Introduction
Choriocarcinoma of non-placental origin is highly
malignant and is mainly characterized by the production of large
amounts of human chorionic gonadotropin (HCG) hormones (1). The disease is extremely rare,
particularly in male patients, and there are few studies on such
cases (2). The present study reports
the case of a 26-year-old male patient with choriocarcinoma,
providing a firsthand opportunity to review the specific features
of the disease, including rapid and multiple metastasis, a high
level of β-HCG, and the associated life-threatening effects.
Case report
In March 2013, a 26-year-old male with a 4-day
history of headache, moderate fever and numbness in the right upper
limb was diagnosed with a cerebral hemorrhage by computed
tomography (CT) scan at The General Hospital of the Second
Artillery Corps of Chinese PLA (Beijing, China). On the same day,
the patient was transferred to Beijing Friendship Hospital, Capital
Medical University (Beijing, China) due to the identification of
multiple undefined lesions in the lungs by X-ray. The patient did
not have any chronic illness and lived in a house with two pets, a
python and a dog, suggesting the possibility of a parasitic
disease.
Upon examination, it was observed that the patient
had normal vital signs with a Glasgow coma scale of 14. No palpable
enlargement of the lymph nodes or lumps beneath the skin were
observed, however, superficial sensation was slightly impaired.
Muscle strength of the right upper limb was measured at level 4,
according to manual muscle testing (3), and the right Babinski sign was positive.
The patient's testes were also examined, but no abnormalities were
found.
Chest X-ray and chest CT scans showed multiple
lesions in the lungs (Fig. 1).
