum, respectively (Fig. 3B). The
posterior wall of the stomach and that of the jejunum were placed
together, and the 60-mm linear stapler was closed and fired
(Fig. 3C). Upon confirmation of no
leakage and bleeding of the anastomosis, the gastric tube was
inserted into the distal anastomotic end of the jejunum. Finally,
the common stab incision was closed using one 60-mm endoscopic
linear staple (Fig. 3D). The surgical
wound and anastomosis were explored to identify any active
bleeding. Thus, the reconstruction of the gastrointestinal tract
was completed.
The resected specimen in the large plastic bag was
removed through the umbilical incision, extended by cutting the
fascia longitudinally with a U-shaped skin incision.
Results
The surgery time was 180 min, and the time required
for totally laparoscopic Billroth II anastomosis was 15 min. The
percentage of the anastomotic time to the total time of surgery was
8.3%. The number of staples used was five, the estimated blood loss
was 30 ml, and no blood was transfused during the surgery. The
postoperative pathological stage was T2N0M0. The first flatus was
observed at 3 days and a liquid diet was started at 6 days.
Postoperative analgesic was used twice, and the patient's
postoperative hospital stay was 8 days. The patient developed no
complications such as anastomotic leakage, postoperative
hemorrhage, anastomotic stenosis or delayed gastric emptying, and
followed a satisfactory postoperative course.
Discussion
Totally laparoscopic gastrectomy is less invasive
and more comfortable for patients than laparoscopy-assisted
gastrectomy (4,9). However, totally laparoscopic gastrectomy
is not yet widely accepted, and its use is limited to just a few
centers. Although the majority of gastrointestinal surgeons prefer
laparoscopy-assisted gastrectomy rather than totally laparoscopic
procedures due to the technical difficulties of intracorporeal
anastomosis, previous studies suggest that totally laparoscopic
gastrectomy is feasible, safe and efficient when performed by
high-volume laparoscopic surgeons (10–12).
However, according to studies involving totally laparoscopic
gastrectomy, intracorporeal reconstruction of the digestive tract
has usually been performed using laparoscopic linear stapling
devices combined with a hand-sewing technique (7,13–16). It has placed great responsibility on
surgeons to find a safe, feasible and simpler method for
gastrointestinal anastomosis during totally laparoscopic
gastrectomy. In the present study, we described a Billroth II
intracorporeal anastomosis using only stapling devices without any
hand-sewing technique.
As shown in this study, the operation time of this
method was 180 min, the blood loss was 30 ml, the time spent in
hospital was 8 days, and no complications were observed after 3
months of follow-up. Compared with the reported studies of totally
laparoscopic subtotal gastrectomy (16–19), these
data suggest that our method of intracorporeal anastomosis using
only stapling devices is safe and feasible, and offers a better or
equally good early surgical outcome. Totally laparoscopic distal
gastrectomy has been spotlighted since all of the procedures may be
performed intracorporeally. However, laparoscopic intracorporeal
suturing and knot tying for anastomosis are considered the most
difficult laparoscopic skills to master (20,21). In
our case, the hand-sewing technique, which can make surgery
time-consuming and can also be a complicated procedure to learn,
was avoided during the procedure. In our case, reconstruction was
performed under continuous laparoscopic guidance, and the
disorientating and time-consuming switch to open surgery was
avoided. Our case has demonstrated a quicker recovery of bowel
function following intracorporeal reconstruction compared with
extracorporeal reconstruction.
In conclusion, the application of totally
laparoscopic Billroth II anastomosis with a linear stapler as part
of the intraperitoneal Billroth II reconstruction is safe and
feasible, allowing a satisfying postoperative recovery and
outcomes. Our initial clinical experience indicated that the
totally laparoscopic D2 radical distal gastrectomy using Billroth
II anastomosis is a simple, easy and safe method of intracorporeal
gastroduodenostomy.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant nos. 81374014 and 81472210),
Zhejiang Provincial Medical and Healthy Science and Technology
Projects (grant no. 2013KYA228), Zhejiang Provincial Science and
Technology Project (grant no. 2013C33112), the Science Research
Fund of Taizhou (grant nos. A121KY08, A131KY13-3 and A131KY13-12)
and Enze Medical Research Fund (grant nos. 12EZA1, 13EZA2 and
13EZB6).
References
|
1
|
Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU,
Kim W, Ryu SW, Lee HJ and Song KY: Morbidity and mortality of
laparoscopic gastrectomy versus open gastrectomy for gastric
cancer: an interim report - a phase III multicenter, prospective,
randomized trial (KLASS Trial). Ann Surg. 251:417–420. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mochiki E, Kamiyama Y, Aihara R,
Nakabayashi T, Asao T and Kuwano H: Laparoscopic assisted distal
gastrectomy for early gastric cancer: five years' experience.
