Introduction
Epidermoid cysts are benign intracranial tumors that
are predominantly located in the cerebellopontine angle, accounting
for ~1% of intracranial tumors (1).
The cysts are lined with benign keratinizing squamous epithelium
and contain laminated keratin. Typical magnetic resonance imaging
(MRI) features include lesions with signal intensity slightly
greater than that of the cerebrospinal fluid on T1-weighted imaging
and high density on T2-weighted imaging without contrast
enhancement (2,3). The presence of contrast enhancement
within or adjacent to an epidermoid cyst is rare, but may indicate
various conditions including giant cell reaction, coexistence of
different histological types and malignant transformation of the
epidermoid cyst (4–6).
The current study presents a case of pathologically
confirmed epidermoid cyst with a focal enhancing area adjacent to
the lesion observed on MRI. The diagnostic procedure and
differential diagnosis are discussed. Written informed consent was
obtained from the patient's family.
Case report
In November 2013, a 55-year-old woman visited the
Neurosurgical Clinic at the Renji Hospital, Shanghai Jiaotong
University School of Medicine (Shanghai, China) due to intermittent
headaches and progressive right limb weakness in both limbs.
Physical examination upon admission revealed that the muscle
weakness in the right limb was grade 3, according to the modified
Medical Research Council grading scale (7). Computed tomography (CT; Aquilion™
Vision; Toshiba, Tokyo, Japan) of the head demonstrated a sharply
defined, low-density lesion occupying the left temporal region and
prepontine area (Fig. 1). MRI of the
head (Signa Excite System 3.0T; GE Healthcare Bio-Sciences,
Pittsburgh, PA, USA) revealed a large cystic mass in the left
temporal region and prepontine area, which was hypointense on
T1-weighted imaging and hyperintense on T2-weighted imaging, with
focal enhancement adjacent to the thalamus region, a 5-mm shift of
midline structure from right to left, and brainstem compression
(Fig. 1). The mass was approached via
a left modified trans-pterional approach. The focally enhanced part
of the mass was not resected due to its close association with the
basal ganglia and its possible pathological nature of a giant cell
reaction. The lesion appeared to have the typical pearly-white
gross appearance of an epidermoid cyst. The resected tissues were
fixed in 10% formalin, paraffin-embedded and cut into 5-mm sections
for immunohistochemical analysis. Hematoxylin-eosin (Solarbio Co.,
Ltd., Beijing, China) staining revealed that the cyst was lined by
keratinizing squamous epithelium and contained lamellated
keratinous debris; no malignant change was suspected from the
pathological findings of the resected specimen (Fig. 2A). A postoperative CT scan of the head
revealed disappearance of the cyst, and remnants of the enhancing
part of the lesion. The patient's symptoms were markedly improved