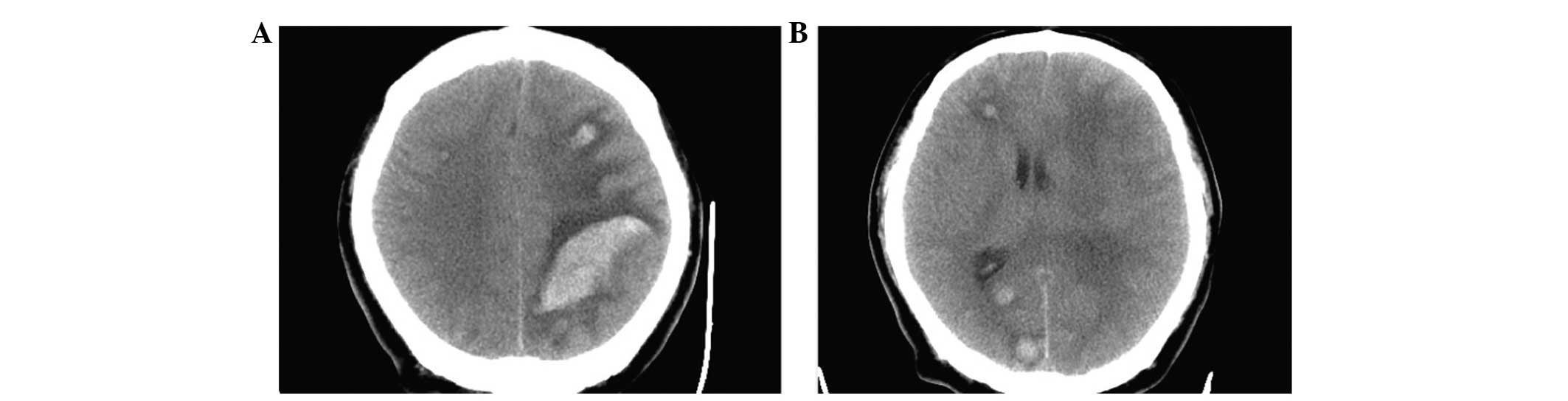
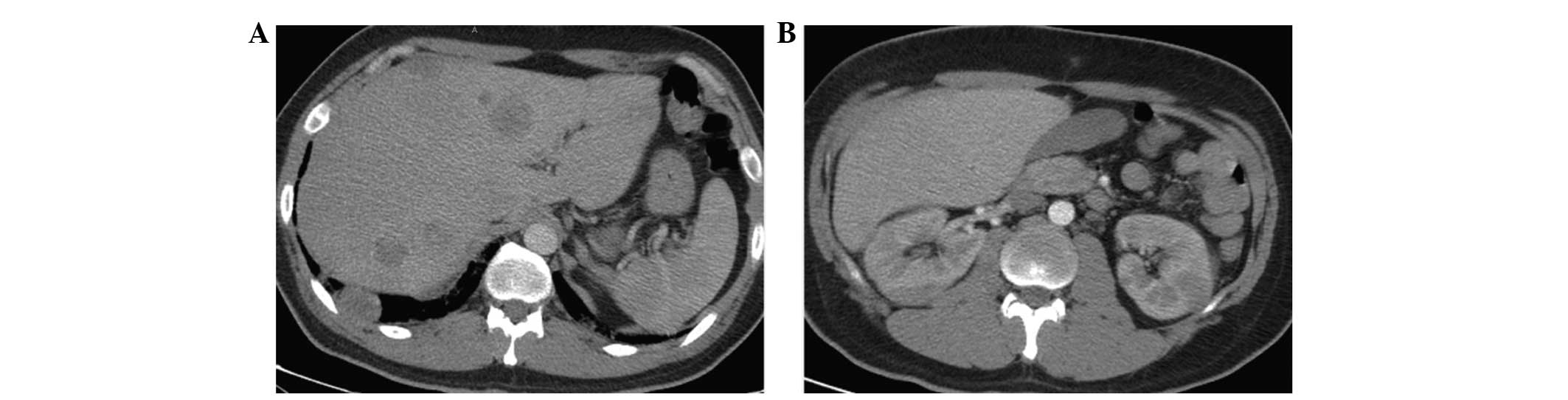
Furthermore, CT scans also showed multiple tumors in the head,
liver and kidneys (Figs. 2 and
3). The laboratory results were as
follows: White blood cell count, 16.59×109/l (normal,
4–10×109/l); hemoglobin, 131 g/l (normal, 120–160 g/l);
platelets, 277×109/l (normal, 100–300×109/l);
C-reactive protein, 132 mg/l (normal, 0–8 mg/l); alanine
aminotransferase, 93 U/l (normal, 0–40 U/l); total bilirubin, 25.6
µmol/l (normal, 3.42–17.1 µmol/l); direct bilirubin, 16.62 µmol/l
(normal, 0–6.84 µmol/l) and albumin, 25.7 g/l (normal, 35–55 g/l).
Parameters for blood electrolytes and renal function were within
normal limits. For the differential diagnosis, tests were performed
for angiotensin-converting enzyme (ACE), a few parasite specific
antibodies (echinococcosis antibody, trichinosis antibody,
schistosoma antibody and liver fluke antibody) and serum tumor
markers. The presence of ACE within the normal range ruled out
sarcoidosis. A negative result for the specific antibodies for
echinococcosis, trichinosis, schistosoma and liver flukes ruled out
the possibility of parasitic diseases. Moreover, the cancer
biomarkers of α-fetoprotein, carbohydrate antigen (CA)125 and CA199
were detected at normal levels. However, the levels of
carcinoembryonic antigen, cytokeratin fragment 21–1 (CYF211) and
neuron-specific enolase (NSE) were higher than normal (Table I). Most noticeably, the β-HCG level
was much higher than normal (>200,000 mIU/ml; normal, 0–25
mIU/ml), as shown in Table I. This
reinforced the suspicion of a malignant tumor. An ultrasound-guided
Tru-Cut biopsy of the liver was performed to confirm this
diagnosis.
 | Table I.Patient's serum tumor markers. |
Table I.
Patient's serum tumor markers.