Surgery. 137:317–322. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim YW, Baik YH, Yun YH, Nam BH, Kim DH,
Choi IJ and Bae JM: Improved quality of life outcomes after
laparoscopy-assisted distal gastrectomy for early gastric cancer:
results of a prospective randomized clinical trial. Ann Surg.
248:721–727. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N,
Taomoto J, Masuda T, Ohga T, Adachi E, Toh Y, Okamura T and Baba H:
Advantages of totally laparoscopic distal gastrectomy over
laparoscopically assisted distal gastrectomy for gastric cancer.
Surg Endosc. 23:2374–2379. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Guzman EA, Pigazzi A, Lee B, Soriano PA,
Nelson RA, Paz Benjamin I, Trisal V, Kim J and Ellenhorn JD:
Totally laparoscopic gastric resection with extended
lymphadenectomy for gastric adenocarcinoma. Ann Surg Oncol.
16:2218–2223. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Song KY, Park CH, Kang HC, Kim JJ, Park
SM, Jun KH, Chin HM and Hur H: Is totally laparoscopic gastrectomy
less invasive than laparoscopy-assisted gastrectomy?: prospective,
multicenter study. J Gastrointest Surg. 12:1015–1021. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huscher CG, Mingoli A, Sgarzini G,
Brachini G, Binda B, Di Paola M and Ponzano C: Totally laparoscopic
total and subtotal gastrectomy with extended lymph node dissection
for early and advanced gastric cancer: early and long-term results
of a 100-patient series. Am J Surg. 194:839–844. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nakajima T: Gastric cancer treatment
guidelines in Japan. Gastric Cancer. 5:1–5. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kinoshita T, Shibasaki H, Oshiro T,
Ooshiro M, Okazumi S and Katoh R: Comparison of
laparoscopy-assisted and total laparoscopic Billroth-I gastrectomy
for gastric cancer: a report of short-term outcomes. Surg Endosc.
25:1395–1401. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim MG, Kim KC and Kim BS, Kim TH, Kim HS,
Yook JH and Kim BS: A totally laparoscopic distal gastrectomy can
be an effective way of performing laparoscopic gastrectomy in obese
patients (body mass index ≥30). World J Surg. 35:1327–1332. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Roukos DH and Katsios C: Totally
intracorporeal laparoscopic gastrectomy for gastric cancer. Surg
Endosc. 24:3247–3248. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dulucq JL, Wintringer P, Perissat J and
Mahajna A: Completely laparoscopic total and partial gastrectomy
for benign and malignant diseases: a single institute's prospective
analysis. J Am Coll Surg. 200:191–197. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Singh KK, Rohatgi A, Rybinkina I,
McCulloch P and Mudan S: Laparoscopic gastrectomy for gastric
cancer: early experience among the elderly. Surg Endosc.
22:1002–1007. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee WJ, Wang W, Chen TC, Chen JC and Ser
KH: Totally laparoscopic radical BII gastrectomy for the treatment
of gastric cancer: a comparison with open surgery. Surg Laparosc
Endosc Percutan Tech. 18:369–374. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wong SK, Tsui DK and Li MK: Laparoscopic
distal gastrectomy for gastric cancer: initial experience on
hand-assisted technique and totally laparoscopic technique. Surg
Laparosc Endosc Percutan Tech. 19:298–304. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bouras G, Lee SW, Nomura E, Tokuhara T,
Nitta T, Yoshinaka R, Tsunemi S and Tanigawa N: Surgical outcomes
from laparoscopic distal gastrectomy and Roux-en-Y reconstruction:
evolution in a totally intracorporeal technique. Surg Laparosc
Endosc Percutan Tech. 21:37–41. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Scatizzi M, Kröning KC, Lenzi E, Moraldi
L, Cantafio S and Feroci F: Laparoscopic versus open distal
gastrectomy for locally advanced gastric cancer: a case-control
study. Updates Surg. 63:17–23. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Choi YY and Kim YJ: Intracorporeal
anastomosis using a Lapra-ty clip in laparoscopic distal
gastrectomy: initial clinical experiences. J Laparoendosc Adv Surg
Tech A. 21:51–55. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Du J, Shuang J, Li J, Zhao Q, Hong L, Du
X, Wen J and Hua J: Totally laparoscopic Billroth II gastrectomy
with a novel, safe, simple and time-saving anastomosis by only
stapling devices. J Gastrointest Surg. 16:738–743. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Figert PL, Park AE, Witzke DB and Schwartz
RW: Transfer of training in acquiring laparoscopic skills. J Am
Coll Surg. 193:533–537. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Portis AJ, Yan Y, Landman J, Chen C,
Barrett PH, Fentie DD, Ono Y, McDougall EM and Clayman RV:
Long-term followup after laparoscopic radical nephrectomy. J Urol.
167:1257–1262. 2002. View Article : Google Scholar : PubMed/NCBI
|