Introduction
Borrmann type IV gastric carcinoma is a diffused
type of gastric cancer (1) that
presents with thickening and stiffening of the gastric wall as a
result of invasive infiltration of at least a third of the
circumference of the stomach (2). In
1858, Brinton first coined the term linitis plastica, which
is also referred to as cirrous carcinoma in English literature, to
describe infiltrative gastric carcinoma invading throughout the
stomach (3). Approximately 10 to 15%
of all gastric adenocarcinomas are considered to be Borrmann's type
IV (4). This type is associated with
poor prognosis as the disease is often diagnosed at an advanced
stage. This may be due to difficulties in detecting the presence of
gastric carcinoma under endoscopic inspection, as there is usually
no ulceration or elevation appearing on the mucosal surface at the
early stage of this malignancy (5).
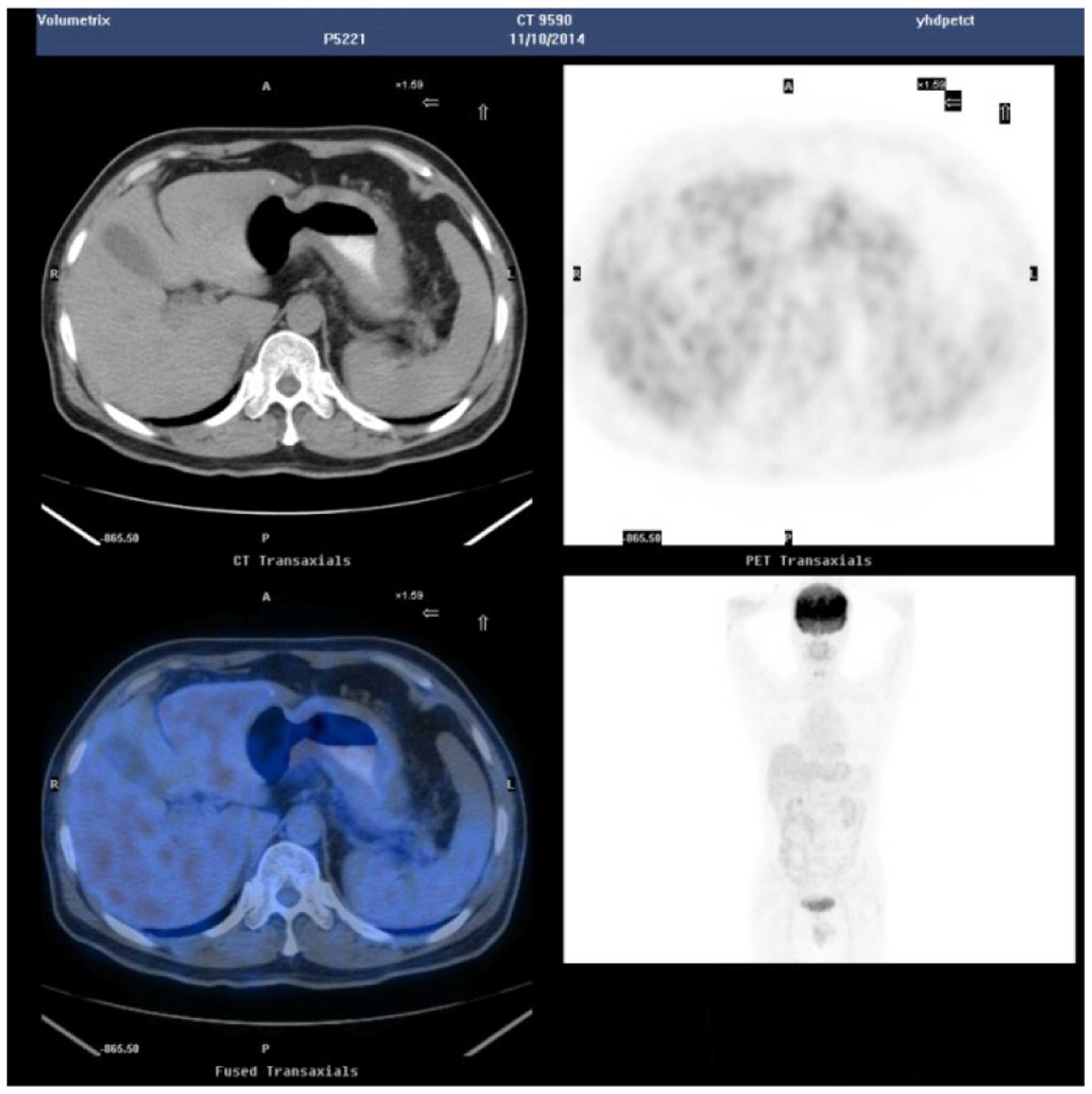
In addition, F-18 fluorodeoxyglucose positron emission tomography
(FDG-PET) is of limited use in this lesion as primary gastric
tumors are generally not susceptible to this radiopharmaceutical
(6). This study reports the case of a
patient suspected of having Borrmann type IV gastric carcinoma but
for whom repeated endoscopic biopsies and positron emission
tomography-computed tomography (PET-CT) examinations failed to
confirm the diagnosis. Written informed consent was obtained from
the patient.
