Introduction
According to the World Health Organization,
cementoblastoma is classified as a benign odontogenic tumor
(1). The majority of patients exhibit
no marked clinical signs, with the tumors often being identified
following orthopantomography. Typical treatment of cementoblastoma
includes the complete removal of the lesion with extraction of the
associated tooth (2); however,
certain patients may decide against surgery, undergoing follow-up
alone. Osteosarcoma is a non-hematopoietic, malignant tumor of the
bone, with the neoplastic cells of the lesion producing osteoid
(3). This form of tumor is
characterized by high malignancy, metastasis and mortality rates
(4). The tumors are most prevalently
located in the metaphyseal region of long bones, particularly in
the knee and pelvis (5). Osteosarcoma
of the jaw is rare, accounting for 5–13% of all osteosarcoma cases
(6), the majority of which are
located in the mandible. Until recently, the etiology of
osteosarcoma of the jaw has remained obscure. In a series of
patients, a greater number of differences in gender, tumor subtype
and metastatic potential of osteosarcoma of the jaw were noted than
previously observed, and better imaging, earlier diagnosis and more
aggressive treatment has been indicated to improve the surgical
clearance of the tumor (7). The
current study reports the case of a young female presenting with an
unusual swelling in the left mandible.
Case report
In December 2012, a 20-year-old female presented
with a 2-year history of swelling in the left mandible, without
pain or any discomfort. The only accompanying symptom was tooth
mobility of the molars. At 1 month prior to presentation, the
swelling had progressed at an increased rate, and was associated
with significant pain and numbness. The patient was initially
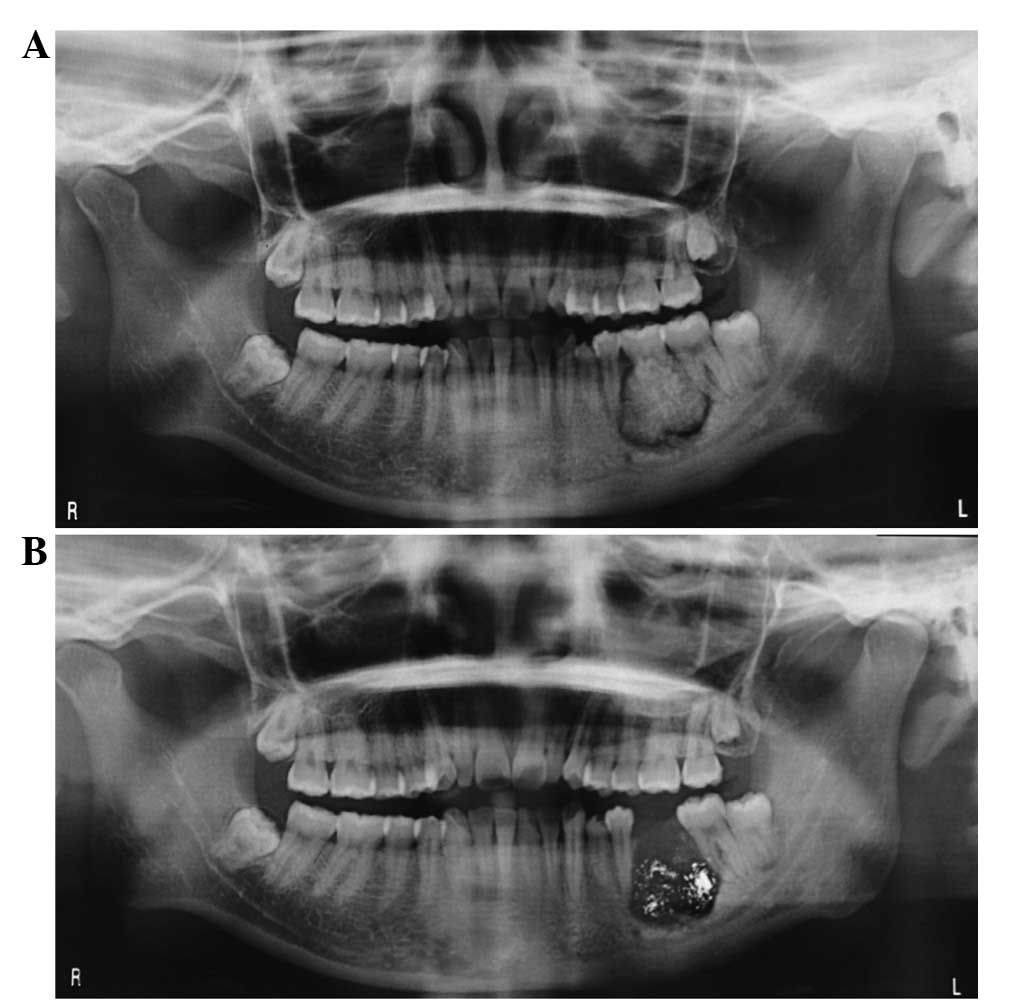
examined by a dentist who performed an orthopantomography
examination. The resulting images exhibited a well-defined,
high-density change of the alveolar ridge surrounding the first
left mandibular molar, with a peripheral radiolucent band.