| Component | Value | Reference range |
|---|
| CEA, ng/ml | 3.42 | 0.00–5.00 |
| AFP, ng/ml | 4.11 | 0.00–15.00 |
| CA199, U/ml | 27.99 | 0.00–37.00 |
| CYF211a, ng/ml | 29.00 | 0.10–3.30 |
| NSEa, ng/ml | 39.36 | 0.00–16.30 |
| CA125a, U/ml | 76.60 | 0.00–35.00 |
| β-HCGb, mIU/ml | >200,000 | 0–25 |
In the meantime, the neurosurgeon suggested a
conservative treatment, as it was believed that the prognosis could
not be improved by surgery. Mannitol (0.5 g by intravenous drip
every 8 h) was administered to the patient to reduce intracranial
pressure. In addition, due to pyrexia and a high white blood cell
count, cefoperazone sodium and sulbactam sodium were administered
by injection (3.0 g by intravenous drip every 12 h) to empirically
fight infection. However, the patient's physical condition
continued to deteriorate. After the third day of hospitalization,
the patient developed a brain hernia, and finally, on the fourth
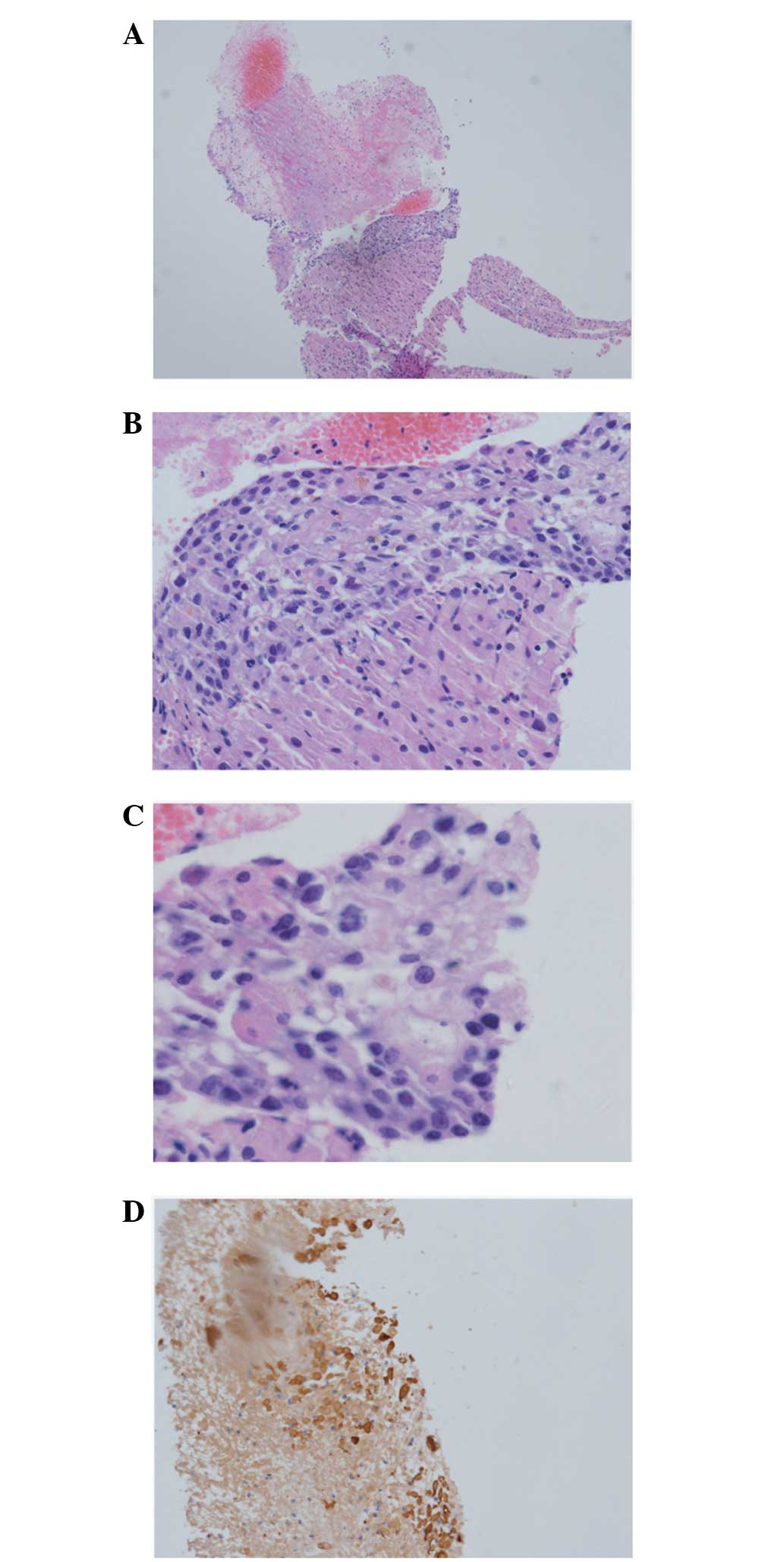
day, the patient succumbed. Following this, the ultrasound-guided
Tru-Cut liver biopsy result was received and it was established
that the carcinoma originated from the epithelial tissue (Fig. 4), thus supporting the diagnosis of
choriocarcinoma.
