Introduction
Metastatic carcinoma of the mandible is a rare
lesion that constitutes <1% of all oral malignancies (1). The primary tumors from which metastases
occur most commonly arise in the breasts, lungs and prostate
(1–3),
followed by the kidney, thyroid gland, liver, stomach, intestines,
testes and bladder (1,4–8). Surgeons
often have little experience with mandibular metastatic carcinomas,
hence, the majority of such tumors are mistakenly considered to be
new primary growths until histological examination reveals their
true metastatic nature (1,2). There are no clear differences in
histological findings between metastatic and primary lesions, and
the diagnosis of mandibular metastatic carcinoma is primarily based
on biopsy rather than radiographical or physical examination
(2,3).
Usually, segmental mandibulectomy surgery, radiotherapy and
chemotherapy are used to extend the survival time of patients,
although a significant extension of survival time has yet to be
achieved (9). However, a poor
prognosis is associated with these patients (2,3,9). In an early study conducted by Clausen
and Poulsen (3), 70 patients were
observed following the recognition of the jaw metastasis; in total,
49 of these patients succumbed to the disease within one year, 6
within 2 years and 2 within 4 years.
In order to provide a greater experience of this
condition, the present retrospective study was conduced to
investigate the clinical and computed tomography (CT) features of 6
patients with mandibular metastatic carcinomas, including the
surgical management options and follow-up outcomes.
Materials and methods
Patients
The medical records of 6 cases of mandibular
metastatic carcinoma obtained between October 17, 2002, and October
24, 2009 from the Ninth People's Hospital, Shanghai Jiao Tong
University School of Medicine (Shanghai, China), were
retrospectively reviewed. Only cases that reported the mandible
site and had histological confirmation were included in the present
study. The cases consisted of 4 women and 2 men, with an average
age of 66.3 years (range, 51–81 years). The origin of the lesions
was the prostate in 2 cases, the lungs in 2 cases, the breast in 1
case and the thyroid gland in 1 case (Table I).
 | Table I.Information on the 6 patients with
mandibular metastatic carcinoma. |
Table I.
Information on the 6 patients with
mandibular metastatic carcinoma.
| Case no. | Gender/age,
years | Site of tumor/size,
cm | Chief complaint | MT history | Computed tomography
scan | Pre-operative
diagnosis | Surgical mode | Pathological
diagnosis | Survival time,
months |
|---|
| 1 | M/73 | Body/5.0 | Pain, swelling, numb
chin | No | Osteoplastic lesion
and periosteal reaction | Osteosarcoma | Segmental
mandibulectomy | Metastatic prostatic
adeno-Ca | 49 |
| 2 | M/81 | Condyle/3.5 | Pain, swelling,
limitation of mouth opening | No | Osteoplastic lesion
and periosteal reaction | Osteosarcoma | Segmental
mandibulectomy | Metastatic prostatic
adeno-Ca | 60 |
| 3 | F/63 | Ascending
ramus/4.0 | Pain, swelling, numb
chin | Lung adeno-Ca | Osteolytic lesion and
periosteal reaction | Osteosarcoma or
metastatic carcinoma | Segmental
mandibulectomy | Metastatic lung
adeno-Ca | 12 |
| 4 | F/71 | Body/3.0 | Pain, swelling | No | Radiolucent
fibro-osseous lesion | Ameloblastoma | Enucleation | Metastatic lung
adeno-Ca | 8 |
| 5 | F/59 | Ascending
ramus/3.0 | Pain, swelling | No | Radiolucent
fibro-osseous lesion | Ameloblastoma | Segmental
mandibulectomy | Metastatic thyroid
adeno-Ca | 27 |
| 6 | F/51 | Body/4.0 | Pain, swelling, numb
chin | Ductal breast
cancer | Osteolytic lesion and
periosteal reaction | Osteosarcoma or
metastatic carcinoma | Segmental
mandibulectomy | Metastatic ductal
breast cancer | Lost to
follow-up |
Ethical approval was obtained from the Ethics
Committee of Ninth People's Hospital, Shanghai Jiao Tong University
School of Medicine [approval no., 2015(98)].
Treatment
Clinical examinations and CT scans were performed in
all 6 patients pre-operatively. With the exception of case 4, all
patients were treated with a segmental mandibulectomy and
post-operative chemoradiotherapy. The patient in case 4 was
reluctant to undergo a mandibulectomy, thus conservative
enucleation was used.
