Introduction
Lung cancer severely compromises human health, and
is nowadays one of the most common malignant tumors worldwide
(1). Since the prophase of clinical
symptoms are not obvious, approximately 80% of patients are already
in middle or late periods while visiting doctors, and thus surgery
does not constitute a viable option (2).
In recent years, RFA has been gradually introduced
for lung cancer treatment (3). It has
key advantages, e.g., precise treatment effect, high safety and
small trauma, which has become an important part in non-surgery
treatment of lung cancer (3,4). Radiofrequency ablation (RFA) can improve
the temperature of tumor tissue in a short period of time and make
tumor cells degenerated and necrotic, thus reaching the aim of
killing tumor tissue, which has achieved great clinical effect
(5–7).
Chemotherapy also plays an important role in cancer treatment
process. Non-small cell lung cancer (NSCLC) accounts for 80% of
lung cancer types.
In this study, we investigated the experience of
middle and late period NSCLC treatment by RFA combined whole-body
chemotherapy, single RFA treatment and whole-body chemotherapy
treatment. We analyzed the effect of RFA combined chemotherapy on
middle and late period NSCLC.
Patients and methods
General information
A total of 85 cases of NSCLC patients admitted to
the Department of Oncological Surgery (Hebei, China) from June,
2013 to December, 2013 were selected. The patients were in clinical
phase III or IV, and diagnosed as NSCLC by pathology. There were 50
males and 35 females, aged 44–76 years with a median age of 58
years. There were 35 cases in the RFA combined chemotherapy group,
including 22 males and 1 female aged 44–65 years; 28 cases in the
RFA group with 18 males and 10 females aged 58–76 years; and 22
cases in the chemotherapy group with 15 males and 7 females aged
52–72 years.
Treatment methods
RFA-combined chemotherapy group
The 85 cases were examined for routine blood tests,
electrocardiogram and chest computed tomography (CT) scan before
surgery. The RFA treatment under the guidance of CT scan. Cool-tip
RFA system (Covidien; Medtronic, Minneapolis, MN, USA) was used,
and RFA needle with 20 or 30 mm was selected according to the size
of the tumor. The CT scanning was carried out after localizing
marker on body surface, and determining needle insertion point
according to body surface localization after selecting treatment
layer, and needle insertion angle and depth was measured. Regular
sterilization and sheet paving was performed. For anesthesia, 2%
lidocaine hydrochloride was used. The needle was gradually inserted
according to needle insertion point and angle, and CT scan was
performed to guide needle depth.
The treatment was started when the RFA needle was
within the tumor tissue. The treatment power was 120 W, and the
time was 10 min. Multiple times of RFA treatment were carried out
according to the size of the tumor for complete cover of the tumor
tissue according to treatment. After the treatment, necessary care
was provided, e.g., oxygen uptake, hemostasis, anti-infection and
fluid replacement. After surgery, blood tests were performed again.
In the groups without chemotherapy, cisplatin + docetaxel was
administered. For chemotherapy, 75 mg/m2 of docetaxel
was added to 0.9% NaCl of 250 ml, intravenous drip on the first
day. Along with 75 mg/m2 of docetaxel 500 ml of 0.9%
NaCl was added for 3 days, separately. The chemotherapy plan
included 6 treatment courses with 21 days of a treatment
course.
RFA group
Treatment methods were the same as the
radiofrequency methods in the RFA combined chemotherapy group.
Chemotherapy group
The treatment methods and period was the same as the
chemotherapy plan in the RFA combined chemotherapy group.
Patients in the three groups were re-examined for a
CT scan 3 and 6 months after surgery. During this process,
treatment was provided on time if there was bleeding in local tumor
tissue in RFA combined chemotherapy group and RFA group.
Data collection and statistical
processing
CT value and tumor sizes
For all groups, the tumor CT scan and tumor size
(longest diameter) was measured at each follow-up. SPSS 13.0
statistical software for Windows (IBM; Chicago, IL, USA) was used
to analyze CT value. The results were expressed as mean ± SD, and
the Student's t-test was used to carry out statistical analysis.
P<0.05 was considered to indicate a statistically significant
difference.
The effects were assessed 6 months after RFA
surgery. SPSS 13.0 statistical software was used to assess
treatment effect. The results are expressed as percentage (%), and
χ2 test used for statistical analysis, with P<0.05
considered to indicate a statistically significant difference.