Case report
Patient presentation and history
A 54-year-old male patient presented to Yantai
Yuhuangding Hospital affiliated to Qingdao University (Yantai,
China) on October 31, 2014, following 3 months of recurrent
abdominal distention after eating. Gastric lesions were suspected.
The patient had no notable medical or family history. He had been
previously admitted to a local hospital due to the complaint of
stomach discomfort, and had received two gastroscopy examinations.
Gastroscopy had revealed erosive gastritis, but there was no
apparent ulceration or other lesions indicating tumors. The biopsy
results had revealed chronic gastritis with erosion of the corpora
ventriculi. An upper gastrointestinal barium meal examination was
then performed, and the examination results suggested the
possibility of infiltrating gastric cancer. An abdominal
contrast-enhanced CT scan was therefore performed, which revealed a
thickened stomach wall of the gastric body. Gastric cancer was
considered and the patient was referred to our hospital for further
diagnosis and treatment.
Examinations and diagnosis
Physical examination upon admission revealed no
anemia (via conjunctival pallor examination), jaundice or pulmonary
abnormalities. The abdomen of the patient was bulging on palpation,
with tenderness of the subxiphoid area. There was no pretibial
edema, and no palpable abdominal mass or superficial lymph nodes.
Blood tests revealed no abnormality of biomarkers including
α-fetoprotein, carcinoembryonic antigen, or tumor markers CA72-4
and CA19-9. A third gastroscope biopsy was later conducted, which
only revealed chronic inflammation of gastric body mucosa (Figs. 1 and 2).
The patient was suspected by the multidisciplinary discussion team
of having Borrmann type IV gastric cancer. Another deep biopsy was
performed with endoscopic ultrasound guidance, which revealed
mucosal hyperemia of the fundus of the stomach and roughened mucosa
in the corpus (Fig. 3). There was
also marked thickening of the gastric wall (~8 mm; Fig. 4), low echo contrast, and loss of
peristaltic movement. Endoscopic ultrasonography of the thickened
stomach wall indicated features of typical changes of malignant
lesions. Ten tissue cores were sampled by biopsy forceps in the
thickened stomach wall. However, no tumor cells were identified by
pathological analysis, so the diagnosis of chronic inflammation of
the gastric mucosa was retained (Fig.
5). In order to exclude the possibility of gastric carcinoma, a
PET-CT scan was requested. Examination revealed slight thickening
of the lesser curvature wall in the proximal gastric angle region,
and splenomegaly with normal 18F-fluorodeoxyglucose (18F-FDG)
uptake (Fig. 6). PET-CT failed to
identify malignant transformations. On November 12, the patient
underwent a second upper alimentary tract barium meal examination,
with the result suggesting possible infiltrative gastric carcinoma.
Still, no definitive diagnosis was given. The patient was
discharged at this point.
Two weeks later, he was admitted to another hospital
due to frequent urination. Cytoscopy examination confirmed apparent
thickening of a large area of the right bladder wall. The biopsy
was sampled and immunohistochemical examination was performed.
Consultation with the pathology department of Yuhuangding Hospital
concluded that malignant cells were present in the interstitial
tissue of the bladder (Fig. 7).
Immunohistochemical examination revealed positive staining for
Syn(+), CK(+) and negative staining for LCA(−), SPA(−), CDX2(−) and
CK20(−), which indicated a gastrointestinal origin of the
pathology; specifically poorly differentiated gastric
adenocarcinoma with neuroendocrine metastasis to the bladder.