Diagnosis and follow-up
The post-operative pathological diagnoses were
formed using histological images and immunohistochemistry. The
post-operative follow-up period ranged from 8 to 60 months (mean,
31.2 months), which reflected the post-operative survival time.
Results
All 6 patients presented with mandibular pain and
bone swelling, 3 patients experienced a numb chin and 1 patient
presented with a limited degree of mouth opening. The patient in
case 3 had a history of lung adenocarcinoma, while case 6 had a
history of ductal breast cancer; each patient were surgically
treated 1.5 years prior to the current admission. Prior to
admission, the suspicion of primary recurrence was eliminated of
the two patients by examination with regard to the relevant
discipline. The remaining 4 patients had no history of malignant
tumors.
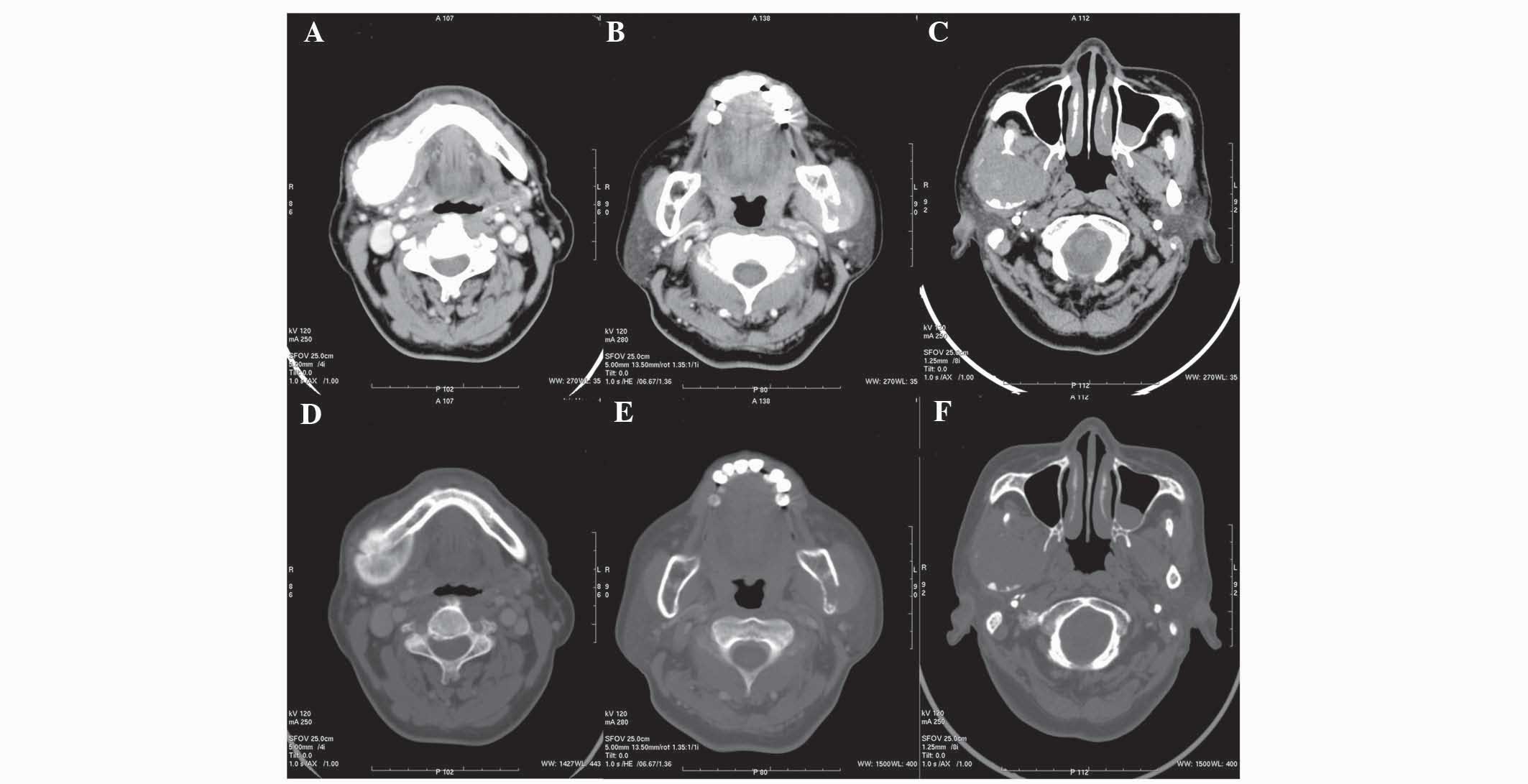
CT scans (Fig. 1)
showed that cases 1 and 2 exhibited osteoplastic lesions (Fig. 1A), while cases 3 and 6 presented with
osteolytic masses (Fig. 1B); all 4 of
these patients presented with the apparent radiographic feature of
a periosteal reaction, which was suggestive of osteosarcoma
(Fig. 1D and E). The tumors of the
other 2 patients (cases 4 and 5) appeared as expansive and
radiolucent masses, with the characteristics of fibro-osseous
lesions (Fig. 1C and F).
