Introduction
Arteriovenous malformation (AVM) is an abnormal
connection between arteries and veins that bypasses the capillary
system. AVM lacks the dampening effect of capillaries on the blood
flow, which means that the malformation can become progressively
larger over time as the amount of blood flowing through it
increases (1–3). An AVM confined to the nasal cavity is
rare, and its high recurrence rate may be due to the use of
embolization with incomplete or no resection (2,4,5). A combined approach of complete surgical
resection with prior superselective embolization is the treatment
of choice. Following resection, the reconstruct of facial defects
is challenging, particularly in the nasal area (1). Only a few studies have reported the use
of either local or free flaps alone for the reconstruction of AVMs
involving the nasal cavity following resection (1–5); however,
a combination of free and local flaps may be used to achieve an
acceptable cosmetic result. The present study reports a case of
nasal reconstruction using a free radial forearm flap in
combination with a forehead flap, following the resection of an AVM
confined to the nasal cavity.
Case report
A 63-year-old male presented to the Department of
Otolaryngology, Chi-Mei Medical Center (Tainan, Taiwan) in December
2011 with a history of nasal bleeding that had occurred
intermittently for ~5 years. The patient also complained of blurred
vision, particularly in the right eye. The symptoms were aggravated
with time, and the patient visited the hospital for assistance.
Sinoscopy showed that the cause of the bleeding was a tumor in the
left nasal cavity. Magnetic resonance imaging and computed
tomography scans showed soft-tissue mass lesions with post-contrast
enhancement in the left nasal cavity, consistent with a vascular
lesion, such as an AVM (Fig.
1A-C).
Angiography showed a large tangle of abnormal
vascular channels in the nasal cavity, with a blood supply
originating from the infraorbital and sphenopalatine branches of
the left internal maxillary artery, the bilateral facial arteries
and the left ophthalmic artery, and with early venous drainage into
dilated and tortuous areas of the nasal mucosal vessels, bilateral
facial veins (more in the right side), bilateral superior
ophthalmic veins (more in the right side) and frontal scalp veins
on the right side (Fig. 1D). AVM was
highly suspected. Pre-operatively, the patient underwent
