Introduction
As life expectancy continues to increase, the number
of elderly patients requiring surgery for the treatment of cancer
also increases (1,2). Cancer management of nonagenarian or
centenarian patients is challenging. Although maintenance of good
health is necessary to achieve longevity, organ function will
deteriorate over time, making the elderly susceptible to stress,
including trauma or surgery, which compromises homeostasis and
results in organ dysfunction or aggravates existing dysfunction
(1,2).
Elderly patients have increased morbidity and mortality risks;
thus, balancing higher toxicity risks with potential improvement of
quality of life due to anticancer therapies presents a significant
challenge when caring for particularly elderly patient (3).
In 2014, the population of Japan included >60,000
citizens aged ≥100 years (4). Japan
has an increasing elderly population, with Okinawa in particular
having one of the highest proportion of elderly individuals. In the
Okinawan culture, a preference for noninvasive care for elderly
patients with cancer may present challenging circumstances for
clinicians when the cancer may be curable (3). Palliative care may not always be a
sufficient treatment choice, particularly if patients suffer from
impaired quality of life and pain from symptoms of untreated cancer
progression (3). Early stage tongue
cancer is particularly easy to access for surgical resection. By
contrast, if left untreated, later stages of this disease is
associated with pain, dysphagia and throat obstruction. Therefore,
the optimal treatment for early stage oral cavity squamous cell
carcinoma (SCC) is surgery (5).
The current case describes a 99-year-old patient
with early stage tongue cancer, which was successfully resected
under general anesthesia. The patient lived disease-free for 5
years, surviving to 104 years old. The study was conducted in
compliance with the Declaration of Helsinki and was approved by the
Ethics Committee of the University of The Ryukyus (Okinawa, Japan).
Written informed consent was obtained from the next of kin of the
patient for publication of the present case report and any
accompanying images.
Case report
A 99-year-old female, who was independent in her
daily activities, presented to our hospital with a 2-month history
of pain at the right edge of the tongue. The patient had no history
of trauma to the tongue. Oral examination identified an indurated,
ulcerated mass, measuring 3×1.5 cm in diameter and was located in
the right tongue margin (Fig. 1).
There was no restriction of tongue movement and no palpable
cervical lymph nodes. A clinical diagnosis of early stage tongue
cancer (T2N0Mx) was made according to the Union for International
Cancer Control TNM classification system (6). A computed tomography (CT) scan was
performed following administration of intravenous contrast material
and identified an enhancing tumor measuring 1.3×0.7 cm in the right
margin of the tongue.
On examination, the patient was 1.39 m tall and
weighed 37 kg with a body mass index of 19.15 kg/m2. By
surgical considerations, the patient was New York Heart Association
class I and American Society of Anesthesiologist Physical Status 2.
Following a number of tests, it was noted that the patient's blood
pressure, pulse rate, respiratory rate and SaO2 were
within the normal ranges (124/70 mmHg, 74 beats/min, 18 breaths/min
and 98% in room air, respectively). The patient had a history of
cerebral infarction 10 years prior to presentation, in addition to
hypertension, sinus bradycardia and kyphosis with a thoracic
compression fracture, but demonstrated no history of
hyperlipidemia, diabetes, cardiac arrhythmia or other evidence of
heart disease. There were no other significant findings from
physical examination. A surgical treatment strategy was discussed
with the patient and the family, and informed consent was obtained
from the next of kin.
Preoperative blood and urine tests reported normal
blood counts, electrolytes and blood coagulation results.
Bilirubin, urea and creatinine levels were unchanged following
diagnostic exams and surgery. The total protein of the patient was
6.9 g/dl. An X-ray of the chest was normal, and an
electrocardiogram reported the presence of sinus bradycardia. The
patient was evaluated by a cardiologist and an anesthesiologist
prior to selecting a treatment strategy. An echocardiogram revealed
moderate pulmonic and tricuspid regurgitation, which the
cardiologist assessed as age-appropriate, and a normal ejection
fraction of 78%. A CT scan of the brain identified no new cerebral
infarctions. The anesthesiologist determined that the patient was a
good candidate for general anesthesia, and suggested that kyphotic
surgical task curvature should be utilized to modify the supine
surgical position due to kyphosis (Fig.
2).
