Introduction
Dermatomyositis (DM) is a rare, autoimmune disease
of the connective, which is associated with immune complex
deposition and subsequent inflammatory cell accumulation (1). The incidence rate of tumors in patients
with DM has been reported to display a variable frequency of
0.6–1.0 per 100,000 individuals (2).
Diagnosis of dermatomyositis is associated with a higher risk of
malignances, including the ovary, lung, pancreas, stomach,
colorectal cancer and non-Hodgkin lymphoma particularly for
patients aged >40 years (3). The
agents including corticosteroids and immunosuppressive drugs are
always used in the treatment of dermatomyositis. The purposes of
treatment are to improve the ability of daily living by increasing
muscle strength and to alleviate extramuscular manifestations,
including rash, dysphagia, dyspnoea, arthralgia and fever.
Approximately 30% of the patients are left with mild to severe
disability though the prognosis has been obviously improved. Age
and association with tumor are risk factors associated with poor
prognosis. DM often presents as a paraneoplastic syndrome, thus
implying the presence of a tumor (4).
A probable hypothesis for the development of DM is that shared
immunological processes link malignancy with myopathy (5). The present study describes a case of DM
and undifferentiated lung cancer, which was surgically treated.
Following video-assisted thoracoscopic surgery (VATS) right upper
lobectomy and lymph node dissection, the DM symptoms resolved.
Case report
A 69-year-old male patient, who was a former smoker
(smoked 1 pack a day for 40 years), was admitted to the Shandong
Provincial Hospital Affiliated to Shandong University (Jinan,
China) in December 2010 presenting with typical cutaneous rash and
aggravating proximal muscle weakness for 3 months. Three months
prior to admission, the patient had noticed a rash of an unclear
cause on his face, neck, chest, back and hands (Fig. 1). Almost at the same time, the patient
experienced aggravating proximal muscle weakness. Upon admission to
the hospital, laboratory test results revealed elevated levels of
creatine kinase (CK) (627.7 U/l; normal values, 35.0–185.0 U/l).
The results of immunological tests, including anti-double-stranded
DNA (cat. no. EA1571; 1:200) and antinuclear (cat. no. EA1590-8;
1:100) antibody tests EUROIMMUN Medical Diagnostics (Beijing,
China), were negative. The tumor markers carcinoembryonic antigen
(cat. no. TF 3H8-1; 1:1), carbohydrate antigen (CA) 19–9 (cat. no.
121SLE; 1:1), CA 125 (cat. no. OC125; 1:1), alpha-fetoprotein (cat.
no. ELA-04957; 1:1), neuron-specific enolase (cat. no. MRQ-55;
1:1), cytokeratin 19 fragment (cat. no. 11820966; 1:1) and
prostate-specific antigen (cat. no. ER-PR8; 1:1) (monoclonal
antibodies diluted with PBS and 10% FBS, incubated for 30 min at
room temperature; Roche Diagnostics, Shanghai, China) were all
negative. Muscle strength testing revealed proximal muscle
weakness. Electromyography performed with Keypoint 6 (9033A07;
Dantec Dynamics, Skovlunde, Denmark) confirmed proximal myopathy.
The patient was diagnosed with DM, based on the typical skin rash,
elevated CK levels and abnormal electromyogram (Dantec Dynamics,
Skovlunde, Denmark). Enhanced chest computed tomography (CT) scan
(Siemens AG, Erlangen, Germany) revealed a tumor located in the
right upper lobe. (Fig. 2A). Whole
body positron emission tomography scan (GE Medical Systems,
Waukesha, WI, USA) demonstrated a high fluorodeoxyglucose uptake
rate by the tumor, with no obvious enlarged lymph nodes or distant