following the surgery (Fig. 1).
Intermittent CT of the head subsequent to the
surgery demonstrated that the size of enhancing part had gradually
increased in comparison with that on the immediate postoperative CT
(Fig. 2B–D). However, the patient
refused reoperation until paralysis of the right limb occurred ~7
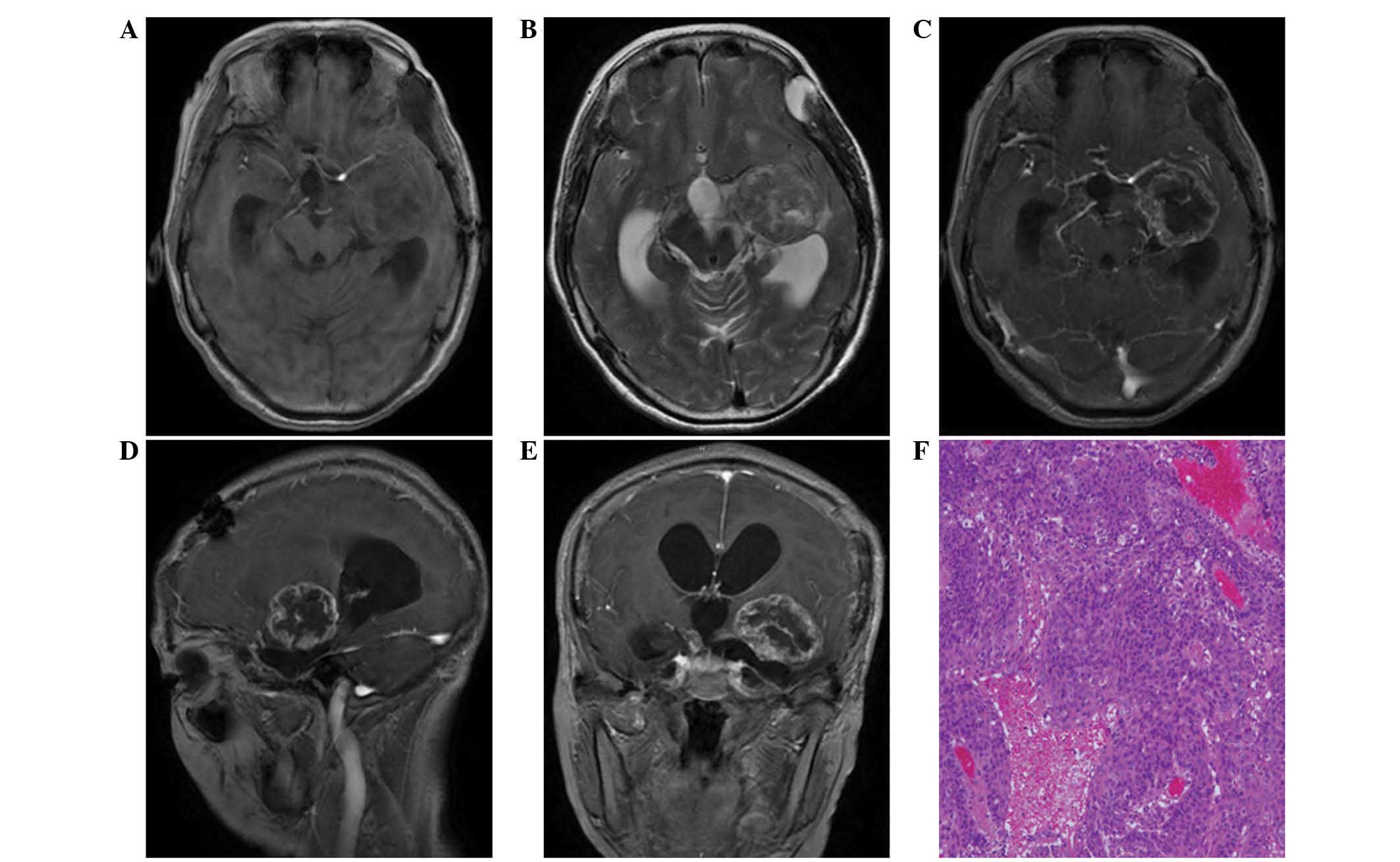
months later. Following re-admission, MRI of the head revealed that
the lesion occupied the left temporal lobe, appeared hypointense on
T1-weighted images and had mixed intensity on T2-weighted images,
with edge enhancement and hydrocephalus (Fig. 3A–E). The lesion was resected via the
aforementioned approach. Postoperative histological examination of
the lesion indicated squamous cell carcinoma (Fig. 3F). A metastatic work-up was conducted
subsequently to look for a primary focus elsewhere, but no
metastatic lesions were observed in other organs of the body.
The lesion was clinically diagnosed as a malignant
transformation of an epidermoid cyst. Adjuvant radiotherapy was
recommended. However, the patient refused adjunctive therapies for
personal reasons. The patient succumbed to pneumonia at ~6 months
following the second surgery.
Discussion
According to a systemic review conducted by Hamlat
et al (1) and the current
findings, present case is classified as the first type of malignant
transformation: Initial malignant transformation of an epidermoid
cyst. Malignant transformation of an epidermoid cyst is a
well-documented but rare occurrence (2,6). The rapid
progression of signs and symptoms is the most important clinical
indication of malignant transformation of epidermoid cysts
(8). The exact mechanism of malignant
changes of epidermoid cysts remain unclear. Chronic inflammatory
response to repeated cyst rupture and subtotal resection of the
cyst wall may result in malignant transformation (9).
Diagnosis of malignant transformation of an
epidermoid cyst is difficult, particularly when solely dependent on
imaging findings. Characteristic imaging findings of malignant
transformation of an epidermoid cyst include a focal enhancing
region within the mass on CT or MRI (2). In addition to typical imaging findings,
diffusion-weighted imaging may help to distinguish the nodular
enhancing area (2,10). Previous studies have reported that
malignant parts of an epidermoid cyst exhibit a low signal, whereas
benign regions exhibit a very high signal. Possible explanations
include central necrosis in the mass lesion and the
T2-shine-through effect (11).
Accurate diagnosis of malignant transformation of an epidermoid
cyst primarily depends on postoperative histopathological
examination. Garcia et al (12) and Hamlat et al (1) summarized the criteria for its
histological diagnosis (summarized in Table I). Hamlat et al (1) conducted a systematic review and found
that 70.3% of patients (52 of 74) fulfilled Garcia's criteria
(1).
 | Table I.Criteria for diagnosis of primary
squamous cell carcinoma. |
Table I.