Surgical resection of the tongue tumor was
performed, and 10 mm tumor-free margins were obtained (Fig. 3). Following resection,
TERUDERMIS® (Terumo Corporation, Tokyo, Japan), a
collagen-based artificial dermis, was grafted onto the cleansed
wound surface. The surgical procedure lasted 60 min in the absence
of hypotension, bradycardia or decreased oxygen saturation
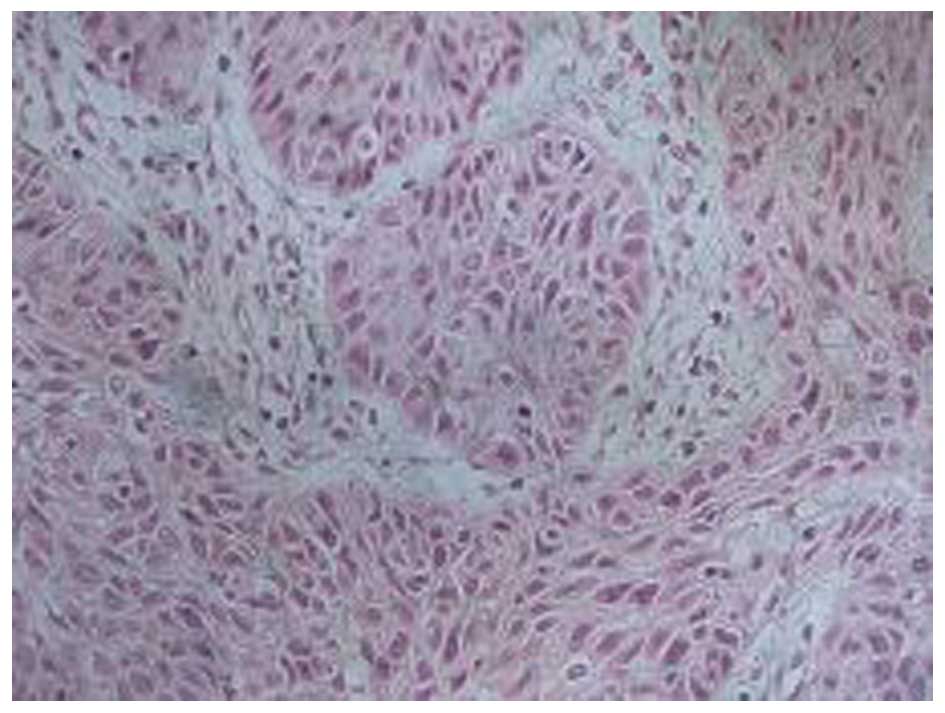
(2). Histopathology of the tongue
mass specimen revealed moderate proliferation of SCC cells.
Inflammation was noted beneath the epithelium (Fig. 4), but peripheral infiltration of the
tumor cells was not observed. Thus, the lesion was diagnosed as
SCC.
The postoperative course was complicated by slight
pain, but the patient did not experience any episodes of delirium.
Nonsteroidal anti-inflammatory drugs were administered for pain
relief, either as a suppository or internally. Intravenous
hydration was discontinued on the first postoperative day and oral
feeding was resumed 6 h post-surgery. The patient was hospitalized
for 14 days for routine monitoring due to old age. Subsequent to
being discharged, the patient lived for 5 years and 2 months more
without any evidence of disease recurrence (Fig. 5).
Discussion
Living to 100 years of age is no longer a rarity
(2), with >60,000 centenarians
living in Japan. Okinawa is a prefecture located in the
southernmost part of Japan and is well-known around the world for
the longevity of its populations. According to statistical reports
from the World Health Organization and the Japanese Ministry of
Health, Labour and Welfare, Okinawan individuals experience
extremely low mortality from stroke, coronary artery disease, and
hormone-dependent cancer of the ovary, prostate and breast
(7). It has also been reported that
Okinawan residents who follow a traditional lifestyle of physical
exercise, diet, cooking, stress coping, guidance of the ‘ikigai’
(meaning living satisfaction) and food culture, enjoy extended
longevity (7,8). Despite rapid changes in regional
politics and lifestyle, the people of Okinawa maintain cultural
respect of their ancestry and the elderly with close family ties
(9).
