Introduction
Nuchal-type fibroma is a rare, benign fibrous
proliferation of unknown pathogenesis involving the dermis and
subcutaneous tissues. The mass is characterized by hypocellular
bundles of collagen with entrapped adipocytes and increased numbers
of small nerves. Nuchal-type fibroma is generally located
predominantly in the interscapular and paraspinous regions
(1). In the majority of cases, the
lesion is solitary; only a small number of cases involving multiple
lesions have been reported (2–4).
Extranuchal sites include the extremities, lumbosacral area,
buttocks and face (4–11). The tumor typically presents between
the third and fifth decades of life, but lesions have additionally
been reported in patients aged 3–74 years. Nuchal-type fibroma has
been observed to be strongly associated with diabetes mellitus and
Gardner's syndrome (12). There is a
ratio of 4:1 male to female predominance, although this is not
observed in Gardner's syndrome-associated patients (4).
Clinically, nuchal-type fibroma characteristically
presents as an asymptomatic, firm, poorly circumscribed,
subcutaneous mass, which requires wide surgical excision (1–4). However,
the unencapsulated nature of this tumor makes complete resection
difficult, which may contribute to its propensity for local
recurrence. Alternatively, reoccurrence may be due to the
persistent presence of factors that triggered the initial
development of the lesion, for example, repetitive trauma (3,7).
Nuchal-type fibroma is frequently misdiagnosed and under-reported