Criteria for diagnosis of primary
squamous cell carcinoma.
| No. | Description |
|---|
| 1 | Tumor restricted to
the intracranial intradural compartment |
| 2 | No invasion of or
extension beyond the dura or cranial bones or through cranial
orifices |
| 3 | No communication with
the middle ear, air sinuses or sella turcica |
| 4 | No evidence of a
nasopharyngeal tumor |
| 5 | Presence of benign
squamous epithelium within the main tumor mass |
| 6 | No evidence of a
primary tumor elsewhere |
Differentiation between malignant transformation of
epidermoid cyst, giant cell reaction and coexistence of different
histological types on imaging findings is challenging (2). Leakage of cyst content, including
cholesterol, keratin and cellular debris, into the subarachnoid
space upon spontaneous rupture of the epidermoid cyst may result in
chemical meningitis. In such a situation, leptomeningeal
enhancement may be observed on post-contrast MRI (2). Foreign giant cell reaction, an
inflammatory giant cell reaction of the ruptured epidermoid cyst,
may also occur in the brain parenchyma (2). Moran et al (4) suggested that the epidermoid cyst in
their patient may have ruptured spontaneously into the adjacent
brain parenchyma, leading to an intense local inflammatory response
with the presence of multinucleated giant cells (4). In such cases, MRI may show an enhanced
region with associated vasogenic edema. As for the coexistence of
different histological types, to the best of our knowledge, there
has only been one case reporting the adjacent nodular enhancing
region and epidermoid cyst (5).
The prognosis of malignant transformation of an
epidermoid cyst is poor (6). Based on
a previous review, the mortality rate was as high as 75% (39 of 52
patients) (2). Surgery followed by
radiotherapy seems to be the optimal therapeutic modality (13). However, in the present case, the
patient declined our recommended treatment for personal reasons and
succumbed to disease within 12 months of the surgery.
The current study presents a rare case of malignant
transformation of an epidermoid cyst in the temporal and prepontine
region. Providing an accurate diagnosis of this type of tumor prior
to surgery is challenging; however, the possibility of malignant
transformation should be considered if the focal enhancing area is
visible. Comprehensive therapy is recommended for patients with a
definite diagnosis.
References
|
1
|
Hamlat A, Hua ZF, Saikali S, Laurent JF,
Gedouin D, Ben-Hassel M and Guegan Y: Malignant transformation of
intra-cranial epithelial cysts: Systematic article review. J
Neurooncol. 74:187–194. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kodama H, Maeda M, Hirokawa Y, Suzuki H,
Hori K, Taki W and Takeda K: MRI findings of malignant
transformation of epidermoid cyst: Case report. J Neurooncol,.
82:171–174. 2007. View Article : Google Scholar
|
|
3
|
Link MJ, Cohen PL, Breneman JC and Tew JM
Jr: Malignant squamous degeneration of a cerebellopontine angle
epidermoid tumor. J Neurosurg. 97:1237–1243. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Moran CC, Vakili ST, Caldemeyer KS and
Smith RR: Foreign body giant cell reaction associated with
epidermoid tumor: CT and MR findings. J Comput Assist Tomogr.
19:628–630. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Masuoka J, Sakata S, Maeda K and Sugita Y:
Adjacent epidermoid cyst and primary central nervous system
lymphoma: Case report. Surg Neurol. 69:530–533; discussion 533–534.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chon KH, Lee JM, Koh EJ and Choi HY:
Malignant transformation of an epidermoid cyst in the
cerebellopontine angle. J Korean Neurosurg Soc. 52:148–151. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Florence P, McCreary E, Provance P,
Rodgers M and Romani W: Muscles: Testing and Function with Posture
and Pain (5th). Lippincott Williams & Wilkins. Baltimore, MD:
2005.
|
|
8
|
Nakao Y, Nonaka S, Yamamoto T, Oyama K,
Esaki T, Tange Y, Mori K and Wada R: Malignant transformation 20
years after partial removal of intracranial epidermoid cyst-case
report. Neurol Med Chir (Tokyo). 50:236–239. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Abramson RC, Morawetz RB and Schlitt M:
Multiple complications from an intracranial epidermoid cyst: Case
report and literature review. Neurosurgery. 24:574–578. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nawashiro H, Higo R, Tokumaru AM, Tsuzuki
N and Shima K: Diffusion-weighted MRI of an intracranial epidermoid
with malignant transformation. Neuroradiology. 43:8912001.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Annet L, Duprez T, Grandin C, Dooms G,
Collard A and Cosnard G: Apparent diffusion coefficient
measurements within intracranial epidermoid cysts in six patients.
Neuroradiology. 44:326–328. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Garcia CA, McGarry PA and Rodriguez F:
Primary intracranial squamous cell carcinoma of the right
cerebellopontine angle. J Neurosurg. 54:824–828. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lakhdar F, Hakkouel M, Gana R, Maaqili RM
and Bellakhdar F: Malignant transformation six months after removal
of intracranial epidermoid cyst: A case report. Case Rep Neurol
Med. 2011:5252892011.PubMed/NCBI
|