Introduction
The incidence of thyroid carcinoma is the highest
among head and neck carcinomas. Differentiated thyroid carcinoma
(DTC) accounts for 90% of thyroid cancers, with 20% of patients
experiencing disease relapse, which decreases survival rates
(1). A timely diagnosis of thyroid
cancer recurrence is critical. Evaluation of serum thyroglobulin
and 131I-diagnostic whole-body scanning (dWBS) are the
most commonly employed detection techniques. However, 15–20% of
patients with abnormal thyroglobulin levels show negative findings
on 131I-dWBS (2,3). Furthermore, it is difficult to
differentiate the recurrence of DTC from cicatricial tissue by
computed tomography (CT), positron emission tomography (PET),
magnetic resonance imaging (MRI), or ultrasound (4). Subsequently, PET/CT has been introduced
in the diagnostics of DTC, since PET/CT shows metabolic activity
and anatomical abnormalities, characteristic of the tumour.
Between December 2005 and June 2013,
18F-fluorodeoxyglucose (FDG) PET/CT was utilized to
diagnose 15 patients with DTC. The results identified
18F-FDG PET/CT as a valuable detecting technique for the
recurrence or metastasization of DTC.
Materials and methods
Patients
Fifteen patients with DTC were admitted to the
Department of Nuclear Medicine of the Xuzhou Central Hospital
(Xuzhou, China) between December 2005 and June 2013. There were 3
male and 12 female patients, aged 25–58 years, with a median age of
46 years (Table I). The patients were
diagnosed with DTC, and underwent total or subtotal
thyroidectomy.
 | Table I.Demographic and clinical data of 15
study patients. |
Table I.
Demographic and clinical data of 15
study patients.
| Patient, no. | Gender | Age, years | Histological type of
the tumour | PET/CT diagnosis | Surgery/follow-up
confirmation | Preoperative
thyroglobulin, ng/ml | Postoperative
thyroglobulin, ng/m |
|---|
| 1 | Female | 36 | Papillary
carcinoma | 2 cervical lymph
nodes | 2 in neck | 53.36 | 4.34 |
| 2 | Female | 45 | Papillary
carcinoma | 2 cervical lymph
nodes | 2 in neck | 34.51 | 2.47 |
| 3 | Male | 33 | Papillary
carcinoma | 2 cervical lymph
nodes | 2 in neck | 61.74 | 5.02 |
| 4 | Female | 48 | Follicular
carcinoma | 4 cervical lymph
nodes | 4 in neck | 66.85 | 5.77 |
| 5 | Female | 25 | Papillary
carcinoma | 3 cervical lymph
nodes | 2 in neck | 56.27 | 4.73 |
| 6 | Female | 58 | Papillary
carcinoma | 4 cervical lymph
nodes | 3 in neck | 72.02 | 6.08 |
| 7 | Male | 55 | Papillary
carcinoma | 2 cervical lymph
nodes | 2 in neck | 42.25 | 3.34 |
| 8 | Female | 29 | Papillary
carcinoma | 2 cervical lymph
nodes | 2 in neck | 58.13 | 4.86 |
| 9 | Female | 52 | Papillary
carcinoma | 2 cervical lymph
nodes | 2 in neck | 49.61 | 3.53 |
| 10 | Female | 40 | Papillary
carcinoma | 1 cervical lymph
node | 1 in neck | 26.68 | 1.18 |
| 11 | Female | 50 | Papillary
carcinoma | 5 cervical lymph
nodes | 4 in neck | 83.43 | 6.71 |
| 12 | Female | 42 | Papillary
carcinoma | 3 cervical lymph
nodes | 3 in neck | 92.62 | 7.29 |
| 13 | Female | 52 | Papillary
carcinoma | 3 cervical lymph
nodes | 3 in neck | 63.45 | 5.43 |
| 14 | Female | 49 | Papillary
carcinoma | 3 in the lung and 2
in the mediastinum | 3 in lung and 2 in
mediastinum | 475.03 | – |
| 15 | Male | 46 | Papillary
carcinoma | Negative | 1 in neck | 46.02 | – |
The pathological types comprised 14 cases of
papillary carcinoma and 1 case of follicular carcinoma. The
patients received 1 or several courses of postoperative treatment
with 131I: 1 patient was treated once, 4 patients were
treated twice, 6 patients were treated three times, 2 patients were
treated four times, 1 patient was treated six times, and the
remaining patient was treated eight times. At the follow up after
the treatment, elevated levels of thyroglobulin (>20 ng/ml) and
negative 131I-dWBS findings were present in each of
these patients. Subsequently, tumour recurrence or metastasization
was suspected. The patients underwent PET/CT examination. Patients
continued receiving thyroidin pills following surgery, including
during PET/CT, to avoid deterioration of the tumour.