due to a close histopathological similarity to other benign fibrous
tumors, including dermatofibrosarcoma protuberans, giant cell
fibroblastoma, mammary and extramammary myofibroblastoma, spindle
and pleomorphic cell lipoma, and elastofibroma (13). Due to the rarity of nuchal-type
fibroma, at present the mortality rate remains unknown.
To the best of our knowledge, <80 cases of
nuchal-type fibroma have been recorded in the literature, including
20 reports of sporadic cases and one clinicopathological study of
52 cases (4). Only 3 studies
describing magnetic resonance imaging (MRI) findings of nuchal-type
fibroma have been published (6–8). The
present study presents unique MRI findings of a nuchal-type fibroma
arising in the right shoulder of a 48-year-old man.
Case report
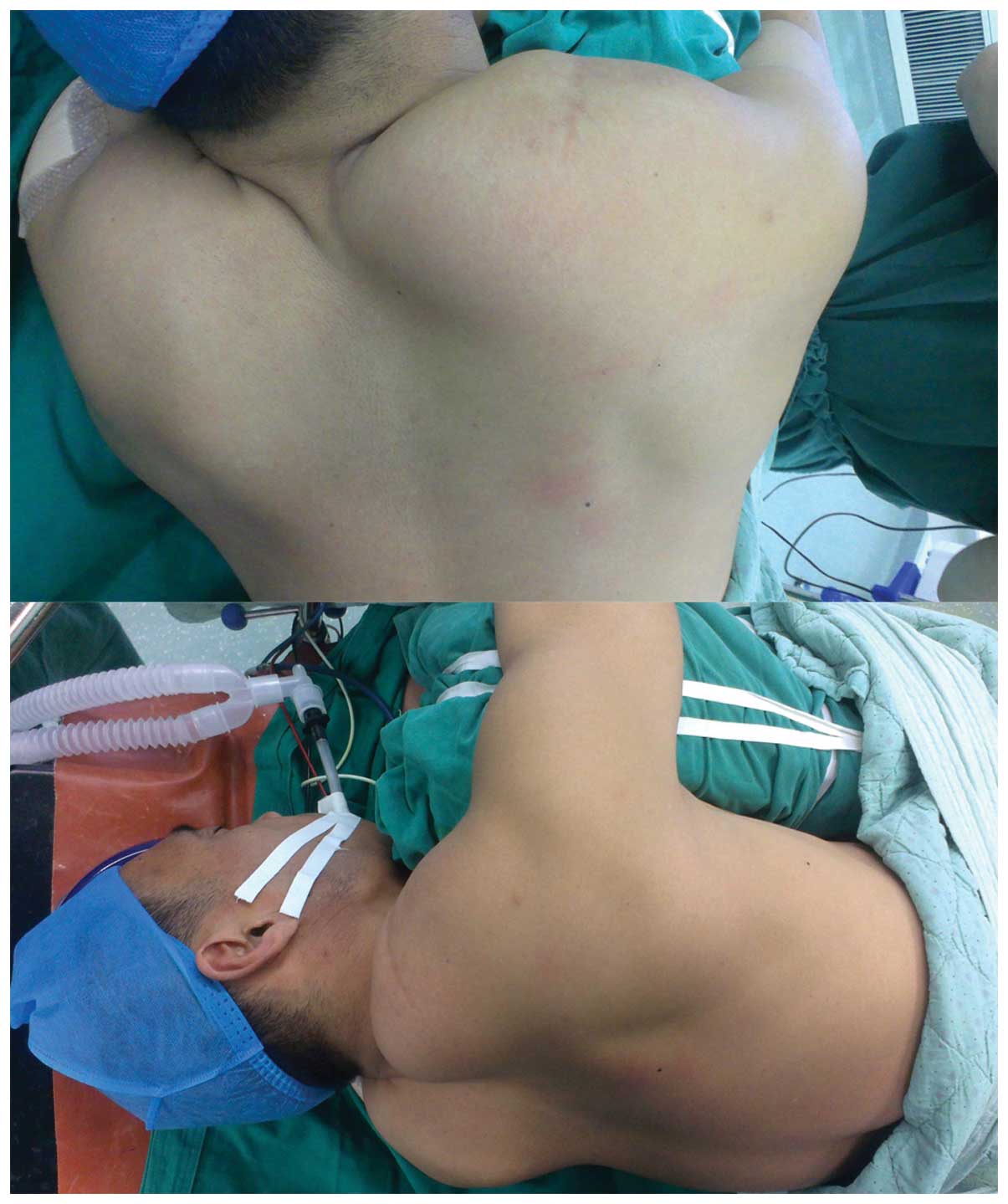
A 48-year-old man presented at The First Hospital of
Jilin University (Changchun, China) with a palpable mass in his
right shoulder in February 2014, which had been present for ~30
years. Clinical examination revealed a 20×10×5 cm solid lump in his
right shoulder. Overlying skin was observed to possess a normal
color and texture (Fig. 1). The
patient had no significant medical history and no history of trauma
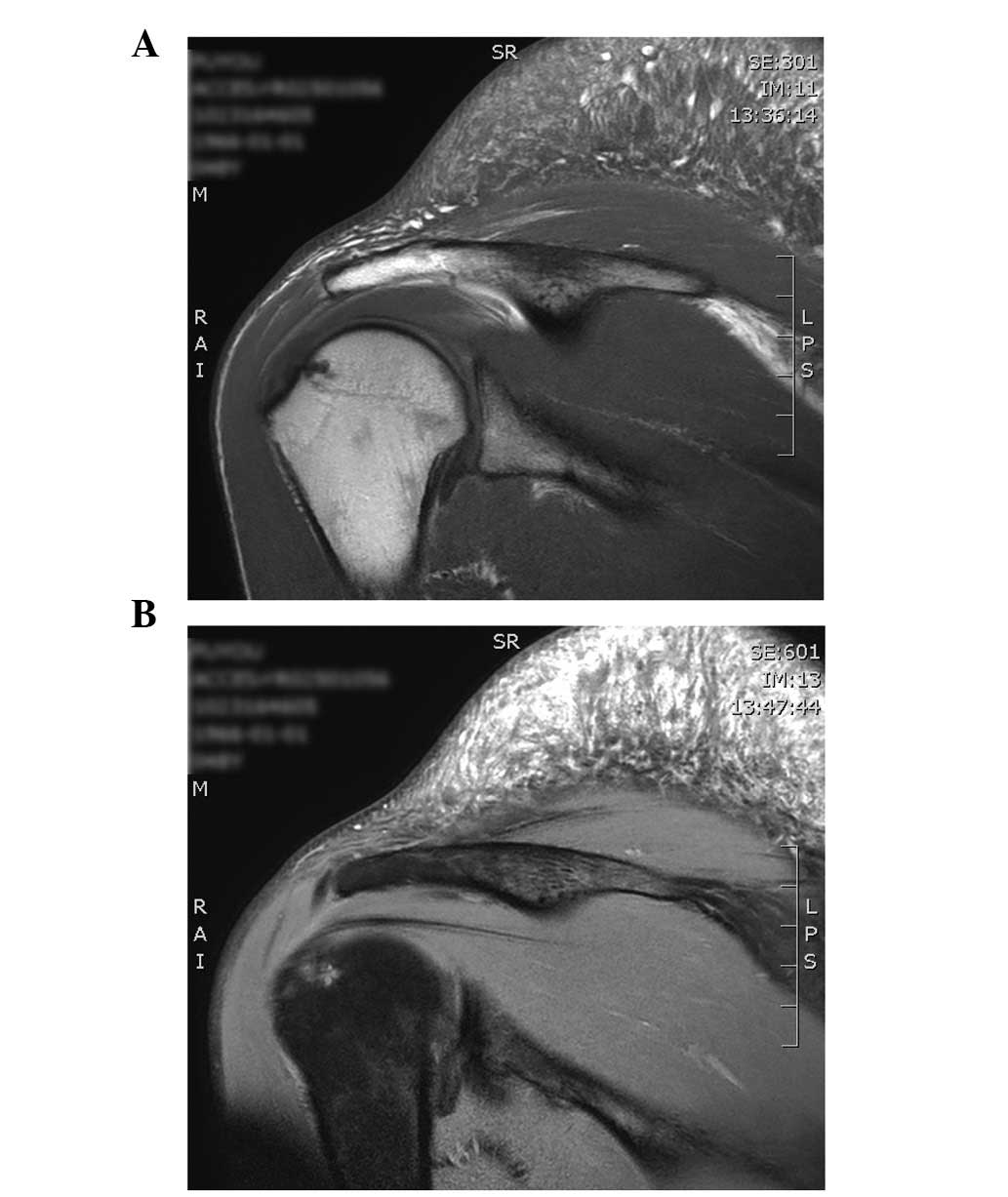
in the affected area. MRI (Ingenia 3.0T; Philips Medical Systems,
Inc., Bothell, WA, USA) revealed a mass with mixed signal intensity
T1- and T2-weighted images; however, the high signal intensity was
observed to be variable and non-unified. The high signal
demonstrated a strip-like pattern. On T2-weighted images, the area