superselective embolization, including occlusion of the bilateral
sphenopalatine arteries, right descending palatine artery, a small
branch of the left superficial temporal artery and the left facial
artery.
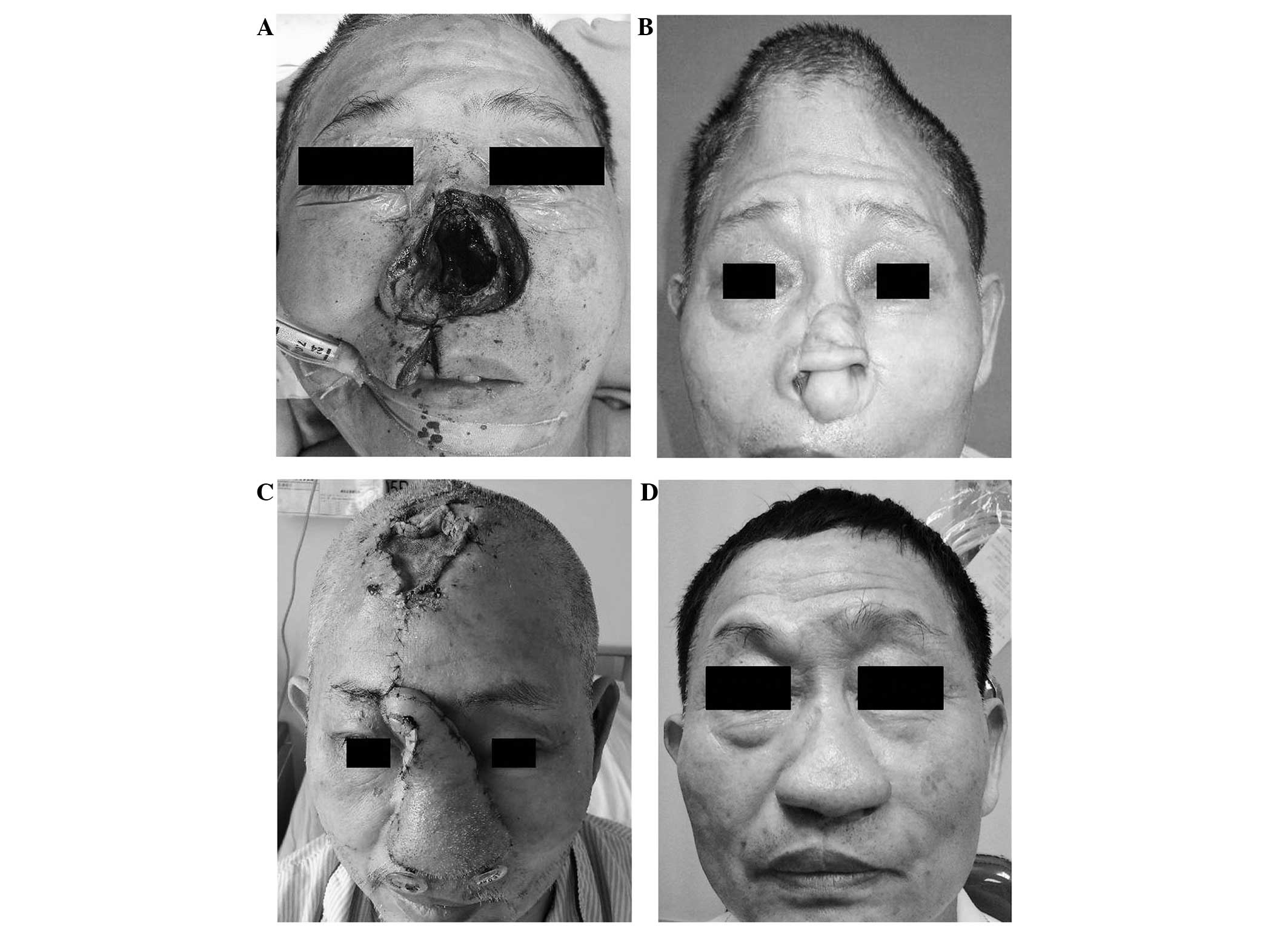
The following day, the patient underwent a complete
resection of the vascular tumor with sinoscopic assistance using a
lateral rhinotomy approach (Fig. 2A).
Subsequently, nasal reconstruction using a radial forearm free flap
and a split thickness skin graft was performed, due to the
extensive involvement of the vascular tumor in the nasal area.
Implantation of tissue expanders on the forehead was performed at
the same time for later nasal reconstruction (Fig. 2B). Pathological examination confirmed
an AVM. Post-operatively, the blurred vision subsided. Sequential
nasal reconstruction surgeries, including a reconstruction using a
full-thickness paramedian forehead flap, a reconstruction of the
nasal dorsum, columella and upper lateral cartilage with rib
cartilage graft, and a nasal alar reconstruction with left ear
cartilage, were performed in April 2012 (Fig. 2C). Flap deviation was also performed
in April, while flap debulking was performed in June 2012. During
1.5 years of follow-up, no recurrence was noted and the patient
possessed an acceptable cosmetic appearance (Fig. 2D). The patient remains under follow-up
and the wound has healed well.
Discussion
An AVM is a structural vascular abnormality in which
arterial vessels connect with venous vessels without capillary
connections. Progression may be due to stimuli, including
pregnancy, trauma, infection and puberty, or iatrogenic injuries,
including biopsy, proximal ligation and subtotal excision (1,2). The
abnormality is a high-flow vascular malformation with multiple
low-resistance shunts (2,3). In the present patient, angiography
demonstrated a large tangle of abnormal vessels in the nasal
cavity, with a blood supply originating from the infraorbital and
sphenopalatine branches of the left internal maxillary artery, the
bilateral facial arteries and the left ophthalmic arteries, and
with early venous drainage into dilated and tortuous areas of the
nasal mucosal vessels, bilateral facial veins (more in the right
side), bilateral superior ophthalmic veins (more in the right side)
and the right frontal scalp vein.
Clinically, the overlying skin of the AVM may appear
normal, or as a pulsatile mass, red in color and with an increased
local temperature (3,4).