The pre-operative first diagnosis of the patients in
cases 1, 2, 3 and 6 was mandibular osteosarcoma. For cases 3 and 6,
considering their malignant history, metastatic carcinoma was
formed as the second diagnosis following pre-operative CT. The
other 2 patients (cases 4 and 5) were diagnosed with ameloblastoma
mainly based on the CT characteristics.
In total, 5 of the patients (cases 1, 2, 3, 5 and 6)
were surgically treated with an en bloc segmental mandibulectomy
with a margin of normal bone, and subsequent adjuvant therapy
consisting of radiotherapy and chemotherapy. For case 4, following
the enucleation of the lesion, an intraoperative rapid-frozen
biopsy provided the diagnosis of malignancy. However, a further
extensive osteotomy was refused by the patient's family.
Alternative chemoradiotherapy was selected instead. All patients
were advised to visit the relevant respective departments of the
hospital for further treatment of the primary site following
discharge from the Department of Oral and Maxillofacial
Surgery.
The pathological diagnosis of all 6 patients was
metastatic carcinoma. Cases 1 and 2 originated from the prostate
(Fig. 2A), with immunostaining of
prostate-specific antigen in the atypical cells confirming the
diagnosis of metastatic prostatic adenocarcinoma (Fig. 3A). Cases 3 and 4 originated from lung
adenocarcinoma; adenoid structures and columnar epithelial cells
with cellular nucleus division were observed (Fig. 2B). Case 5 originated from thyroid
adenocarcinoma (Fig. 2C), with
immunostaining testing positive for thyroglobulin in the cytoplasm
of the nests of tumor tissues (Fig.
3B). Case 6 originated from breast ductal cancer; a large
number of ductal carcinoma cell nests were surrounded by osseous
trabecular structures (Fig. 2D).
Patients from cases 1, 3, 4 and 5 succumbed to
cachexia caused by cancer recurrence or extensive metastasis during
the follow-up period. The patient from case 2 succumbed due to
cardiac disease 60 months after surgery, and case 6 was lost to
follow-up, thus a survival time could not be acquired.
Discussion
In total, <1% of mandibular malignancies are
metastatic lesions of a primary tumor originating in another region
of the body (1,2). However, the actual morbidity rate may be
even higher for the following reasons: i) Radiographic surveys of
the jaws are not routine; ii) certain precancerous lesions and
preinvasive carcinomas are hard to detect by radiographic
examination; and iii) the jaws are seldom examined during autopsy
(10–13).
Cases of primary carcinoma metastasizing to the
mandible were previously reviewed in a study by D'Silva et
al, which recorded the following primary sites: Breasts (25%),
lungs (13%), prostate (10%), colon (7%), thyroid gland (3%) and
kidneys (3%) (1). Metastasis of
maxillofacial bone carcinoma to distant regions occurs primarily
via the blood (2). However, there is
a much higher frequency of metastasis development in the mandible
compared with other maxillofacial bones (3,10). The
exact reason for this is unknown. The mandible is fed by the
terminal inferior alveolar artery, which is tightly encased by the
annular mandibular marrow cavity (14). Furthermore, the pathway of the
inferior alveolar artery traveling through the mandible is quite
long. We speculate that these anatomical features are more suitable
for the stagnation and gathering of tumor cells, and that the
nutrient-rich red active marrow within the mandible is eligible for
tumor proliferation.