Therefore, in combination with the medical history, physical
examination and auxiliary examination during hospitalization, the
patient was diagnosed as having Borrmann type IV gastric cancer,
and the histological type was confirmed to be gastric poorly
differentiated adenocarcinoma with neuroendocrine metastasis.
Discussion
The classification of advanced gastric cancer (ADC)
into four distinct types was introduced by Borrmann in 1926; these
remain the standard criteria in cancer diagnosis (7,8).
Borrmann's type IV gastric cancer is characterized by a unique
morphology both macroscopically and microscopically (9). Gastric linitis plastica is a
diffuse infiltrative type of cancer in which the malignant cells
invade a large area of the stomach, causing thickening and
stiffening of the stomach wall (10).
The majority of patients presenting with symptoms
are diagnosed at an advanced stage due to the limited sensory
system of the stomach. Histopathological findings are essential to
the diagnosis and therapeutic decision-making in Borrmann type IV
gastric cancer. Histopathological diagnosis is the diagnostic gold
standard of Borrmann type IV gastric cancer required by medical
ethics and practice guidelines. However, tumor cells individually
invade the submucosa without prominent ulcers or masses on the
mucosal surface in the early stage. Early diagnosis of Borrmann's
type IV cancer is difficult (9).
Endoscopic biopsy demonstrated 90–98% sensitivity in the detection
of gastric cancer; however, in the case of Borrmann type IV AGC,
not only detection of the tumor but also diagnosis of the specific
type of tumor is documented as being difficult with gastroscopy. In
addition, the success rate in correctly diagnosing the malignancy
via endoscopic biopsy is also significantly lower in Borrmann type
IV AGC compared with other Borrmann types. The unsatisfactory
performances of gastroscopy and combined biopsy reflect the complex
submucosa origination and unique morphological features of Borrmann
type IV cancer. Infiltration predominantly occurs in the submicosal
or muscular area, and is often associated with no apparent
ulceration or elevation on the mucosal surface, which creates
difficulty in endoscopic observation. Moreover, tumor cells are
often widely dispersed within a dense fibrous stroma as a result of
desmoplastic reaction that spares the mucosal layer, which may also
influence pathological analysis of a small biopsy that may only
contain the normal mucosal layer (11).
PET has been used to diagnose and monitor cancer
lesions for many years. FDG is the most commonly used
radiopharmaceutical, which uses the glucose metabolic path for
diagnosing cancer. The increased metabolism of FDG is a
characteristic of numerous cancer types. There are certain other
radiotracers that have been proven useful in addition to 18F-FDG
(12). FDG uptake is closely related
to tissue property, rather than being specific to one type of
malignant neoplasm. Therefore, attempts to use PET-CT with FDG in
gastric cancer diagnosis may be unsatisfactory (12). Kawamura et al (13) reported that the expression level of
GLUT1 protein in stomach carcinomas was 30% (128/617), and no
expression was observed in 50 samples of tubular adenomas of the
stomach; its expression in signet ring cell carcinoma and mucinous
adenocarcinoma was relatively low, at 2% and 6%, respectively.
Among the other histological types, papillary adenocarcinoma (44%)
demonstrated slightly higher GLUT1 expression levels than the
tubular (32%) or poorly differentiated adenocarcinoma type (28%)
(14). In addition, tests for
Borrmann type IV gastric cancer often present a false negative
result due to the abounding mucin content. It should also be
distinguished from mucinous adenocarcinoma, signet ring cell
carcinoma and poorly differentiated adenocarcinoma, which are also
low in 18F-FDG uptake (15).
Therefore, it would be inappropriate to confirm a diagnosis simply
based on high FDG uptake, as this could also occur in gastritis or
stomach ulcers (15).
In summary, accurate preoperative diagnosis of
Borrmann type IV gastric cancer is extremely difficult, usually due
to its distinctive infiltration pattern along the submucosal layer.