Following orthopantomography (ORTHOPHOS XG 5 DS/Ceph; Sirona Dental
Systems GmbH, Bensheim, Germany), the initial clinical diagnosis
was stated as cementoblastoma (Fig.
1). As the leading treatment for cementoblastoma, extraction of
the first left mandibular molar was performed. Subsequent to the
diagnosis and molar removal, the patient was transferred to the
Department of Oral Maxillofacial Head and Neck Oncology, Ninth
People's Hospital (Shanghai, China), for further treatment. A
physical examination identified that the lesion was a 2.5×2.5-cm
solid swelling on the left mandible, with the primary expansion
observed on the buccal cortical plate (Fig. 2). No enlarged lymph node was noted in
the cervicofacial chain. Further orthopantomography was performed,
and detected that the region of radiolucency, with a rough margin,
involved the roots of the second premolar and the second molar.
Certain high-density spots were identified in the radiolucent area
(Fig. 1). A chest radiograph appeared
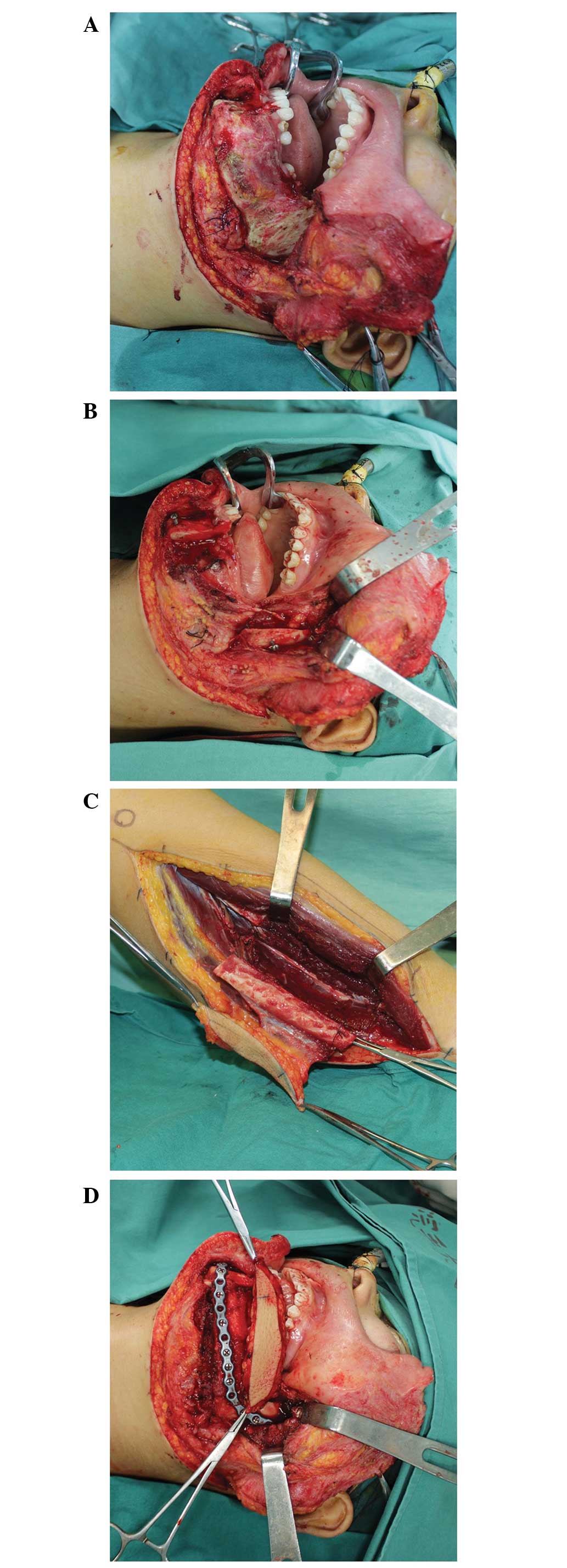
to reveal no suspicious abnormalities. The patient underwent a left
total mandibulectomy with reconstruction using a vascularized
fibular osteocutaneous flap and titanium plate (Fig. 3). The tumor exhibited typical
characteristics of osteosarcoma, including the compact bone and
trabecula-like structures surrounded by abundant active
osteoblasts, with the final pathology confirming the lesion to be
sclerosing osteosarcoma (Fig. 4). No
radiotherapy or chemotherapy was administered to accompany the
radical surgical. The patient recovered well and was discharged 14
days after surgery without any other complications. At a 6-month
follow-up examination, the patient exhibited normal occlusion and
oral commissure (Figs. 5 and 6), and no recurrence or metastasis was
observed during 2 years of follow-up, using enhanced CT scans of
the head, neck and chest regions.
Discussion
True cementoma, now known as cementoblastoma, is a
benign odontogenic tumor commonly presenting with painful swelling
of the alveolar ridges (1). Such
lesions have a predilection for the mandible and are primarily
associated with the mandibular first molar. The pulp vitality of
the involved teeth generally remains intact. Cementoblastoma is
most commonly observed in males at a mean age of 21 years (8). The majority of patients are usually