metastasis (Fig. 2B). The final
diagnosis was lung cancer (stage IB and T2aN0M0, based on the
tumor-lymph-node-metastasis classification) (6), with DM presenting as a paraneoplastic
syndrome. Upon diagnosis of DM, the patient commenced treatment
with 40 mg oral prednisone (Qilu Pharmaceutical Co., Ltd., Jinan,
China) and 200 mg oral hydroxychloroquine (Sanofi, Shanghai, China)
once per day, prior to being subjected to VATS (LTF-240, Olympus
Medical Systems Corp., Tokyo, Japan) right upper lobectomy and
lymph node dissection. Prednisone and hydroxychloroquine treatment
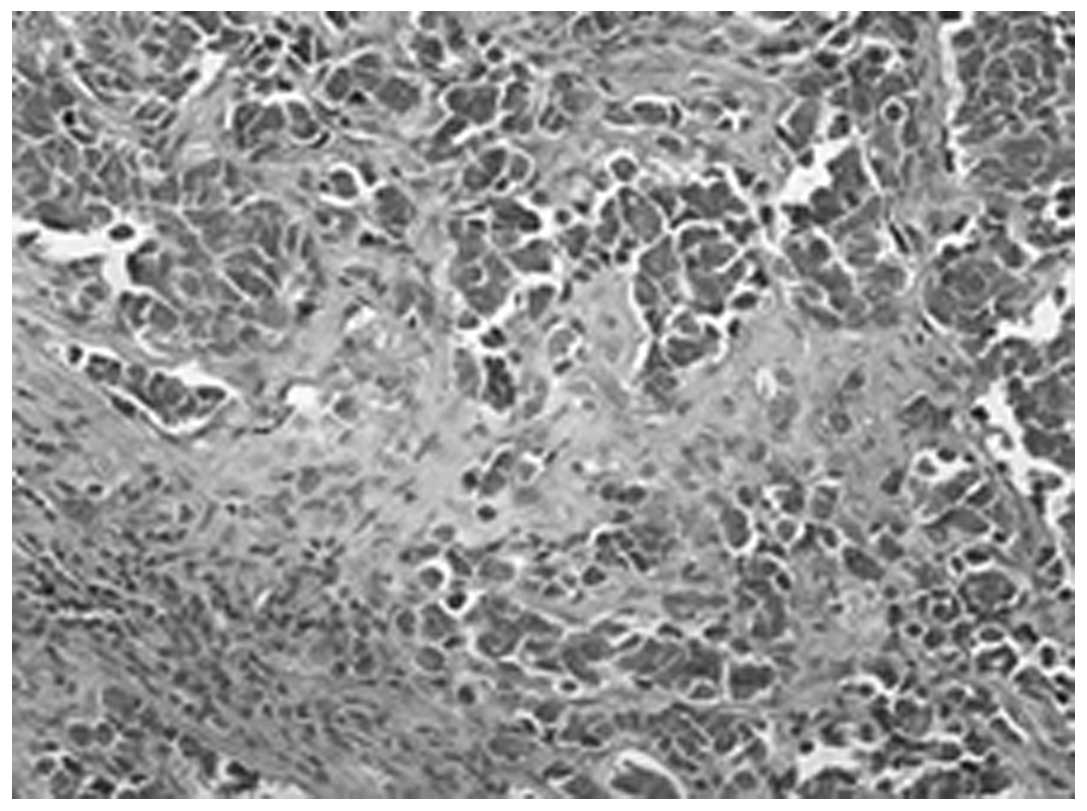
was terminated ~1 month after surgery. Postoperative pathological
examination using an Olympus Medical Systems Corp. microscope
(BX51) confirmed undifferentiated cancer (Fig. 3) and pulmonary hilar lymph node
metastasis.
The postoperative course of the patient was
uneventful, and a considerable improvement in muscle weakness, as
well as normalization of the CK levels, were observed. During the
6-month follow-up examination, the patient received chemotherapy
and remained healthy, without DM symptoms or cancer relapse.
However, the patient decided to discontinue the subsequent
follow-ups in the Shandong Provincial Hospital Affiliated to
Shandong University, and his clinical condition at the time of
writing was unknown.
Discussion
DM is an idiopathic autoimmune disease characterized
by skin and muscle lesions, with an incidence rate of 0.6–1.0 per
100,000 individuals (2) and a female
to male ratio of 2:1 (1). DM mainly
affects children and adults with two peak age ranges: Children aged
5–14 years and adults aged 45–60 years (1).
The exact disease mechanism has not been fully
determined. DM is characterized by immune complex deposition in the
capillary beds and frequent presence of inflammatory cell
accumulation, mainly T cell-mediated myotoxicity or
complement-mediated microangiopathy, which infiltrate myocytes
leading to structural changes, including vacuolization and
degeneration (2,7). Expression of capillary endothelium
antigens, subsequent complement activation and immune complex
deposition are known to induce endothelial cell edema,
vacuolization, capillary necrosis, perivascular inflammation and
ischemia, with muscle fiber destruction (2,7).
Clinical symptoms of DM include progressive
symmetric proximal muscle weakness and typical skin lesions
(7). Serious cases of DM with
respiratory muscle involvement may be fatal (8). The typical skin lesions associated with
DM are heliotrope erythema around the eyes and dusky erythematous
skin rashes on the face, neck, posterior arms and upper trunk
(4). Other symptoms that may be
present in different degrees include the following: i) Systemic
symptoms, such as fever and weight loss; ii) musculoskeletal
changes, such as arthralgia and synovitis; iii) gastrointestinal
disorders, such as dysphagia, dysmotility and malabsorption; iv)
cardiac and pulmonary disorders, such as tachyarrhythmia and
interstitial lung disease; and v) vascular disorders, such as
Raynaud's phenomenon and vasculitis (9).
DM diagnosis is mainly based on the Bohan and Peter
criteria listed below: i) Progressive proximal and symmetric muscle
weakness; ii) muscle biopsy exhibiting characteristic changes of
myositis; iii) elevated levels of serum skeletal muscle enzymes;
iv) electromyography indicating primary myopathic changes; and v)
typical skin lesions (10). In the
present case, the diagnosis of DM was based on the above symptoms
iii-v.