In general, advances in the medical field have
resulted in increases in life expectancy. Therefore, surgery with
general anesthesia has become an important issue for elderly
patients (2). Aging is associated
with various physiological changes that affect functional reserve
and result in a diminished ability to respond appropriately to
stresses such as surgery (2).
Perioperative mortality rates have decreased in elderly patients,
however, the long-term benefit to these individuals is unknown
(10). The National Cancer Center
Network (NCCN) has published a series of guidelines indicating
that, in general, age is not the primary consideration for surgical
risk (11). Although surgery under
general anesthesia in nonagenarians and centenarians is not without
risk, available studies regarding surgery in centenarians suggest
that there is no significantly increased risk of mortality
(12–15). Results of a previous study of
nonagenarians and centenarians support the hypothesis that cardiac
surgical procedures may appropriately be performed on a higher-risk
patient group independent of age (16). The same study also demonstrated that
the majority of nonagenarians and centenarians could be
preoperatively identified as having a relatively low mortality risk
(2,16). A recent study of 1,201 patients
undergoing major surgery for head and neck cancer identified that
surgical complication rates did not increase with age (17). By contrast, advanced tumor stage and
prolonged surgery time were associated with surgical complications
(17). Medical evaluation should
focus on risk factor identification, optimization of health status,
prediction of complications, and providing accurate information to
the surgeon, physician and anesthesiologist (2). Although the 99-year-old patient
described in the current case presented with evidence of mild
clinical diseases, the patient was able to perform normal
activities and the laboratory tests were within normal limits.
In 1990, Barzan et al (18) published a retrospective study of 438
elderly patients with head and neck cancer. The study stated that
although age did affect several features of patients with head and
neck cancer, it did not appear to be an independent prognostic
factor for survival and local control (18). Furthermore, the study outlined the
treatment policy for head and neck cancer during those years as
follows: All resectable lesions underwent radical surgery, followed
by radiotherapy if the resected tumor demonstrated unfavorable
histological prognostic features, including extra-nodal spread or
positive surgical resection margins (18). Radiotherapy alone, or combined with
chemotherapy, was administered to patients with loco-regional tumor
extension or poor status that precluded radical surgery (18).
Older patients with head and neck cancer require
more supportive care (19). The NCCN
guidelines also emphasize the application of supportive care to
minimize toxicity and promote cancer treatment effectiveness among
older patients (11). The
preanesthetic evaluation of the entire procedure and projected rate
of postoperative recovery allows for successful surgical treatment
(2). There were no episodes of
postoperative delirium. Prehospital and postoperative nutritional
status may also serve an important role in the surgical outcomes
for centenarians (2,20), and thus, in the present case, oral
feeding was resumed 6 h post-surgery. Furthermore, a coordinated
care approach between surgical and geriatric medical teams is
highly desirable to achieve positive outcomes (15,21).
In the current case, the patient and their family
agreed to the performance of surgical resection under general
anesthesia, which provided pain relief and allowed the patient to
maintain a good quality of life. The most notable fact of the
present case is perhaps that the patient was discharged without
complications and lived without recurrence for 5 more years. To the
best of our knowledge, this patient is one of the oldest
individuals to undergo a partial tongue cancer resection under
general anesthesia. Despite previous studies describing the
treatment of head and neck cancer in elderly patients (22–24), a
previous study describing the treatment of tongue cancer by surgery
under general anesthesia in a patient ≥99 years old could not
identified.
In conclusion, a treatment plan should ideally be
based on careful assessment of the wishes of the patient and their
family, medical risks, and benefits and economic costs of
alternative treatments (2), in
addition to consideration of the patient's culture. The present
case demonstrates that an elderly patient is able to undergo
successful surgical resection under general anesthesia. The
relative safety of surgical interventions and perioperative care of
elderly patients should encourage physicians to keep surgical
treatment options in mind despite their advanced age.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for an English language review of the
original manuscript.
References
|
1
|
Rosenthal RA and Kavic SM: Assessment and
management of the geriatric patient. Crit Care Med. 32(Suppl 4):
S92–S105. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Imbelloni LE, Lima U and Pedrosa FK:
Successful anesthesia and hip surgery in a 107-year-old patient. Am
J Case Rep. 15:308–311. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chien CR and Shih YC: Use of personalized
decision analysis in decision making for palliative vs. surgical
management of the oldest-old patients with localized skin cancer in
a culturally sensitive environment: A case study of a 96-year-old
male Taiwanese patient. J Pain Symptom Manage. 45:792–797. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Japan Statistics Bureau: Japan Population
Statistics. http://www.stat.go.jp/data/jinsui/pdf/201407.pdfAccessed.