Results
Change of CT value
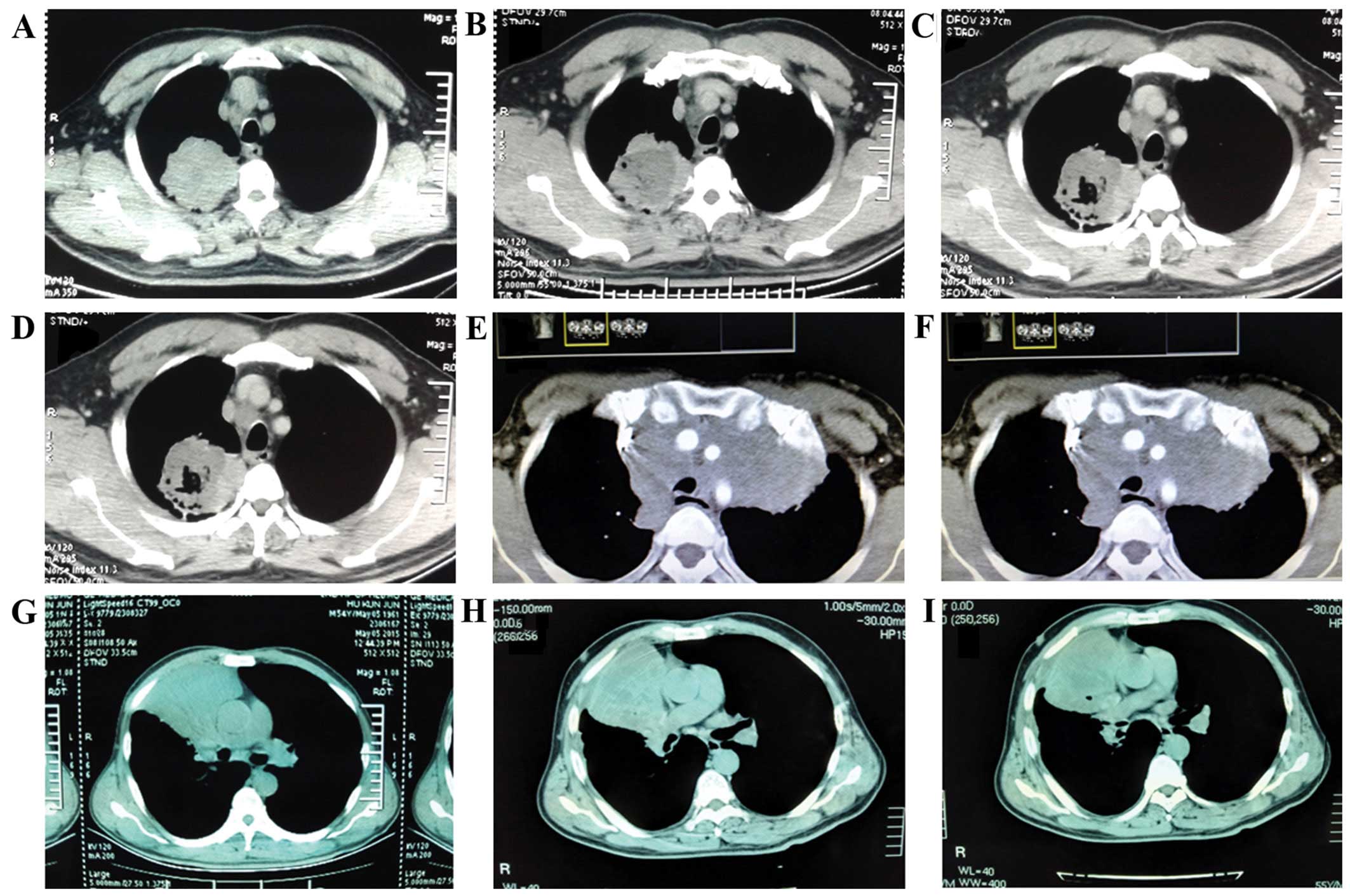
In the RFA combined chemotherapy group, the CT value
before surgery was 48.9±12.7 HU (Fig.
1A), 3 months after surgery was 27.5±10.8 HU (Fig. 1B), and 6 months after surgery
24.6±11.2 HU (Fig. 1C). In RFA group,
CT value before surgery was 50.4±13.5 HU (Fig. 1D), 3 months after surgery it was
30.4±11.0 HU (Fig. 1E), and 6 months
after surgery 26.6±14.7 HU (Fig. 1F).