An association between DM and an increased risk of
malignancy has been previously demonstrated. Tumors have been shown
to usually occur following the onset of DM, or simultaneously with
it (3,11). The most common malignancies associated
with DM are lung, colorectal, cervical and ovarian cancer (12); however, the cause and effect
relationship between cancer and DM is not fully understood
(4). Several possible hypotheses have
been established regarding the occurrence of DM and
malignancy-immune disorders, viral infections or substance
secretion by cancer cells that facilitate abnormal immunologic
responses. The tumors may share cross-reacting antigens with muscle
fibers, tendon sheath and blood vessels. Related cross-reacting
antibodies may lead to concurrent occurrence of DM (13). In numerous cases, DM manifests as a
paraneoplastic syndrome. The paraneoplastic clinical symptoms not
directly associated with the primary tumor or metastasis have been
shown to resolve following complete removal of the tumor (3); in case of tumor relapse, muscle weakness
and typical skin rash recurrence is observed, suggesting the
paraneoplastic nature of DM (14).
There also appear to be some clinical differences in these
patients, as their CK values are closer to normal and are less
likely to present myositis-specific antibodies (11).
In the current case, DM presented as a
paraneoplastic syndrome accompanied by undifferentiated cancer of
the right upper lobe. DM symptoms comprised the first indication of
cancer. Surgical removal of the tumor was performed, which led to a
marked alleviation of the symptoms, thus supporting the
paraneoplastic nature of DM.
In conclusion, DM is a disease with a relatively
simple clinical diagnosis; however, clinicians consider the
possible association of DM with malignancy. The existence of occult
primary tumors should be excluded in all patients with a diagnosis
of DM, based on patient's age, gender, local epidemiology and risk
factors. Patients aged >40 years should be particularly screened
for potential malignancies. The results of the present study
suggested that early diagnosis and timely treatment is crucial for
the prognosis of the tumor. In addition, a diagnosis of DM should
always be considered a warning sign of malignancy.
References
|
1
|
Mastaglia FL and Phillips BA: Idiopathic
inflammatory myopathies: Epidemiology, classification, and
diagnostic criteria. Rheum Dis Clin North Am. 28:723–741. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dalakas MC and Hohlfeld R: Polymyositis
and dermatomyositis. Lancet. 362:971–982. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hill CL, Zhang Y, Sigurgeirsson B, Pukkala
E, Mellemkjaer L, Airio A, Evans SR and Felson DT: Frequency of
specific cancer types in dermatomyositis and polymyositis: A
population-based study. Lancet. 357:96–100. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Callen JP: Relation between
dermatomyositis and polymyositis and cancer. Lancet. 357:85–86.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Buchbinder R and Hill CL: Malignancy in
patients with inflammatory myopathy. Curr Rheumatol Rep. 4:415–426.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Detterbeck FC, Boffa DJ and Tanoue LT: The
new lung cancer staging system. Chest. 136:260–271. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dalakas MC: Inflammatory disorders of
muscle: Progress in polymyositis, dermatomyositis and inclusion
body myositis. Curr Opin Neurol. 17:561–567. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fathi M, Lundberg IE and Tornling G:
Pulmonary complications of polymyositis and dermatomyositis. Semin
Respir Crit Care Med. 28:451–458. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dalakas MC: Polymyositis, dermatomyositis
and inclusion-body myositis. N Engl J Med. 325:1487–1498. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Miller FW, Rider LG, Plotz PH, Isenberg DA
and Oddis CV: Diagnostic criteria for polymyositis and
dermatomyositis. Lancet. 362:1762–1763. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chow WH, Gridley G, Mellemkjaer L,
McLaughlin JK, Olsen JH and Fraumeni JF Jr: Cancer risk following
polymyositis and dermatomyositis: A nationwide cohort study in
Denmark. Cancer Causes Control. 6:9–13. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fujita J, Tokuda M, Bandoh S, Yang Y,
Fukunaga Y, Hojo S, Ueda Y, Dobashi N, Dohmoto K, Ishida T and
Takahara J: Primary lung cancer associated with
polymyositis/dermatomyositis, with a review of the literature.
Rheumatol Int. 20:81–84. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Andras C, Ponyi A and Constantin T:
Dermatomyositis and polymyositis associated with malignancy: A
21-year retrospective study. J Rheumatol. 35:438–444.
2008.PubMed/NCBI
|
|
14
|
Zang YS, Xiu QY, Fang Z, Li B and Xia TB:
Case report: Dramatic recovery of lung adenocarcinoma-associated
dermatomyositis with targeted lung cancer therapy alone.
Oncologist. 13:79–81. 2008. View Article : Google Scholar : PubMed/NCBI
|