18F-FDG PET/CT imaging
The Philips GXL 16 PET/CT scanning instrument
(Philips Medical Systems, Inc., Cleveland, OH, USA) was used. The
patients fasted for ≥6 h prior to scanning. Strict blood glucose
levels (non-diabetic patients, <6.1 mmol/l; patients with
diabetes, <8.3 mmol/l) were maintained. The patients were
intravenously administered 270–370 MBq of 18F-FDG (4.4
MBq/kg). After 60 min and prior to the scanning, the patients were
required to empty their bladders.
Collection ranges were from the basilar part to the
proximal femur. The 16-slice helical CT scanning parameters were
140 kV, 320 mA, with flat sweeping. Data were analyzed by image
fusion following iterative reconstruction, obtaining coronal,
sagittal and cross-sectional CT, PET and PET/CT fusion images. The
PET/CT images were reviewed independently by two radiologists who
calculated a standardized uptake value of radioactive hot lesion. A
standardized uptake value of ≥2.5 localized in metastatic regions
was considered as indicative of tumour metastasization.
Diagnostic criteria of tumour
recurrence or metastasization
Based on the positive results of PET/CT scanning,
the lesions located in the neck underwent surgical excision, and
postoperative histopathology was carried out. The patients were
monitored for their serum thyroglobulin levels for 1 month. If the
lesions were located in the organs where surgical excision was
problematic, the status was determined by clinical situation and
the follow-up imaging results within 6 months after the initial
PET/CT examination.
Data analysis
The PET/CT images were qualitatively ranked as true
positive, false negative, and false positive. Sensitivity and
positive predictive value (PPV) for the diagnosis of recurrence and
metastasization of DTC were calculated.
Statistical analysis
The SPSS 13.0 statistical software (SPSS, Inc.,
Chicago, IL, USA) was used for statistical analysis. Data were
presented as mean ± standard deviation. The differences were tested
using the paired t-test. P<0.05 was considered to indicate a
statistically significant difference.