of the high signal was markedly larger than that on T1-weighted
images (Fig. 2). Marginal excision of
the tumor was performed. A longitudinal incision was made to reveal
the mass. The lesion was not well demarcated and did not display a
definite capsule. The tumor was resected completely with a large
surrounding margin of normal tissue. Intraoperative fast frozen
pathology resulted in the diagnosis of fibroma, and the incision
was sutured without extensive excision. Light microscopic
examination (DP20; Olympus Corporation, Tokyo, Japan) of the
pathological specimen revealed following staining with hematoxylin
and eosin revealed that the mass was composed of typical collagen
fibers. Mucoid tissue degeneration was observed. The
clinicopathological features of the resected tissue were consistent
with a diagnosis of nuchal-type fibroma (Fig. 3). At the time of writing, the present
patient remained free of recurrent disease at the 8-month follow-up
appointment. Further observation of the patient will be performed
in the outpatient department.
Discussion
Nuchal-type fibroma typically presents as an
asymptomatic, relatively slow-growing, superficial mass (1–2,11). The mean tumor diameter is 3.5 cm, but
tumors have been observed to reach 8 cm in diameter (4). To the best of our knowledge, the largest
nuchal-type fibroma recorded in the literature was 16.5×15.0×6.5 cm
(10). The present study reports a
case of a nuchal-type fibroma with a size of ~20×10×5 cm. The mass
was large, visible under the skin of the patient's right shoulder
and easily palpable.