entirely asymptomatic, and diagnosis is often made according to
X-ray observations. Certain patients experience swelling, pain,
tooth mobility, paresthesia or cortical expansion of the mandible.
In the current case, the only initial clinical sign of the disease
was swelling. The imaging data obtained from the patient's dentist
appeared to be similar to the radiographical appearance of
cementoblastoma, which includes the formation of hard-tissue in
connection with the root of a tooth, a definite boundary, a
radiopaque or mixed-density and a thin surrounding radiolucent zone
(1). In the present case, 1 month
prior to presentation, the mandibular began to swell at an
increased rate, the pain was also increasing and numbness was
experienced. An important detail was later noted to have been
overlooked in the initial orthopantomography; the roots of the
involved tooth had been eroded by the tumor and presented an
incomplete structure of the teeth. When combined with the patient
symptoms, this finding meant that concern was raised over the
diagnosis of cementoblastoma.
Osteosarcoma is a malignancy of mesenchymal cells
and commonly occurs in the long bones. Osteosarcoma of the jaw is
rare, accounting for ~1% of all head and neck malignancies
(9). The disease has a moderate male
predilection, with a peak in incidence in the second to third
decades of life (10). The maxilla
and the mandible are affected almost equally, with the alveolar
ridge and the antrum in the maxilla and the body of the mandible
serving as preferential sites for the tumors. A number of risk
factors are understood to be associated with osteosarcoma,
including genetic bias, Paget's disease of the bone, hereditary
retinoblastoma, trauma, a history of fibrous dysplasia, chromic
oxide and radiation (11). However,
the disease etiology remains unclear.
Clinical symptoms of osteosarcoma of the jaw include
swelling (with or without pain) and loosening of the teeth. Certain
well-differentiated tumors grow slowly and present as benign
lesions. As a malignant tumor, osteosarcoma is invasive, and may
cause irreversible numbness if the neoplasm invades the inferior
alveolar nerve (10). This form of
numbness is dissimilar to the paresthesia experienced by patients
with cementoblastoma, which is caused by tumor pressure.