Multiple gastroscopic biopsy and deep biopsy under radiological
guidance that reaches the proper area of the lesion, are essential
for the diagnosis of Borrmann type IV gastric cancer. The utility
of 18F-FDG in PET-CT is limited in the diagnosis of gastric cancer;
further evaluation of 18F-FDG uptake in gastric cancer is
required.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant no., 81071758), Shangdong
Science and Technology Development Project (grant no.,
2015GSF118142), the Natural Science Foundation of Shandong Province
Joint Programme (grant no., ZR2015HL069) and Yantai Yuhuangding
Hospital Initiative Foundation for Young Scientist (grant no.,
201402).
References
|
1
|
Lauren P: The two histological main types
of gastric carcinoma: diffuse and so-called intestinal-type
carcinoma. An attempt at a histo-clinical classification. Acta
Pathol Microbiol Scand. 64:31–49. 1965.PubMed/NCBI
|
|
2
|
Pedrazzani C, Marrelli D, Pacelli F, Di
Cosmo M, Mura G, Bettarini F, Rosa F, de Manzoni G and Roviello F:
Gastric linitis plastica: Which role for surgical resection?
Gastric Cancer. 15:56–60. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moreaux J, Barrat F and Msika S: Linitis
plastica of stomach. Study of 102 cases surgically treated. Results
of the surgical treatment. Chirurgie. 112:485–492. 1986.(In
French). PubMed/NCBI
|
|
4
|
Accetta AC, Manso JE, Mello EL, Paiva RK,
Castro Ldos S and Accetta P: Type IV Borrmann gastric
adenocarcinoma: analysis of curative resection results. Rev Col
Bras Cir. 38:237–244. 2011.(In English and Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yook JH, Oh ST and Kim BS:
Clinicopathological analysis of Borrmann type IV gastric cancer.
Cancer Res Treat. 37:87–91. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sampath S, Harisankar CN, Bhattacharya A,
Gupta R and Mittal BR: F-18 Fluorodeoxyglucose positron emission
tomography/computed tomography in the staging of linitis plastica
caused by primary gastric adenocarcinoma. World J Nucl Med.
12:67–69. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Borrmann R: Geschwulste des margens.
Handbuch Spez Pathol Anat und Histo. Henke F and Lubarsch O: (1st).
Springer-Verlag. (Berlin, Germany). 864–871. 1926.(In German).
|
|
8
|
Borchard F: Classification of gastric
carcinoma. Hepatogastroenterology. 37:223–232. 1990.PubMed/NCBI
|
|
9
|
Yokota T, Teshima S, Saito T, Kikuchi S,
Kunii Y and Yamauchi H: Borrmann's type IV gastric cancer:
clinicopathologic analysis. Can J Surg. 42:371–376. 1999.PubMed/NCBI
|
|
10
|
Jafferbhoy S, Shiwani H and Rustum Q:
Managing gastric linitis plastica: keep the scalpel sheathed.
Sultan Qaboos Univ Med J. 13:451–453. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim JI, Kim YH, Lee KH, Kim SY, Lee YJ,
Park YS, Kim N, Lee DH, Kim HH, do Park J and Lee HS: Type-specific
diagnosis and evaluation of longitudinal tumor extent of borrmann
type IV gastric cancer: CT versus gastroscopy. Korean J Radiol.
14:597–606. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Staniuk T, Zegarski W, Małkowski B,
Jankowski M, Klag M and Pietrzak T: Evaluation of FLT-PET/CT
usefulness in diagnosis and qualification for surgical treatment of
gastric cancer. Contemp Oncol (Pozn). 17:165–170. 2013.PubMed/NCBI
|
|
13
|
Kawamura T, Kusakabe T, Sugino T, Watanabe
K, Fukuda T, Nashimoto A, Honma K and Suzuki T: Expression of
glucose transporter-1 in human gastric carcinoma: Association with
tumor aggressiveness, metastasis, and patient survival. Cancer.
92:634–641. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Małkowski B, Staniuk T, Srutek E, Gorycki
T, Zegarski W and Studniarek M: (18F)-FLT PET/CT in patients with
gastric carcinoma. Gastroenterol Res Pract. 2013:6964232013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Song W, Chen CY, Xu JB, Ye JN, Wang L,
Chen CQ, Zhang XH, Cai SR, Zhan WH and He YL: Pathological
diagnosis is maybe non-essential for special gastric cancer: case
reports and review. World J Gastroenterol. 19:3904–3910. 2013.
View Article : Google Scholar : PubMed/NCBI
|