Other symptoms and signs may include pain,
ulceration, excessive growth, profuse bleeding and even congestive
heart failure (3,4). In the present patient, constant nasal
bleeding was the major complaint. The patient also experienced
blurred vision, particularly in the right eye, which could have
been associated with multiple shunts of the AVM involving the
ophthalmic artery and vein (particularly on the right side).
Following the complete resection of the nasal lesion, the blurred
vision subsided, which strongly suggested that it was caused by the
nasal AVM.
The Schobinger classification is one of the staging
systems for AVM and includes the following stages: Stage I,
blushing and warm cutaneous lesions; stage II, bruit, audible
pulsations and expanding lesions; stage III, pain, ulceration,
bleeding and infection; and stage IV, cardiac failure (5). The present patient exhibited stage III
disease.
In the present study, pathological examination
confirmed an AVM, however, occasionally, distinguishing between
AVMs and hemangiomas is confusing. The use of elastic tissue stains
is an useful ancillary tool to distinguish between these two
conditions. The presence of arteries and arterioles is an integral
feature of an AVM. The presence of intra-lesional nerves can also
be useful to distinguish between AVMs and hemangiomas on
hematoxylin and eosin-stained sections.
AVMs are mainly found in the intracranial region
(6). Extracranial involvement is
uncommon; the most common sites are the cheeks, ears, nose and
forehead (in order of frequency in the extracranial region)
(7). Other rare locations, such as
the mandible, have also been reported (8). Following a search on PubMed (http://www.ncbi.nlm.nih.gov/pubmed), certain
studies on nasal AVM were found; however, lesions confined only to
the nasal cavity were rare, as was the resection of this type of
defect. Only a few studies have reported the use of either local or
free flaps alone for the reconstruction of AVM involving the nasal
cavity following resection (1–5). One study
described the use of a combination of free radial forearm and
forehead flaps without prosthesis for nasal reconstruction in 2011
(9); however, for the management of
nasal AVM, reconstruction using a combination of free radial
forearm and local forehead flaps following resection of AVM
confined to the nasal cavity has not been reported in the
literature (1–6).
Pre-operatively deciding the extent of the resection
of the AVM is crucial. Magnetic resonance imaging is used to
determine the extent of the soft-tissue involvement, while computed
tomography is able to delineate any bone involvement (10). Selective angiography is useful for the
investigation of AVM, as it can identify specific vascular
abnormalities and demonstrate the flow characteristics, feeding
vessels and dangerous anastomoses (11).
Highly selective embolization as a single treatment
modality is rarely successful with AVMs, due to the later
development of novel vascular pathways. Embolization leads to a
marked reduction in the blood flow within the vascular tumor, which
decreases surgical blood loss and permits a complete resection of
the tumor (11); however,
pre-operative embolization should not be used to reduce the extent
of resection (12). Partial resection
is not curative and should be avoided, since revascularization and
novel collateral circulation can lead to recurrence (7), and may encourage further shunting and
reexpansion (12). Proximal artery
ligation alone should also be avoided for the treatment of AVMs due
to novel collateral circulation (3,4).
A multidisciplinary approach is recommended for the
management of an AVM (2). The
combined use of a complete surgical excision and prior
superselective embolization is the treatment of choice for AVMs
(10,11,13). It
has been shown that it is best for the complete surgical resection
to be performed within 48 h of highly selective embolization, as
the resulting inflammation neutralizes hemodynamic benefits, making
surgery more challenging (2–4). In the present patient, superselective
embolization was performed first, then 1 day later, in order to
avoid recurrence, a complete surgical resection of the lesions in
the nasal cavity was performed. Due to the extensive involvement of
the nasal AVM, the nasal defect was hard to reconstruct without the
use of a flap. Reconstruction should include the internal nasal
lining. Use of distant tissue through microvascular transfer is a
way of bringing this lining to within the nose (9,14,15). In the present study, the free radial
forearm flap was used for the lining. The tissue expander was also
placed in the forehead, and further nasal reconstruction was
performed. During the surgeries, a full-thickness paramedian
forehead flap was used. The nasal dorsum, columella and upper
lateral cartilage area were reconstructed using rib cartilage
graft. A nasal alar reconstruction was achieved using the left ear
cartilage.