Occasionally, laboratory parameters have demonstrated an increase
in alkaline phosphatase or lactic dehydrogenase in serum levels
(12), with such unfavorable serum
parameters considered to indicate a poor prognosis for patients
with osteosarcoma.
In general, the radiographical appearance of
osteosarcoma of the jaw relies on three processes: i) Bone
formation and mineralization; ii) bone destruction; and iii)
periosteal bone formation. In the majority of cases, the tumor is a
mixed lytic/blastic lesion that is dependent on the degree of
ossification (13). During the early
stage of osteosarcoma, the observation of a widened periodontal
ligament space and inferior dental canal is typical of the disease,
however, it is extremely difficult to recognize (14). In certain cases, the typical ‘sunray’
appearance may be observed at the periphery of the tumor in plain
radiographs and computed tomography scans. The hallmark of
cementoblastoma is the sharp border between the tubular dentin of
the root and the cementum-like component (15). In the present case, the osteosarcoma
resembling cementoblastoma mimicked ‘benign’ bone growth, and there
was no observation of the typical ‘sunray’ radiographical
appearance. It was noted, however, that the tumor exhibited an
irregular shape with a rough margin. The roots of the first molar
and the mandibular canal were invaded by the tumor. The structure
of the root canal was destroyed, and the wall of the mandibular
canal was discontinuous.
Macroscopically, certain osteoblastic osteosarcomas
tend to be grey-tan and randomly granular, while others become
denser, sclerotic and more yellow-white (16). Histopathologically, the observation of
osteoid is key for the diagnosis of osteosarcoma. Osteoid is a
pink, dense, intercellular material that is curvilinear with small
nubs and arborization (Fig. 4)
(16). Sclerosing osteosarcoma is a
subtype of osteoblastic osteosarcoma that presents with compact
osteoid and bone within the tumor; certain studies have reported
that the deposition of bone matrix occurs between adipocytes in the
marrow cavity (16). As lesions are
typically decalcified, the immature bone surrounded by adipocytes
may be obscured (17). In certain
cases, the osseous matrix may be deposited on the normal bone
trabeculae, and the tumor cells may be small, pyknotic and
surrounded by large amounts of bone matrix; this phenomenon is
known as ‘normalization’ (16). When
compared with the pathological characteristics of osteosarcoma,
cementoblastoma is composed of sheets of cementum and peripheral
radiating columns of unmineralized tissue, similar to normalization
(18). For this reason, it is
difficult to distinguish between cementoblastoma and osteosarcoma
when only a small tissue specimen is available. A further feature
of osteosarcoma is the variable amounts of cartilage matrix and
fibrous tissue. In the present case, the tumor exhibited typical
characteristics of osteosarcoma; it was composed of compact bone,
trabecula-like structures, which were surrounded by abundant active
osteoblasts with varying morphology and atypical nuclear fission,
fibrous connective tissue and an infective lesion.
If the diagnosis of the current case were
cementoblastoma, the optimal treatment would have been dental
extraction and post-operative follow-up. Certain patients that
present with no clinical signs may not decide to undergo surgery
and instead undergo follow-up examinations alone. However, if a
patient with osteosarcoma misdiagnosed as cementoblastoma underwent
a dental extraction, the tumor would undergo rapid growth (19).
Without aggressive intervention, osteosarcoma of the
jaw may be fatal, and prompt radical resection is currently the
preferred treatment. Extensive resection requires surgeons to
remove the tumor with a 1.5–2 cm margin. It has previously been
reported that the 5-year survival rate of patients with
osteosarcoma of the mandible is 34.8% and that of the maxilla is
25.8% (20). Age serves as a
prognostic factor of osteosarcoma, with older patients
demonstrating a more favorable prognosis when compared with younger
patients (21). Local recurrence and
metastasis may also present in patients. Metastasis generally
occurs via the bloodstream, and most frequently arises in the lungs
(22). Regional lymph node metastasis
is rarely observed. Metastasis occurs in only 18% of patients with
osteosarcoma of the jaw, and it has been reported that men are
affected more commonly (21). Using
an immunomagnetic detection assay, Bruland et al (23) examined blood and bone marrow samples
from 60 patients who were suspected of having osteosarcoma. It was
demonstrated that this type of technique may be successfully used
to detect metastasis in cases of osteosarcoma. In the present case,
the chest radiograph did not detect any metastases. At a 2-year
follow-up examination, the patient demonstrated no signs of local
recurrence or metastasis.
