Introduction
Esophageal cancer is the eighth most common type of
cancer worldwide, and the incidence rate is 11.5 in 100,000
individuals for men and 4.7 in 100,000 individuals for women
(1). Histologically, esophageal
cancers are divided into two primary types: Esophageal
adenocarcinomas and esophageal squamous cell carcinomas, which are
associated with the lower esophagus and between the middle and
upper esophagus, respectively (2).
The most common presenting symptom for esophageal cancer is
progressive dysphagia for solids, which progresses to dysphagia for
liquids over the course of weeks to months (3). Esophageal manometry is a common
procedure used for the detection of esophageal motility disorders,
and conventional pull-through and high-resolution manometry (HRM)
are each used clinically. HRM is an advanced form of manometry that
has been used in research and clinical practice (4). HRM is a device for esophageal pressure
recording, and a common procedure used for the diagnosis of
esophageal motility disorders, including achalasia,
gastroesophageal reflux disease, esophageal hiatus hernia and
nutcracker esophagus (5–7). HRM has multiple advantages, including
ease of use, high sensitivity and accuracy in the analysis of
detailed esophageal pressure topography (8,9) compared
with conventional pull-through manometry. The combination of HRM
with other examinations, including gastroscopy, endoscopic
ultrasound, barium esophagogram and impedance testing, may
therefore assist the diagnosis of esophageal cancer.
The current study presents the case of a patient
that had undergone an endoscopy and endoscopic ultrasound for
dysphagia; however, no evidence of cancer was observed.
Subsequently, an abnormal high-pressure zone was identified using
HRM, leading to an endoscopy and biopsy of a tumor. Therefore,
although HRM is usually used to diagnose esophageal motility
disorders, in the present case it was used as an aid to diagnose
esophageal cancer.
Case report
A 48-year-old female presented to the Sir Run Run
Shaw Hospital (Hangzhou, China) in September 2011 with a history of
dysphagia for 5 months and regurgitation for 1 week. At 5 months
prior to this presentation, the patient had developed dysphagia
with no clear cause, and no other symptoms were recorded. The
patient did not have a history or smoking or heavy drinking. The
patient visited a local hospital and underwent an upper endoscopy
that revealed coarse mucosa in the region of the distal esophagus
above the pectinate line, and dotted damaged mucosa distributed
sporadically without diffusion. The lesion with the largest
diameter measured ~0.3 cm. The patient was diagnosed with reflux
esophagitis (grade A), antral polyps and chronic superficial
gastritis with partial atrophy. Treatment with a combination of
traditional Chinese (unknown) and Western medicines (40 mg
pantoprazole once a day and 5 mg mosapride three times a day for
~15 days) was applied, but no improvement was shown. At 3 months
prior to presentation, the patient visited another local hospital
and an endoscopic ultrasound examination revealed a lesion, ~0.5-cm
in diameter, protruding into the anterior of the gastric antrum and
mucosa, with a smooth surface and a small amount of surrounding
swelling. A diagnosis of lesions protruding into the gastric antrum
and a thickened muscular layer was considered. The patient
continued to experience dysphagia and also presented with
regurgitation 1 week prior to being admitted to the Sir Run Run
Shaw Hospital for further evaluation. At the time of admission,
weight loss of 5 kg over the last week was noted.