MRI is the preferred method to visualize nuchal-type
fibroma and its components and borders. Previously published MRI of
nuchal-type fibromas demonstrated masses with a low or mild signal
intensity (6–8). The present MRI revealed a mass that
displayed mixed signal intensity on T1- and T2-weighted images,
which was a prominent difference compared with previously reported
findings. The present MRI findings may assist in the differential
diagnosis of nuchal-type fibroma of the shoulder, particularly for
those with high signal intensity, which potentially indicates
mucoid degeneration of the nuchal-type fibroma (14,15). To
the best of our knowledge, this is the first report of mucoid
degeneration in nuchal-type fibroma. Since nuchal-type fibromas and
Gardner-associated fibromas resemble one another, it has been
suggested that a subset of nuchal-type fibromas that occur in
multiple sites, unusual locations or in children may be
Gardner-associated fibroma, in which the fibromatosis may present a
sentinel event for identification, which requires further genetic
analysis (16).
The etiology of nuchal-type fibroma remains to be
elucidated, but its microscopic features have been described and
confirmed by several studies (1–4,11–13,17,18).
Microscopically, the majority of nuchal-type fibromas are composed
of haphazardly arranged thick collagen fibers. Fibroblasts are
sparsely scattered between the collagen fibers (13,18,19). In
addition, entrapped islands of adipose tissue and skeletal muscle
are typically observed (1,3,13). In
certain cases, the lesions may contain enlarged peripheral nerves
with perineural fibrosis (1,13). Microscopic examination of the
pathological specimen from the present patient revealed typical
nuchal-type fibroma collagen fibers and mucoid tissue degeneration.
Additional research is required to confirm the factors involved in
the pathogenesis of nuchal-type fibroma.
Gross total resection within healthy tissue is the
preferred treatment for nuchal-type fibroma (3). Michal et al (4) reported that nuchal-type fibroma has a
tendency to recur following excision. From 25 reviewed cases of
nuchal-type fibroma, 3 patients presented with a single recurrence,
2 patients with lesions that recurred twice and 1 patient with a
lesion that recurred 3 times (4). In
the present case, complete surgical removal was performed with a
margin of surrounding normal tissue. A longitudinal incision was
made to reveal the entire mass. As the tumor was not well
demarcated, localization and definition of the tumor margin was
very important. Intraoperative fast frozen pathology resulted in
the diagnosis of fibroma, and the operation was concluded without
extensive excision. Retrospectively, the procedure may appear
inappropriate for the treatment of nuchal-type fibroma, since
incomplete resection may be associated with an increased recurrence
rate. The final pathological diagnosis indicated nuchal-type
fibroma, emphasizing that accurate intraoperative diagnosis is
essential in such cases. At the time of writing, the present
patient remained free of recurrent disease at the 8-month follow-up
appointment.
In conclusion, the present nuchal-type fibroma
demonstrated unique MRI findings and microscopic features that
differed from previously reported cases. Even though nuchal-type
fibroma is generally asymptomatic, it should be considered as a
potential diagnosis for a subcutaneous mass with mixed signal
intensity on T1- and T2-weighted images, particulary when the high
signals appear in a strip-like pattern, with additional findings of
typical collagen fibers and mucoid tissue degeneration observed by
microscopy. The present findings provide useful information that
may improve the clinical management of this uncommon lesion.
References
|
1
|
Enzinger FM and Weiss SW: Benign tumors
and tumorlike lesions of fibrous tissue. Soft Tissue Tumors (2nd).