July 22–2014(In Japanese).
|
|
5
|
Shah JP: Surgical approaches to the oral
cavity primary and neck. Int J Radiat Oncol Biol Phys. 69(Suppl 2):
S15–S18. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sobin LH, Gospodarowicz MK and Wittekind
C: Head and Neck tumours. TNM Classification of Malignant Tumours.
O'Sullivan B: (7th). Wiley-Blackwell. (Oxford). 22–62. 2009.
|
|
7
|
Suzuki M, Willcox B and Willcox C:
Successful aging: Secrets of okinawan longevity. Geriatr Gerontol
Int. 4(s1): S180–S181. 2004. View Article : Google Scholar
|
|
8
|
Sho H: History and characteristics of
Okinawan longevity food. Asia Pac J Clin Nutr. 10:159–164. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Iseki K: Screening and prevention of renal
disease: Large population study in Okinawa, Japan. Nephrology.
4:S86–S89. 1998. View Article : Google Scholar
|
|
10
|
Clayman GL, Eicher SA, Sicard MW, Razmpa E
and Goepfert H: Surgical outcomes in head and neck cancer patients
80 years of age and older. Head Neck. 20:216–223. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
National Comprehensive Cancer Network:
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines):
Older Adult Oncology. 2015.http://www.nccn.org/professionals/physician_gls/pdf/senior.pdfAccessed.
January 15–2015
|
|
12
|
Forster MC and Calthorpe D: Mortality
following surgery for proximal femoral fractures in centenarians.
Injury. 31:537–539. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Warner MA, Saletel RA, Schroeder DR,
Warner DO, Offord KP and Gray DT: Outcomes of anesthesia and
surgery in people 100 years of age and older. J Am Geriatr Soc.
46:988–993. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Katlic MR: Surgery in centenarians. JAMA.
253:3139–3141. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ozorio G and Chan DK: Surgery in the very
elderly. Intern Med J. 37:837–838. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bridges CR, Edwards FH, Peterson ED,
Coombs LP and Ferguson TB: Cardiac surgery in nonagenarians and
centenarians. J Am Coll Surg. 197:347–357. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Peters TT, van Dijk BA, Roodenburg JL, van
der Laan BF and Halmos GB: Relation between age, comorbidity and
complications in patients undergoing major surgery for head and
neck cancer. Ann Surg Oncol. 21:963–970. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Barzan L, Veronesi A, Caruso G, Serraino
D, Magri D, Zagonel V, Tirelli U, Comoretto R and Monfardini S:
Head and neck cancer and ageing: A retrospective study in 438
patients. J Laryngol Otol. 104:634–640. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
VanderWalde NA, Fleming M, Weiss J and
Chera BS: Treatment of older patients with head and neck cancer: A
review. Oncologist. 18:568–578. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Takeda S, Noji H, Hirose N, Arai Y,
Yamamura K, Shimizu K, Homma S, Ebihara Y and Takayama M:
Nutritional intake by the oldest elderly Japanese. Tokyo
Centenarian Study 6. Nippon Ronen Igakkai Zasshi. 35:548–558.
1998.(In Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Solomon DH: A statement of principles:
Toward improved care of older patients in surgical and medical
specialities. J Am Geriatr Soc. 48:699–701. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Siddiqui F and Gwede CK: Head and neck
cancer in the elderly population. Semin Radiat Oncol. 22:321–333.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Syrigos KN, Karachalios D, Karapanagiotou
EM, Nutting CM, Manolopoulos L and Harrington KJ: Head and neck
cancer in the elderly: An overview on the treatment modalities.
Cancer Treat Rev. 35:237–245. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sarris EG, Harrington KJ, Saif MW and
Syrigos KN: Multimodal treatment strategies for elderly patients
with head and neck cancer. Cancer Treat Rev. 40:465–475. 2014.
View Article : Google Scholar : PubMed/NCBI
|