Discussion
It is known that the majority of choriocarcinomas
are placental choriocarcinomas, which always occur in females
following gestational events such as molar pregnancy, normal or
ectopic pregnancy, and abortion (1).
Choriocarcinoma from non-placental origin is a rare disease,
especially in male patients (4). A
search of PubMed using keywords such as ‘choriocarcinoma,
non-gestational’ and ‘male’, revealed only ~20 studies, and almost
all of these were case reports. This further emphasizes the
rareness of the carcinoma.
The 26-year-old patient in the present study was
diagnosed with intracranial hemorrhage as the first symptom.
Multiple lesions were then found in the lungs, liver and kidneys.
Notably, no abnormalities were observed in the testicular physical
exam. Choriocarcinoma usually undergoes vascular invasion and
easily causes metastatic bleeding (4,5). A study
by Baagar et al described choriocarcinoma syndrome as the
hemorrhage of the tumor at its metastatic site. A case was reported
in which a patient succumbed from the hemorrhage of a liver
metastasis (5). There is no effective
therapeutic treatment for choriocarcinoma syndrome, as it has
already metastasized by the time it is diagnosed, and it is too
late for the patient to undergo surgery.
In the present case, lesions were identified in the
brain, lungs, liver, kidneys and skin. The presence of multiple
lesions in the lung was particularly unique. It is extremely
difficult to determine the location of the original carcinoma in
patients where multiple organs are involved. When the present
patient was first admitted, parasitic infections were tested for
first due to a close proximity with dogs and snakes, and as the
patient was also an animal breeder. Therefore, parasitic infections
such as echinococcosis, trichinosis, schistosoma and liver flukes
were first ruled out. In addition, the patient's ACE levels were
also determined to rule out sarcoidosis. Furthermore, the
possibility of metastatic carcinoma, particularly those originating
from the reproductive system, was considered. However, testicular
examination did not find any abnormalities. Finally, after
detecting high levels of β-HCG, the possibility of a rare carcinoma
was considered. Later, a liver biopsy provided further evidence
that confirmed this diagnosis.
The HCG hormone is a characteristic marker of
choriocarcinoma. A literature review by Yokoi et al reported
that 96.4% of choriocarcinoma patients had abnormal elevated serum
β-HCG levels (4). Jiang et al
suggested that serum β-HCG levels could be used as a marker to
assess the effectiveness of treatment (6). Since choriocarcinoma cells express high
levels of HCG, we hypothesize that HCG levels may have a certain
association with prognosis. A higher HCG level would correspond
with a poor prognosis, but this hypothesis would require large
samples to test it further. Other tumor markers in the present
patient, including CA125, CYF211 and NSE, were exhibited at
elevated levels, but the causes and significance of these increased
levels are unknown.
It has also been reported that choriocarcinoma
patients could develop paraneoplastic syndromes such as
hyperthyroidism (4,7,8). However,
in the present case, thyroid function could not be checked due to a
delayed diagnosis and the rapid deterioration of the patient's
condition.
There have been no reports that describe a perfect
treatment plan for choriocarcinoma of non-placental origin. Early
tumor resection is believed to be an effective method (9). However, the best time for surgery is
always missed when carcinoma is identified due to the high degree
of malignancy and early bleeding. Thereafter, the only option left
is conservative treatment such as chemotherapy, which includes
treatment with drugs such as etoposide, cisplatinum, methotrexate,
actinomycin D, bleomycin, 5-fluorouracil, VP-16, cyclophosphamide
and vincristine (10–12). However, these drugs are only partially
effective, as the majority of patients succumb within a short
follow-up time. Guo et al reported one case of intracranial
choriocarcinoma that was treated using radiotherapy, in which
patient survived for ~6 months (13).
However, this was only an individual case, and there has been no
evidence of a large number of cases showing the effectiveness of
conservative treatment. Only symptomatic treatments, such as
hydration and anti-infection treatments, were administered to the
present patient due to delayed diagnosis, however, we suggest that
a patient should be given chemotherapeutic treatment as soon as a
malignant tumor is suspected.