Mosby. (Maryland Heights, MO). 102–135. 1988.
|
|
2
|
Lee SE, Kim YC and Kim SC: Nuchal fibroma
presenting as two posterior neck masses. J Dermatol. 34:262–263.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
do Kim H, Kim TH, Sung NH, Shin H, Lee AY
and Lee SH: Multiple nuchal-type fibromas on the scalp: A case
report. Ann Dermatol. 27:194–196. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Michal M, Fetsch JF, Hes O and Miettinen
M: Nuchal-type fibroma: A clinicopathologic study of 52 cases.
Cancer. 85:156–163. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Döngel I, Yazkan R, Duman L, Oztürk O and
Kapucuoğlu FN: Huge inflammatory myofibroblastic tumor of pleura
with concomitant nuchal fibroma. Ann Thorac Surg. 96:1461–1464.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee GK, Suh KJ, Lee SM and Lee SJ:
Nuchal-type fibroma of the buttock: Magnetic resonance imaging
findings. Jpn J Radiol. 28:538–541. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sraj SA, Lahoud LE, Musharafieh R and Taha
A: Nuchal-type fibroma of the ankle: A case report. J Foot Ankle
Surg. 47:332–336. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ewald C, Kuhn SA, Brodhun M and Kalff R:
Nuchal extra-abdominal aggressive fibromatosis of desmoid type in a
77-year-old female. Neurol India. 55:419–420. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Michal M: Non-nuchal-type fibroma
associated with Gardner's syndrome. A hitherto-unreported
mesenchymal tumor different from fibromatosis and nuchal-type
fibroma. Pathol Res Pract. 196:857–860. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hameed M, Benevenia J, Blacksin M and
Aisner SC: Nuchal fibroma of the shoulder involving skeletal
muscle: A radiographic and clinicopathological study. A case
report. J Bone Joint Surg Am. 80:1684–1686. 1998.PubMed/NCBI
|
|
11
|
Balachandran K, Allen PW and MacCormac LB:
Nuchal fibroma. A clinicopathological study of nine cases. Am J
Surg Pathol. 19:313–317. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Diwan AH, Graves ED, King JA and
Horenstein MG: Nuchal-type fibroma in two related patients with
Gardner's syndrome. Am J Surg Pathol. 24:1563–1567. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Díaz-Flores L, Gutiérrez R, García MP,
Sáez FJ, Díaz-Flores L Jr, Valladares F and Madrid JF: CD34+
stromal cells/fibroblasts/fibrocytes/telocytes as a tissue reserve
and a principal source of mesenchymal cells. Location, morphology,
function and role in pathology. Histol Histopathol. 29:831–870.
2014.PubMed/NCBI
|
|
14
|
Chudasama CH, Chudasama VC and Prabhakar
MM: Arthroscopic management of mucoid degeneration of anterior
cruciate ligament. Indian J Orthop. 46:561–565. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cho SD, Youm YS, Lee CC, Seo DK and Kim
TW: Mucoid degeneration of both ACL and PCL. Clin Orthop Surg.
4:167–170. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wehrli BM, Weiss SW, Yandow S and Coffin
CM: Gardner-associated fibromas (GAF) in young patients: A distinct
fibrous lesion that identifies unsuspected Gardner syndrome and
risk for fibromatosis. Am J Surg Pathol. 25:645–651. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Alsaleh N and Amanguno H: Nuchal Fibroma:
A rare entity of neck masses. Gulf J Oncolog. 1:10–12.
2015.PubMed/NCBI
|
|
18
|
Linos K, Sedivcová M, Cerna K, Sima R,
Kazakov DV, Nazeer T, Glazyrin A, Valerian BT and Carlson JA: Extra
nuchal-type fibroma associated with elastosis, traumatic neuroma, a
rare APC gene missense mutation, and a very rare MUTYH gene
polymorphism: A case report and review of the literature. J Cutan
Pathol. 38:911–918. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Diwan AH and Horenstein MG:
Dermatofibrosarcoma protuberans association with nuchal-type
fibroma. J Cutan Pathol. 31:62–66. 2004. View Article : Google Scholar : PubMed/NCBI
|