Results
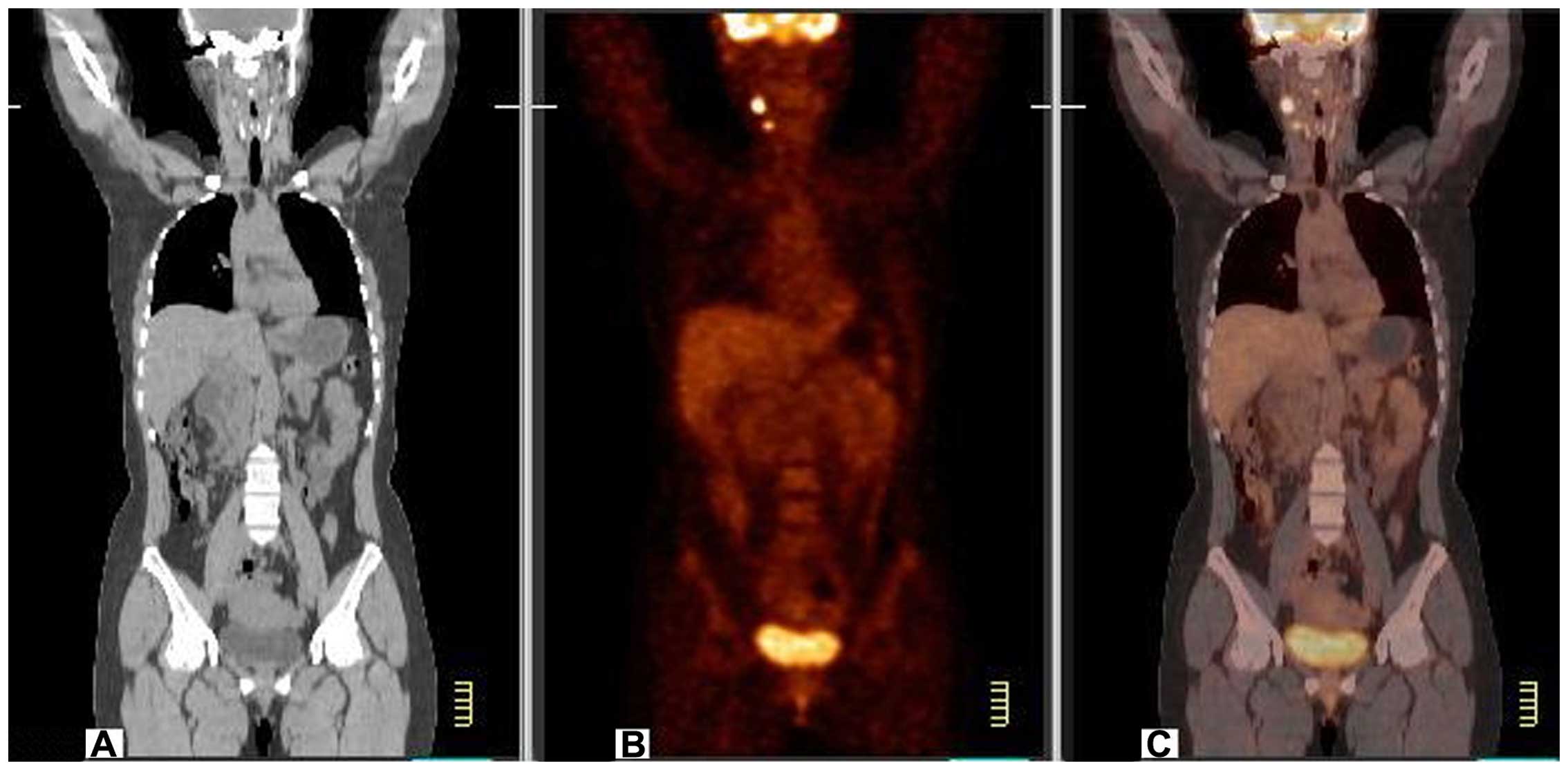
In 14 patients, PET/CT scanning had a sensitivity of
93.33%. The 14 patients were found to have 40 tumour recurrences or
metastases, of which 35 were cervical lymph node metastases
(Fig. 1). The tumours were excised
and were identified by postoperative pathology as being tumour
metastases in 32 cases and as inflammatory changes in 3 cases.
Thus, PPV comprised 91.43%. In 1 patient, 5 lumps were located in
the lungs and the mediastinum. No biopsy or surgical intervention
were conducted in this patient. The lumps increased during the
follow up for 6 months, confirming their metastatic nature.
One patient had negative PET/CT findings and
developed neck lumps after 6 months of follow up, which were
confirmed as tumour metastases.
A total of 13 patients with preoperative serum
thyroglobulin levels of 58.53±18.34 ng/ml underwent surgery. Their
postoperation serum thyroglobulin levels were 4.67±1.71 ng/ml
(p<0.05 vs. preoperative).