In the present study, pain and swelling were the
most common symptoms of the mandibular malignancies, but the most
significant symptom was paresthesia of the chin. Nerve numbness has
a close association with malignant tumors (3,15).
Limitation of mouth opening was also found in the patient that
presented with a condylar metastasis (case 2) in the present study.
It should be noted that condylar metastasis with symptoms of
temporomandibular joint pain and limited mouth opening could mimic
temporomandibular disorders (TMD) (16–19). In
this case, clinicians should be aware of the differential diagnosis
of this tumor, particularly when patients have a history of
malignancy or respond to TMD-therapy inappropriately (19).
In general, the primary tumor is diagnosed prior to
the appearance of oral metastasis. However, in the present study, 4
out of the 6 cases experienced oral symptoms prior to diagnosis of
the primary site. Furthermore, in certain cases, the primary
malignancy remains undetected even though metastatic tumors of the
jaw have been pathologically diagnosed (1).
CT is the conventional diagnostic tool for
mandibular metastatic lesions (6). In
the current study, the 2 prostatic metastatic cases presented with
osteoplastic lesions, while others showed osteolytic change. A
‘sunburst’ periosteal reaction was observed in 4 lesions and the
other 2 lesions showed a well-demarcated radiolucent fibro-osseous
lesion. However, the diagnosis of mandibular metastatic carcinoma
can be difficult to make based solely on CT features. For cases 3
and 6, due to the history of malignancy, the possibility of
metastatic carcinoma was considered in the differential diagnosis,
however, it was thought more likely that the lesion was a primary
osteosarcoma according to the CT results.
The differential diagnosis for mandibular metastatic
carcinoma includes TMD, ameloblastoma, primary intraosseous
squamous carcinoma, and particularly, osteosarcoma (2,16,17,20,21). The
past medical history, symptoms, clinical examination, and CT or
magnetic resonance imaging (MRI) results of a patient should be
carefully investigated. For patients with a history of malignancy,
metastatic carcinoma must be considered in the differential
diagnosis. As CT or MRI scans can provide uncharacteristic
findings, biopsy is an essential and indispensable tool for forming
a diagnosis (3). Additionally, if
surgeons suspect that there is a possibility of metastases, then
positron emission tomography (PET)/CT maybe required (22). PET/CT is usually an effective
diagnostic tool for metastatic carcinoma, with the shortcoming of
this equipment being its low popularity in developing regions.
Mandibular metastatic carcinoma is associated with a
poor prognosis. The majority of patients diagnosed with oral
metastasis succumb to the disease within 1 year, while the 4-year
survival rate is estimated to be 10% (3,23). The
main purpose of therapy is to relieve pain and extend the survival
time. In the present study a collaborative therapeutic schedule
that included surgical, chemical and radioactive treatment was
recommended. Following this integrated therapy, and combined with
androgen deprivation, the 2 patients in the prostatic metastatic
cases achieved survival times of >4 years. By contrast, the
patient in case 4 who rejected the extensive osteotomy succumbed to
cachexia 8 months later. It should be noted that if extensive
metastases have been detected pre-operatively or if the patient is
in a bad general condition, palliative care may be the sensible
choice.
As the general prognosis of such patients is rather
poor, intraoperative immediate mandible reconstruction by bone
transplantation, including fibular or iliac bone flaps, should be
avoided to alleviate the risks and repercussions associated with
surgery.
In conclusion, the diagnosis of mandibular
metastatic carcinoma is rather difficult, particularly for patients
who develop oral symptoms prior to the diagnosis of the primary
site and in whom there is no history of malignancy. A poor
prognosis is associated with these patients. To extend the survival
time of such patients, a treatment strategy using multiple
therapies, including segmental mandibulectomy, radiotherapy and
chemotherapy, is recommended.
References
|
1
|
D'Silva NJ, Summerlin DJ, Cordell KG,
Abdelsayed RA, Tomich CE, Hanks CT, Fear D and Meyrowitz S:
Metastatic tumors in the jaws: A retrospective study of 114 cases.
J Am Dent Assoc. 137:1667–1672. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bigelow NH and Walsh TS: Metastatic
carcinoma of the mandible. Ann Surg. 137:138–140. 1953. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Clausen F and Poulsen H: Metastatic
carcinoma to the Jaws. Acta Pathol Microbiol Scand. 57:361–374.