Upon physical examination, the lymph nodes in the
bilateral supraclavicular region were palpable and measured ~0.5 cm
in diameter. Carbohydrate antigen 242 levels were found to be
slightly elevated at 16.48 U/ml (normal values, 0.00–10.00 U/ml),
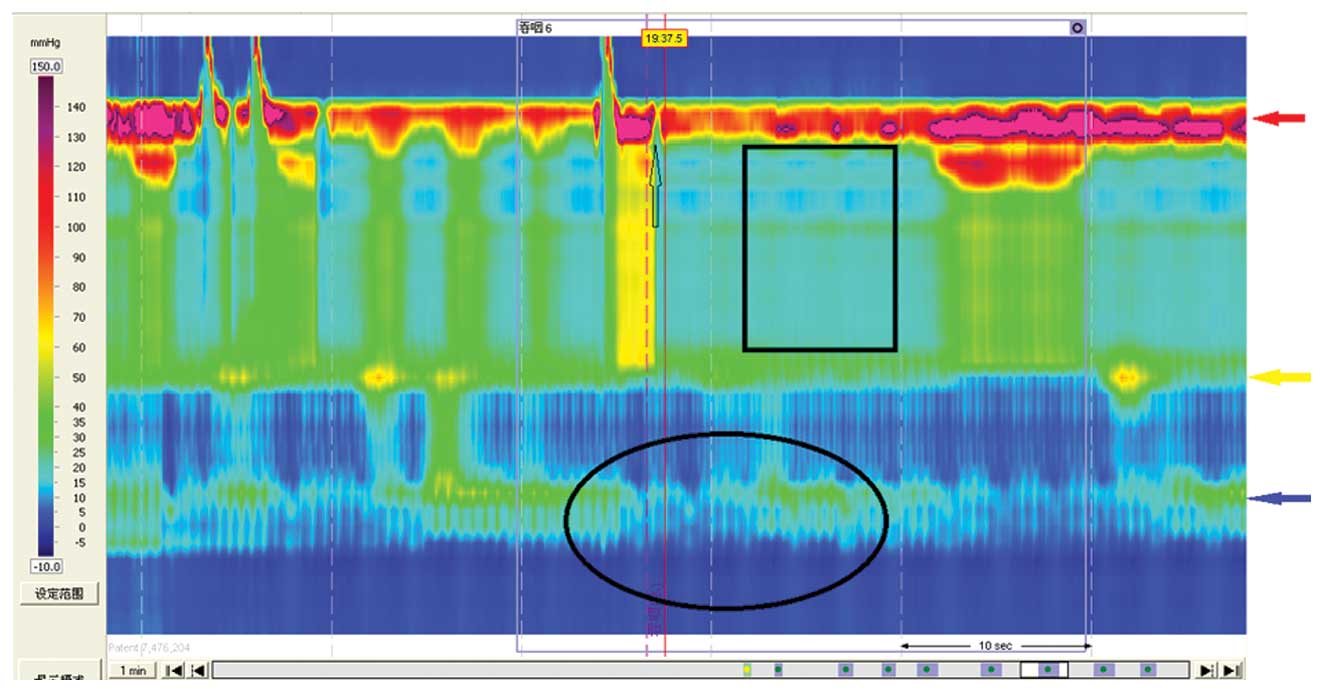
but all other blood chemistry results were normal. The HRM of the
esophagus performed to clarify the patient's condition revealed an
abnormal high-pressure zone that was located 33 cm from the incisor
and did not relax upon swallowing (A100 Manometry Equipment; Sierra
Scientific Instruments LLC, Los Angeles, CA, USA). Synchronous
waves were observed, and the pressure of the esophageal lumen was
found to increase with secondary synchronous peristaltic waves. The
lower esophageal sphincter (LES) was 39 cm from the incisor and
relaxed upon swallowing (Fig. 1). The
abnormal high-pressure zone could have been caused by an
obstruction, and therefore an upper gastrointestinal series (barium
swallow) test and gastroscopy were recommended to further pinpoint
the cause. The upper gastrointestinal series (barium swallow) test
(digital radiography; AXIOM Aristos FX; Siemens Healthcare,
Erlangen, Germany.) showed that a mucosal lesion, filling defect
and wall stiffness were present 56 mm along the esophagus, below
the level of the arcus aortae. In addition, the barium had
difficulty in passing through that region, suggesting that the
proximal esophagus was dilated (Fig.