A large amount of controversy surrounds the
performance of post-operative radiotherapy and chemotherapy. Due to
the anatomical circumstances in the craniofacial region, it is
challenging to achieve a tumor-free surgical resection margin. The
majority of scholars consider that patient survival time is limited
if the osteosarcoma is treated by ablative surgery alone. However,
other studies have suggested that extensive resection alone is
sufficient, with the 5-year survival rate of patients who underwent
resection recorded at ~60% (24,25). It is
considered that radiotherapy should be confined to the treatment of
unresectable, residual and recurrent tumors, as radiotherapy itself
is a risk factor for osteosarcoma. From the results of previous
studies, it cannot be confirmed whether chemotherapy has an effect
on the prognosis of patients with osteosarcoma (26,27); this
may be due to the diversity in chemotherapy regimens that were
administered. A number of previous studies reported that modern
adjuvant chemotherapy increased the survival time of patients, and
in certain cases, also controlled metastasis (10).
Cementoblastoma is a type of benign odontogenic
tumor, with the optimal treatment consisting of tooth extraction
and follow-up examination. Osteosarcoma of the jaw is a rare,
malignant disease with a poor prognosis, and the imaging and
clinical appearance of the lesion is highly variable. The preferred
treatment options include a segmental mandibulectomy or
maxillectomy, whilst post-operative radiotherapy and chemotherapy
is controversial. Due to the opposing biological behavior
underlying the two diseases and varying prognoses, it is important
that surgeons are able to distinguish between osteosarcoma and
cementoblastoma. The current case presented with sclerosing
osteosarcoma, which originated from the mandible, and resembled a
cementoblastoma. The findings discussed in the present study aim to
provide a clearer understanding of the distinguishing features of
osteosarcoma and cementoblastoma, and possibly aid their
differentiation in the clinic.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (grant no. 81271112), the
Development Foundation supported by the Shanghai Municipal Human
Resources and Social Security Bureau (grant no. 201312), and the
Southern Management Corporation Rising Star Scholar, supported by
Shanghai Jiao Tong University (grant no. 2013SMC-A-4).
References
|
1
|
van der Waal I: Cementoblastoma. In: World
Health Organization Classification of Tumours. Pathology and
Genetics of Head and Neck Tumours. Barnes L, Eveson JW, Reichart P
and Sidransky D: IARC Press. (Lyon). 3182005.
|
|
2
|
Sharma N: Benign cementoblastoma: A rare
case report with review of literature. Contemp Clin Dent. 5:92–94.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Amaral MB, Buchholz I, Freire-Maia B,
Reher P, de Souza PE, de Marigo HA, Martins CR and Horta MC:
Advanced osteosarcoma of the maxilla: A case report. Med Oral Patol
Oral Cir Bucal. 13:E492–E495. 2008.PubMed/NCBI
|
|
4
|
Nthumba PM: Osteosarcoma of the jaws: A
review of literature and a case report on synchronous multicentric
osteosarcomas. World J Surg Oncol. 10:2402012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dahlin DC and Coventry MB: Osteogenic
sarcoma. A study of six hundred cases. J Bone Joint Surg Am.