Discussion
Examination of thyroglobulin levels and
131I-dWBS following treatment is important for tumour
monitoring and the detection of metastasization in DTC (5). Elevated thyroglobulin levels indicate
recurrence or metastasization, resulting in 131I-dWBS
scans being able to locate the tumour. When 131I-dWBS
shows negative findings, B-mode ultrasound, CT, MRI, PET or other
imaging techniques are used to localize recurrent or metastatic
tumour. The first three methods are mainly used to locate the
tumour by anatomical abnormalities, while PET reveals the tumour
through metabolic abnormalities (6).
Each of these techniques has its advantages and limitations. By
contrast, PET/CT imaging can simultaneously reveal metabolic status
and anatomical location of the lesion, thus combining the
advantages of PET and CT (7). This
technique is useful in difficult diagnoses, such as that for
postoperative scars or nodules, which lack typical benign or
malignant signs. Malignant tumours consume glucose at 10-fold
higher rates than normal or scar tissue, and this feature enables
precise differential diagnosis in those cases (8). Therefore, combined functional and
morphological examination during PET/CT can improve the ability to
detect recurrent and metastatic tumours (9).
The diagnostic efficiency of 18F-FDG
PET/CT imaging in the postoperative follow up of patients with DTC
depends on patient selection, sample size, thyroglobulin levels,
and thyroid-stimulating hormone levels (10). Sensitivity and PPV for recurrence and
metastasization of DTC range from 66 to 93.3% and from 87.5 to
100%, respectively (11–13). These values are significantly higher
than those achieved by B-mode ultrasound, CT, MRI, or PET alone. In
the present study, sensitivity and PPV were 93.33 and 91.43%,
respectively, for patients with positive thyroglobulin levels and
negative 131I-dWBS findings. This is in agreeement with
previous findings (14–19). In such patients, metastatic tumour is
more aggressive, which leads to elevation of the sensitivity of
18F-FDG PET/CT imaging. However, tumours that uptake
iodine do not uptake FDG, therefore, 18F-FDG PET/CT
cannot fully replace 131I-dWBS and should not be
recommended for routine screening for recurrent or metastatic
DTC.
In conclusion, findings of the present study
indicate that 18F-FDG PET/CT imaging is an informative
technique for the detection of recurrence or metastasization of DTC
in patients with positive thyroglobulin levels and negative
131I-dWBS.
References
|
1
|
Wang E, Karedan T and Perez CA: New
insights in the treatment of radioiodine refractory differentiated
thyroid carcinomas: to lenvatinib and beyond. Anticancer Drugs.
26:689–697. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhang Y and Gao Z: Clinical application
and progress of PET/CT in differentiated thyroid carcinoma with
positive TG and negative 131I scanning. Chin Med Device
Inf. 17:8–12. 2011.(In Chinese).
|
|
3
|
Bertagna F, Bosio G, Biasiotto G, Rodella
C, Puta E, Gabanelli S, Lucchini S, Merli G, Savelli G, Giubbini R,
et al: F-18 FDG-PET/CT evaluation of patients with differentiated
thyroid cancer with negative I-131 total body scan and high
thyroglobulin level. Clin Nucl Med. 34:756–761. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Laurens ST and Oyen WJG: Value of
fluorodeoxyglucose pet/computed tomography patient management and
outcomes in thyroid cancer. Pet Clinics. 10:265–278. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Krajewska J and Jarzab B: Novel therapies
for thyroid cancer. Expert Opin Pharmacother. 15:2641–2652. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim TY, Kim WG, Kim WB and Shong YK:
Current status and future perspectives in differentiated thyroid
cancer. Endocrinol Metab (Seoul). 29:217–225. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lauri CI, Di Traglia S, Galli F,
Pizzichini P and Signore A: Current status of PET imaging of
differentiated thyroid cancer with second generation
radiopharmaceuticals. Q J Nucl Med Mol Imaging. 59:105–115.
2015.PubMed/NCBI
|
|
8
|
Tiedje VI, Schmid KW, Weber F, Bockisch A
and Führer D: Differentiated thyroid cancer. Internist (Berl).