2). Based on the aforementioned findings, mid-esophageal cancer
was considered as a possible diagnosis. A contrast-enhanced chest
computed tomography scan revealed wall thickening and narrowing of
the lumen in the thoracic segment of the esophagus, as well as
dilation of the upper segment of the esophagus accompanied by the
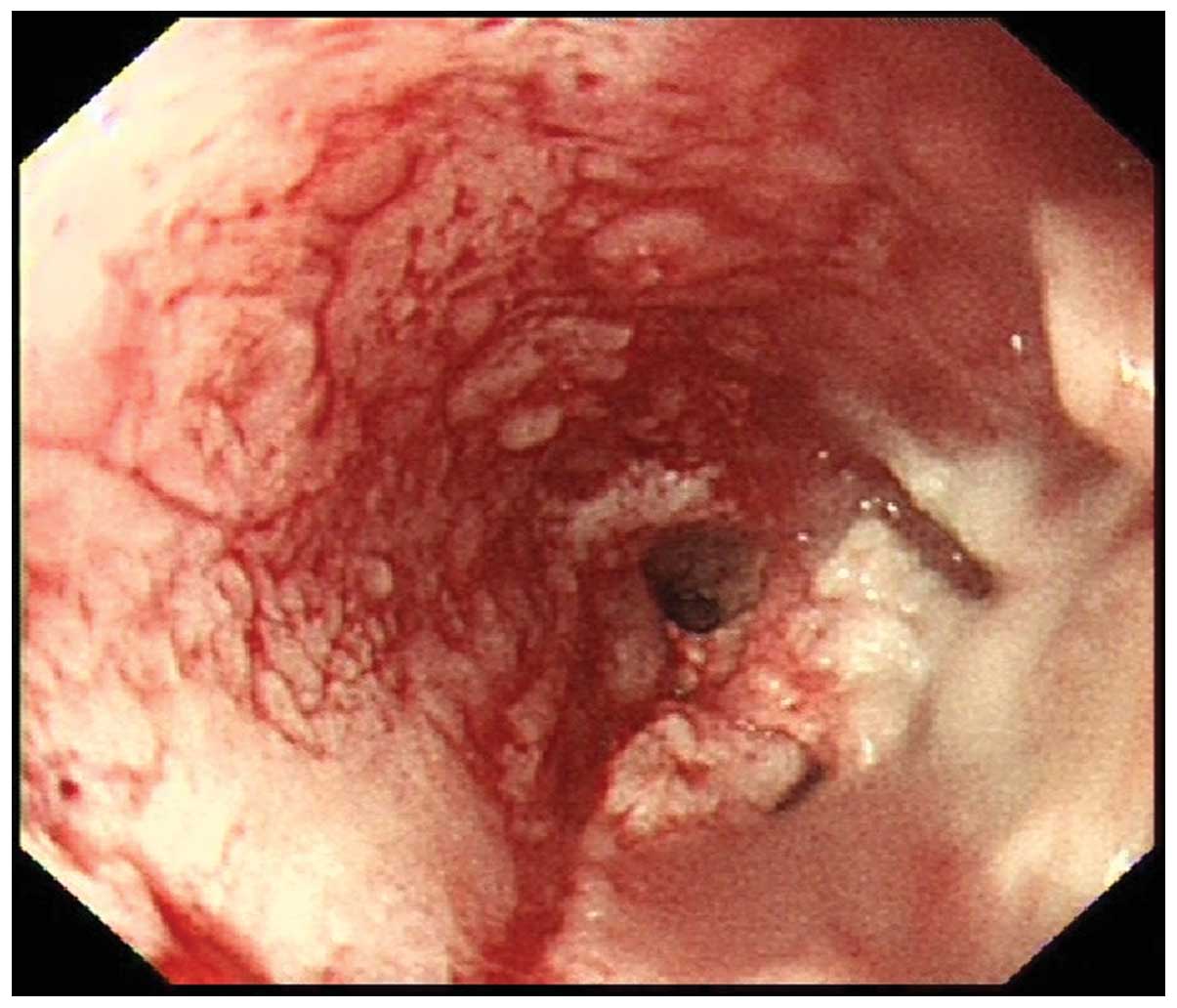
presence of excess fluid. Gastroscopy (CV-260; Olympus Corporation,
Tokyo, Japan) revealed nodular irregular ulcers with thick fur on
the surface, and surrounding lip-like mucosa 25–30 cm from the
incisor. These lesions were considered to have caused the narrowing
of the lumen, which made the advancing of the endoscope difficult
(Fig. 3). The patient was suspected
to have mid-esophageal cancer and the biopsy performed confirmed
the diagnosis of basaloid squamous cell carcinoma (BSC), due to the
pathological features observed in the excised tissue; cells
possessed round or oval nuclei with ‘dusty’ chromatin, pale
nucleoplasms and small distinct nucleoli, and the tumor lobules had
central comedo-type necrosis and peripheral palisading.