Choriocarcinoma of non-placental origin is a highly
malignant carcinoma with poor prognosis. The present patient serves
as a typical example to this effect, since multi-organ metastasis
was observed, the symptoms were only displayed for 4 days prior to
admission and the patient succumbed after the fourth day of
admission. Similarly, based on literature reviews, the majority of
patients succumb to organ bleeding, respiratory failure,
hemorrhagic shock, disseminated intravascular coagulation and
abdominal compartment syndrome (11).
The occurrence of liver or brain metastases is associated with a
worse prognosis (14).
In conclusion, the typical symptoms of multiple
space-occupying lesions in different organs and accompanying high
HCG levels point towards the possible diagnosis of choriocarcinoma
of non-placental origin. This disease is life-threatening and
should be diagnosed and treated as soon as possible.
Acknowledgements
This study was sponsored by the National Natural
Science Funds of China (grant no. 813740041020795).
References
|
1
|
Smith HO, Kohorn E and Cole LA:
Choriocarcinoma and gestational trophoblastic disease. Obstet
Gynecol Clin North Am. 32:661–684. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kyriakou F, Vaslamatzis MM, Bastani S,
Lianou MA, Vourlakou C and Koutsoukou A: Primary choriocarcinoma of
the renal pelvis presenting as intracerebral hemorrhage: A case
report and review of the literature. J Med Case Rep. 5:5012011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hislop H, Avers D and Brown M: Daniels and
Worthingham's Muscle Testing: Techniques of Manual Examination and
Performance Testing (9th). Elsevier. India: 2013.
|
|
4
|
Yokoi K, Tanaka N, Furukawa K, Ishikawa N,
Seya T, Horiba K, Kanazawa Y, Yamada T, Ohaki Y and Tajiri T: Male
choriocarcinoma with metastasis to the jejunum: A case report and
review of the literature. J Nippon Med Sch. 75:116–121. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Baagar K, Khan FY and Alkuwari E:
Choriocarcinoma syndrome: A case report and a literature review.
Case Rep Oncol Med. 2013:6972512013.PubMed/NCBI
|
|
6
|
Jiang L, Wu JT and Peng X: Primary
choriocarcinoma of the colon: A case report and review of the
literature. World J Surg Oncol. 11:232013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Heda P and Cushing G: Testicular
choriocarcinoma presenting as hyperthyroidism. Am J Med. 126:e1–e2.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
McCracken EJ, Johnston PC, Lindsay JR,
Mulholland C, McAleer JJ and Black RN: Testicular choriocarcinoma:
An unusual case of paraneoplastic thyrotoxicosis. QJM. 105:675–677.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bolze PA, Attia J, Massardier J, Seckl MJ,
Massuger L, van Trommel N, Niemann I, Hajri T, Schott AM and
Golfier F: EOTTD group: Formalised consensus of the European
Organisation for Treatment of Trophoblastic Diseases on management
of gestational trophoblastic diseases. Eur J Cancer. 51:1725–1731.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Waseda Y, Komai Y, Yano A, Fujii Y,
Noguchi N and Kihara K: Pathological complete response and two-year
disease-free survival in a primary gastric choriocarcinoma patient
with advanced liver metastases treated with germ cell tumor-based
chemotherapy: A case report. Jpn J Clin Oncol. 42:1197–1201. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hadgu A, Tindni A and Panda M: Primary
pulmonary choriocarcinoma in a male. BMJ Case Rep.
2010:bcr02201027122010.PubMed/NCBI
|
|
12
|
Oshima J, Uemura M, Kato T, Nagahara A,
Kiuchi H, Tsujimura A and Nonomura N: Modified BEP regimen leads to
abatement of choriocarcinoma syndrome in a patient with extra
gonadal germ cell tumor: A case report. Hinyokika Kiyo. 60:183–187.
2014.(In Japanese). PubMed/NCBI
|
|
13
|
Guo J, Zhong C, Liu Q, Xu J, Zheng Y, Xu
S, Gao Y, Guo Y, Wang Y, Luo Q and Jiang J: Intracranial
choriocarcinoma occurrence in males: Two cases and a review of the
literature. Oncol Lett. 6:1329–1332. 2013.PubMed/NCBI
|
|
14
|
Chapman GW Jr: Metastatic intracerebral
choriocarcinoma in a teenager. J Natl Med Assoc. 89:758–760.
1997.PubMed/NCBI
|