56:153–166; quiz 167–168. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kim SJ, Lee TH, Kim IJ and Kim YK:
Clinical implication of F-18 FDG PET/CT for differentiated thyroid
cancer in patients with negative diagnostic iodine-123 scan and
elevated thyroglobulin. Eur J Radiol. 70:17–24. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ma C, Xie J, Lou Y, Gao Y, Zuo S and Wang
X: The role of TSH for 18F-FDG-PET in the diagnosis of recurrence
and metastases of differentiated thyroid carcinoma with elevated
thyroglobulin and negative scan: A meta-analysis. Eur J Endocrinol.
163:177–183. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kaneko K, Abe K, Baba S, Isoda T, Yabuuchi
H, Sasaki M, Hatakenaka M and Honda H: Detection of residual lymph
node metastases in high-risk papillary thyroid cancer patients
receiving adjuvant I-131 therapy: The usefulness of F-18 FDG
PET/CT. Clin Nucl Med. 35:6–11. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Panareo S, Rossi R, Cittanti C, Giganti M,
Prandini N, Franceschetti P, De Biasi V, Lunardon S and Feggi L:
Recombinant thyrotropin stimulation improves 18F-FDG PET/CT
sensitivity in patients with recurrent differentiated thyroid
cancer. J Nucl Med. 52(Suppl 1): 13082011.PubMed/NCBI
|
|
13
|
Leboulleux S, Schroeder PR, Busaidy NL,
Auperin A, Corone C, Jacene HA, Ewertz ME, Bournaud C, Wahl RL,
Sherman SI, et al: Assessment of the incremental value of
recombinant thyrotropin stimulation before
2-[18F]-Fluoro-2-deoxy-D-glucose positron emission
tomography/computed tomography imaging to localize residual
differentiated thyroid cancer. J Clin Endocrinol Metab.
94:1310–1316. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vera P, Kuhn-Lansoy C, Edet-Sanson A,
Hapdey S, Modzelewski R, Hitzel A, d'Anjou J and Basuyau JP: Does
recombinant human thyrotropin-stimulated positron emission
tomography with [18F]fluoro-2-deoxy-D-glucose improve detection of
recurrence of well-differentiated thyroid carcinoma in patients
with low serum thyroglobulin? Thyroid. 20:15–23. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hevrouet T, Devillers A, Cuggia M, Bernard
AM, Le Jeune F, Le Dortz L, Herry JY and Garin E: Influence of
rhTSH on 18 FDG uptake in a population of 42 patients with
suspected recurrence of differentiated thyroid carcinoma. Med Nucl
(Paris). 33:321–330. 2009.(In French).
|
|
16
|
Volante M, Collini P, Nikiforov YE,
Sakamoto A, Kakudo K, Katoh R, Lloyd RV, LiVolsi VA, Papotti M,
Sobrinho-Simoes M, et al: Poorly differentiated thyroid carcinoma:
The Turin proposal for the use of uniform diagnostic criteria and
an algorithmic diagnostic approach. Am J Surg Pathol. 31:1256–1264.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Stokkel MP, Duchateau CS and Dragoiescu C:
The value of FDG-PET in the follow-up of differentiated thyroid
cancer: a review of the literature. Q J Nucl Med Mol Imaging.
50:78–87. 2006.PubMed/NCBI
|
|
18
|
Yamaga LY, Cunha ML, Wagner J, Thom AF,
Daniel MM and Funari MB: Diagnostic value of positron emission
tomography/computed tomography with fluorine-18 fluordeoxyglucose
in patients with differentiated thyroid gland carcinoma, high
thyroglobulin serum levels and negative iodine whole body scan. Arq
Bras Endocrinol Metabol. 51:581–586. 2007.(In Portuguese).
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rivera M, Ghossein RA, Schoder H, Gomez D,
Larson SM and Tuttle RM: Histopathologic characterization of
radioactive iodine-refractory fluorodeoxyglucose-positron emission
tomography-positive thyroid carcinoma. Cancer. 113:48–56. 2008.
View Article : Google Scholar : PubMed/NCBI
|