Written informed consent was obtained from the
patient for the publication of the present study.
Discussion
Esophageal cancer is the eighth most common type of
cancer worldwide, accounting for 2% of all malignant tumors, and
the sixth most common cause of mortality worldwide (1). Furthermore, 75% of the patients
presenting with this type of tumor succumb within the first year of
diagnosis, with a 5-year survival rate of <5%, due to its
invasiveness and difficulty in diagnosis (10). Therefore, the early diagnosis of
esophageal cancer can markedly improve the survival time of
patients.
Esophageal cancer has two pathological subtypes:
Squamous carcinoma and adenocarcinoma. BSC comprises a rare subtype
of squamous carcinoma found mainly in the upper respiratory and
digestive tracts, which was first reported by Wain et al
(11) in 1986. A previous study
reported the incidence of BSC to be <1% (12). This type of carcinoma derives from the
fundus of pseudostratified columnar epithelium in the esophageal
gland ducts or primitive acinar cells; the mucosa is complete
without damage in the early phase, and the tumor grows under the
mucosa. Tumor growth oppresses the mucous epithelium, resulting in
damage that can cause an ulcer. A previous study of 10 cases
reported that BSC patients are typically older males with a history
of drinking and smoking (11);
however, increasing incidence rates of BSC have been observed in
young females and individuals who do not smoke or consume alcohol.
In the present case, the patient was a 48-year-old female.
Despite the fact that the patient developed
dysphagia 5 months ago, solid and liquid food could be swallowed,
although vomiting was occasionally noted afterwards. The symptoms
were not aggravated and the results from tests performed at local
hospitals did not reveal any presence of cancer 3 months prior to
the current admission to the Sir Run Run Shaw Hospital; however, 1
week prior to admission, the patient suddenly presented with
regurgitation and difficulty in swallowing even liquids. It is
known that the mucosa is not damaged in the early phases of the
disease, which may result in a negative upper endoscopic
examination, despite the growth of the tumor beneath the mucosa,
causing the symptoms to appear only when esophageal motility is
affected (13).
HRM is performed as follows: 36 Solid-state channels
are spaced at 1-cm intervals, with 12 sensors distributed evenly
around each channel, for a total of 432 pressure sensors in a
electrode catheter, with a diameter of 4.7 mm. The technique can
therefore simultaneously measure esophageal tension, peristalsis,
and the length and pressure of the sphincter. Based on the
anatomical features of the esophagus, only two high-pressure zones
in the upper esophageal sphincter and LES can be visualized at
rest. In the present patient, a high-pressure zone was observed 33
cm from the incisor, with synchronous waves, indicating achalasia.
The patient was 155 cm tall; the LES in individuals of this height
is known to be 40 cm from the incisor (14). An unexpected low-pressure zone, which
relaxed after swallowing 5 ml of water, was observed 6 cm below the
high-pressure zone. It was determined that the low-pressure zone
was in the LES, while the high-pressure zone was caused by an
obstruction, which was confirmed by an upper gastrointestinal
series (barium swallow) test and gastroscopy.
The present results suggested that physicians should
focus attention on abnormal high-pressure zones when measuring
esophageal pressure. Physiological stricture due to compression by
the arcus aortae should be excluded as a cause first. In certain
cases, compression by the arcus aortae or an enlarged heart could
be responsible, but this could readily be distinguished by counting
the number of beats (3,15,16). In
addition, physicians should also take into account compression
caused by foreign bodies or conditions that can affect the
esophagus, such as tight belts, hiatus hernia and esophageal
narrowing caused by an ulcer or a tumor. Prior to examining the
patient, it is important to remove their belt in order to make sure
that any abnormal high-pressure zones observed are not caused by
pressure on the gastric area. During data analysis, it is important
to determine the pressure inversion point in the gastroesophageal
junction, to exclude a large giant hiatus hernia.