49:101–110. 1967.PubMed/NCBI
|
|
6
|
Fu HH, Zhuang QW, He J, Wang LZ and He Y:
Giant cell-rich osteosarcoma or giant cell reparative granuloma of
the mandible? J Craniofac Surg. 22:1136–1139. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Granowski-LeCornu M, Chuang SK, Kaban LB
and August M: Osteosarcoma of the jaws: Factors influencing
prognosis. J Oral Maxillofac Surg. 69:2368–2375. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brannon RB, Fowler CB, Carpenter WM and
Corio RL: Cementoblastoma: An innocuous neoplasm? A
clinicopathologic study of 44 cases and review of the literature
with special emphasis on recurrence. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 93:311–320. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ferrari D, Codecà C, Battisti N, Broggio
F, Crepaldi F, Violati M, Bertuzzi C, Dottorini L, Caldiera S,
Luciani A, et al: Multimodality treatment of osteosarcoma of the
jaw: A single institution experience. Med Oncol. 31:1712014.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kämmerer PW, Shabazfar N, Vorkhshori
Makoie N, Moergel M and Al-Nawas B: Clinical, therapeutic and
prognostic features of osteosarcoma of the jaws - experience of 36
cases. J Craniomaxillofac Surg. 40:541–548. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mendenhall WM, Fernandes R, Werning JW,
Vaysberg M, Malyapa RS and Mendenhall NP: Head and neck
osteosarcoma. Am J Otolaryngol. 32:597–600. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Roca AN, Smith JL Jr and Jing BS:
Osteosarcoma and parosteal osteogenic sarcoma of the maxilla and
mandible: Study of 20 cases. Am J Clin Pathol. 54:625–636. 1970.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cavalcanti MG, Ruprecht A and Yang J:
Radiological findings in an unusual osteosarcoma in the maxilla.
Dentomaxillofac Radiol. 29:180–184. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gardner DG and Mills DM: The widened
periodontal ligament of osteosarcoma of the jaws. Oral Surg Oral
Med Oral Pathol. 41:652–656. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang S, Shi H and Yu Q: Osteosarcoma of
the jaws: Demographic and CT imaging features. Dentomaxillofac
Radiol. 41:37–42. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Raymond AK, Ayala AG and Knuutila S:
Conventional osteosarcoma. In: World Health Organization
Classification of Tumours. Pathology and Genetics of Tumours of
Soft Tissue and Bone. Fletcher CDM, Unni KK and Mertens F: IARC
Press. (Lyon). 264–270. 2002.
|
|
17
|
Klein MJ and Siegal GP: Osteosarcoma:
Anatomic and histologic variants. Am J Clin Pathol. 125:555–581.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jaffe HL: Intracortical osteogenic
sarcoma. Bull Hosp Joint Dis. 21:189–197. 1960.PubMed/NCBI
|
|
19
|
Nissanka EH, Amaratunge EA and Tilakaratne
WM: Clinicopathological analysis of osteosarcoma of jaw bones. Oral
Dis. 13:82–87. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Patel SG, Meyers P, Huvos AG, Wolden S,
Singh B, Shaha AR, Boyle JO, Pfister D, Shah JP and Kraus DH:
Improved outcomes in patients with osteogenic sarcoma of the head
and neck. Cancer. 95:1495–1503. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Garrington GE, Scofield HH, Cornyn J and
Hooker SP: Osteosarcoma of the jaws. Analysis of 56 cases. Cancer.
20:377–391. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Anil S, Krishnan AP and Rajendran R:
Osteosarcoma of the mandible masquerading as a dental abscess:
Report of a case. Case Rep Dent. 2012:6350622012.PubMed/NCBI
|
|
23
|
Bruland OS, Høifødt H, Saeter G, Smeland S
and Fodstad O: Hematogenous micrometastases in osteosarcoma
patients. Clin Cancer Res. 11:4666–4673. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nagler RM, Malkin L, Ben-Arieh Y and
Laufer D: Sarcoma of the maxillofacial region: Follow-up of 25
cases. Anticancer Res. 20:3735–3741. 2000.PubMed/NCBI
|
|
25
|
Yamaguchi S, Nagasawa H, Suzuki T, Fujii
E, Iwaki H, Takagi M and Amagasa T: Sarcomas of the oral and
maxillofacial region: A review of 32 cases in 25 years. Clin Oral
Investig. 8:52–55. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jundt G and Prein J: Bone tumors and
tumor-like lesions of the jaw. Findings from the Basel DOSAK
reference registry. Mund Kiefer Gesichtschir. 4(Suppl 1):
S196–S207. 2000.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mardinger O, Givol N, Talmi YP and Taicher
S: Osteosarcoma of the jaw. The chaim sheba medical center
experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
91:445–451. 2001. View Article : Google Scholar : PubMed/NCBI
|