After 1.5 years of follow-up, no recurrence was
noted in the present patient. The cosmetic results and olfactory
perception of the patient were acceptable; however, rhinomanometry
showed an increased inspiratory airflow resistance in the right
naris compared with the left, which may have been due to the
smaller nasal pathway through the right naris with greater air flow
resistance.
In conclusion, AVM confined to the nasal cavity is
considerably rare. Reconstruction using a combination of and local
forehead flaps following resection of an AVM confined to the nasal
cavity had not previously been reported in the literature. The
present study reported a case of complete resection and
reconstruction using a free radial forearm flap combined with a
forehead flap, with acceptable cosmetic results. It should be noted
that the differential diagnosis of blurred vision should include
nasal diseases, such as AVM.
References
|
1
|
Weinzweig N, Chin G, Polley J, Charbel F,
Shownkeen H and Debrun G: Arteriovenous malformation of the
forehead, anterior scalp, and nasal dorsum. Plast Reconstr Surg.
105:2433–2439. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bhandari PS, Sadhotra LP, Bhargava P, Bath
AS, Mukherjee MK and Maurya S: Management strategy for facial
arteriovenous malformations. Indian J Plast Surg. 41:183–189. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kohout MP, Hansen M, Pribaz JJ and
Mulliken JB: Arteriovenous malformations of the head and neck:
Natural history and management. Plast Reconstr Surg. 102:643–654.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pompa V, Valentini V, Pompa G, Di Carlo S
and Bresadola L: Treatment of high flow arteriovenous malformations
(AVMs) of the head and neck with embolization and surgical
resection. Ann Ital Chir. 82:253–259. 2011.PubMed/NCBI
|
|
5
|
Pompa V, Brauner E, Bresadola L, Di Carlo
S, Valentini V and Pompa G: Treatment of facial vascular
malformations with embolization and surgical resection. Eur Rev Med
Pharmacol Sci. 16:407–413. 2012.PubMed/NCBI
|
|
6
|
Nocini PF, Fior A, Tolo C and Bertossi D:
Arteriovenous Malformation of the nasal ala: A case report. J Oral
Maxillofac Surg. 58:1303–1309. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Woo HJ, Song SY, Kim YD and Bai CH:
Arteriovenous malformation of the external ear: A case report.
Auris Nasus Larynx. 35:556–558. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chhoeurn V, de Villa GH and Lo LJ: Osseous
regeneration after embolization of mandibular arteriovenous
malformation. Chang Gung Med J. 26:937–942. 2003.PubMed/NCBI
|
|
9
|
Menick FJ and Salibian A: Microvascular
repair of heminasal, subtotal, and total nasal defects with a
folded radial forearm flap and a full-thickness forehead flap.
Plast Reconstr Surg. 127:637–651. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Coskun BU, Sozen E, Basak T, Alkan S and
Dadas B: Arteriovenous malformation of the nasopharynx: A case
report. Int J Pediatr Otorhinolaryngol. 69:1287–1290. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim KS: Arteriovenous malformation in the
pretragal region: Case report. Head Neck. 33:281–285. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lowe LH, Marchant TC, Rivard DC and
Scherbel AJ: Vascular malformations: Classification and terminology
the radiologist needs to know. Semin Roentgenol. 47:106–117. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nekooei S, Hosseini M, Nazemi S and
Talaei-Khoei M: Embolization of arteriovenous malformation of the
maxilla. Dentomaxillofacial Radiol 35: 451–455, 2006. Antunes MB
and Chalian AA: Microvascular reconstruction of nasal defects.
Facial Plast Surg Clin North Am. 19:157–162. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Antunes MB and Chalian AA: Microvascular
reconstruction of nasal defects. Facial Plast Surg Clin North Am.
19:157–162. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Moore EJ, Strome SA, Kasperbauer JL,
Sherris DA and Manning LA: Vascularized radial forearm free tissue
for lining in nasal reconstruction. Laryngoscope. 113:2078–2085.
2003. View Article : Google Scholar : PubMed/NCBI
|