A dilated esophagus can induce synchronous waves,
thus, organic diseases should be excluded as the cause when
patients are diagnosed with achalasia. The presence of synchronous
waves, as well as diffuse and segmental esophageal spasms, is
commonly observed in patients with achalasia (3).
Overall, it is possible that the presence of cancer
was not reported by endoscopy, since the early phases of a
sub-mucosal lesion or motility disorder of the esophagus do not
result in changes that can be detected endoscopically; therefore,
for those patients presenting with evident symptoms of esophageal
motor dysfunction without significant findings by gastroscopy, HRM
is recommended and further examination or follow-ups are required.
Finally, esophageal carcinoma should be considered when an abnormal
high-pressure zone is observed by HRM.
Acknowledgements
This study was supported by the Zhejiang Province
Key Science and Technology Innovation Team (grant no. 2013TD13) and
the Health Department of Zhejiang Province (grant no.
2014KYB121).
References
|
1
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Devesa SS, Blot WJ and Fraumeni JF Jr:
Changing patterns in the incidence of esophageal and gastric
carcinoma in the United States. Cancer. 83:2049–2053. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kruger D: Assessing esophageal dysphagia.
JAAPA. 27:23–30. 2014.PubMed/NCBI
|
|
4
|
Fox MR and Bredenoord AJ: Oesophageal
high-resolution manometry: Moving from research into clinical
practice. Gut. 57:405–423. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bredenoord AJ and Smout AJ:
High-resolution manometry of the esophagus: more than a colorful
view on esophageal motility? Expert Rev Gastroenterol Hepatol.
1:61–69. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pandolfino JE, Fox MR, Bredenoord AJ and
Kahrilas PJ: High-resolution manometry in clinical practice:
Utilizing pressure topography to classify oesophageal motility
abnormalities. Neurogastroenterol Motil. 21:796–806. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bredenoord AJ, Fox M, Kahrilas PJ,
Pandolfino JE, Schwizer W and Smout AJ: International High
Resolution Manometry Working Group: Chicago classification criteria
of esophageal motility disorders defined in high resolution
esophageal pressure topography. Neurogastroenterol Motil. 24(Suppl
1): 57–65. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kahrilas PJ, Ghosh SK and Pandolfino JE:
Esophageal motility disorders in terms of pressure topography: The
Chicago Classification. J Clin Gastroenterol. 42:627–635. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bredenoord AJ and Smout AJ:
High-resolution manometry. Dig Liver Dis. 40:174–181. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hiyama T, Yoshihara M, Tanaka S and
Chayama K: Genetic polymorphisms and esophageal cancer risk. Int J
Cancer. 121:1643–1658. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wain SL, Kier R, Vollmer RT and Bossen EH:
Basaloid-squamous carcinoma of the tongue, hypopharynx, and larynx:
Report of 10 cases. Hum Pathol. 17:1158–1166. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Epstein JI, Sears DL, Tucker RS and Eagan
JW Jr: Carcinoma of the esophagus with adenoid cystic
differentiation. Cancer. 53:1131–1136. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tsang WY, Chan JK, Lee KC, Leung AK and Fu
YT: Basaloid-squamous carcinoma of the upper aerodigestive tract
and so-called adenoid cystic carcinoma of the oesophagus: The same
tumour type? Histopathology. 19:35–46. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen J, Qiao RM and Shang J: The
relationship between positions of upper and lower esophageal
sphincter and height and age. Zhonghua Xiaohua Neijing Zazhi.
23:126–127. 2006.(In Chinese).
|
|
15
|
Kahrilas PJ, Kim HC and Pandolfino JE:
Approaches to the diagnosis and grading of hiatal hernia. Best
Pract Res Clin Gastroenterol. 22:601–616. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hou X: Techniques for high resolution
manometry. High Resolution Manometry in Digestive Tract. Science
Press. (Beijing). 1582014.
|