1963. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jones GM, Telfer MR and Eveson JW:
Metastatic renal clear cell carcinoma of the jaws. Two cases
illustrating clinical and pathological diagnostic problems. Br J
Oral Maxillofac Surg. 28:172–175. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ismail SB, Abraham MT, Zaini ZB, et al:
Metastatic follicular thyroid carcinoma to the mandible: A case
report. Cases J. 2:65332009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kamatani T, Tatemoto Y, Tateishi Y and
Yamamoto T: Isolated metastasis from hepatocellular carcinoma to
the mandibular condyle with no evidence of any other metastases: A
case report. Br J Oral Maxillofac Surg. 46:499–501. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Uchiyama Y, Murakami S, Kakimoto N,
Nakatani A, Kishino M, Hamab Y and Furukawa S: Diagnostic imaging
findings for mandibular metastasis from gastric adenocarcinoma.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 107:e49–e53.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Babu KG, Raud C, Kumaraswamy SV and
Lalitha N: Carcinoma colon with mandible and liver metastases. Br J
Oral Maxillofac Surg. 34:133–134. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nishikawa H, Nakashiro K, Sumida T, Sugita
A and Hamakawa H: Mandibular osteoblastic metastasis of poorly
differentiated carcinoma of the thyroid gland. Int J Oral
Maxillofac Surg. 39:301–304. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Freudlsperger C, Kurth R, Werner MK,
Hoffmann J and Reinert S: Condylar metastasis from prostatic
carcinoma mimicking temporomandibular disorder: A case report. Oral
Maxillofac Surg. 16:79–82. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Buchner A and Ramon Y: Distant metastases
to the jaws: Report of four cases. J Oral Surg. 25:246–250.
1967.PubMed/NCBI
|
|
12
|
Cash CD, Royer RQ and Dahlin DC:
Metastatic tumors of the jaws. Oral Surg Oral Med Oral Pathol.
14:897–905. 1961. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Neville BW and Day TA: Oral cancer and
precancerous lesions. CA Cancer J Clin. 52:195–215. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim ST, Hu KS, Song WC, Kang MK, Park HD
and Kim HJ: Location of the mandibular canal and the topography of
its neurovascular structures. J Craniofac Surg. 20:936–939. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Orhan K, Bayndr H, Aksoy S, Seker BK,
Berberoğlu A and Ozan O: Numb chin syndrome as a manifestation of
possible breast cancer metastasis around dental implants. J
Craniofac Surg. 22:942–945. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tabib R, Elias S, Tal Y, Ben-Yehuda A and
Abu-Tair J: Temporomandibular joint-related symptoms as initial
presentation of lung carcinoma in a patient with Takayasu's
arteritis. J Oral Maxillofac Surg. 69:226–229. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Qiu YT, Yang C, Chen MJ and Qiu Wl:
Metastatic spread to the mandibular condyle as initial clinical
presentation: Radiographic diagnosis and surgical experience. J
Oral Maxillofac Surg. 71:809–820. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kelles M, Akarcay M, Kizilay A and
Samdanci E: Metastatic renal cell carcinoma to the condyle of the
mandible. J Craniofac Surg. 23:e302–e303. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kruse AL, Luebbers HT, Obwegeser JA,
Edelmann L and Graetz KW: Temporomandibular disorders associated
with metastases to the temporomandibular joint: A review of the
literature and 3 additional cases. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 110:e21–e28. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tchan MC, George M and Thomas M:
Metastatic prostate cancer mimicking primary osteosarcoma of the
jaw: An infrequent clinical case. South Med J. 101:657–659. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yagan R, Bellon EM and Radivoyevitch M:
Breast carcinoma metastatic to the mandible mimicking
ameloblastoma. Oral Surg Oral Med Oral Pathol. 57:189–194. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cheung PK, Chin RY and Eslick GD:
Detecting residual/recurrent head neck squamous cell carcinomas
using PET or PET/CT: Systematic review and meta-analysis.
Otolaryngol Head Neck Surg. Dec 29–2015.(Epub ahead of print).
PubMed/NCBI
|
|
23
|
Kesting MR, Loeffelbein DJ, Hölzle F,
Wolff KD and Ebsen M: Male breast cancer metastasis presenting as
submandibular swelling. Auris Nasus Larynx. 33:483–485. 2006.
View Article : Google Scholar : PubMed/NCBI
|