For the chemotherapy group, the CT value before surgery was
45.4±15.0 HU (Fig. 1G), 3 months
after surgery it was 43.1±15.8 HU (Fig.
1H), and 6 months after surgery 46.2±13.5 HU (Fig. 1H) (Table
I).
 | Table I.Changes of CT value. |
Table I.
Changes of CT value.
| Groups | CT value before
surgery (HU) | CT value 3 months
after surgery (HU) | CT value 6 months
after surgery (HU) |
|---|
| RFA combined
chemotherapy | 48.9±12.7 | 27.5±10.8 | 24.6±11.2 |
| RFA | 50.4±13.5 | 30.4±11.0 | 26.6±14.7 |
| Chemotherapy | 45.4±15.0 | 43.1±15.8 | 46.2±13.5 |
Before surgery, CT value of the three groups were
not statistically significant (P>0.05). CT value of RFA combined
chemotherapy group decreased significantly after surgery
(P<0.05). CT value of RFA group decreased significantly after
surgery (P<0.05). CT value of chemotherapy group did not change
significantly (P>0.05). Compared with chemotherapy group, CT
value of RFA combined chemotherapy group and RFA group decreased
significantly after surgery (P<0.05) (Table II).
 | Table II.Effect assessment. |
Table II.
Effect assessment.
| Groups (n) | CR (n) | PR, n (%) | SD, n (%) | P, n (%) |
|---|
| RFA combined
chemotherapy (35) | 0 | 28 (80.0) | 5 (14.3) | 2 (5.7) |
| RFA (28) | 0 | 18 (64.3) | 5 (17.9) | 5 (17.9) |
| Chemotherapy
(22) | 0 | 6 (27.3) | 10 (45.5) | 6 (27.3) |
The effect assessment
In RFA combined chemotherapy group, there was no
complete response (CR) (0/35), partial response (PR) 80% (28/35),
stable disease (SD) 14.3% (5/35), P 5.7% (2/35). In the RFA group
there was no CR (0/28), PR 64.3% (18/28), SD 17.9% (5/28), P
17.9%(5/28). In the chemotherapy group, there was no CR (0/22), PR
27.3% (6/22), SD 45.5% (10/22), P 27.3% (6/22) (Table II).
The effective rate (CR+PR) of the RFA combined
chemotherapy group was higher than that of the RFA and chemotherapy
groups (P<0.05). By contrast, the progressive rate (P) of the
RFA combined chemotherapy group was significantly lower than that
of the RFA and chemotherapy groups (P<0.05) (Table II).
Postoperative complications
In the RFA combined chemotherapy group, there was no
death related to operation; 3 cases of chest pain, 5 cases of
pneumothorax, 1 case received cavitas thoracis paracentesis once, 1
case needed cavitas thoracis closed type drainage, whereas in other
3 cases cavitas thoracis was absorbed spontaneously; 7 cases have
sputum with blood, no hemoptysis, no intra-lung bleeding; 15 cases
had fever, with the highest temperatures under 38.5°C, and were
obviously improved after physical cooling. For the RFA group, there
was no death related to operation; 3 cases chest pain, 4 cases of
pneumothorax, 1 case received cavitas thoracis paracentesis 1 time
in and after surgery respectively, and other 3 cases absorbed by
themselves; 5 cases had sputum with blood, 1 cases hemoptysis, no
intra-lung bleeding; 12 cases had fever, with the highest
temperatures under 38.5°C, and obvious improvement after physical
cooling.
Discussion
In recent years, there has been a gradual increase
of lung cancer incidence (1), which
is now the malignant tumor with the highest incidence and
mortality. There is a study indicating that a 5-year survival rate
of phase I NSCLC patients without treatment is only 6%, and the
median survival time is 9–14 months (2). According to statistics, <20% patients
can be offered surgery. Therefore, the position of non-surgery in
lung cancer treatment becomes more important.
RFA is a new technique aiming at tumor treatment.
The principle uses high frequency electromagnetic waves produced by
radiofrequency electric current to make intra-cellular polar
molecules agitate and friction to generate heat, leading to protein
degeneration and leading to irreversible clotting necrosis, and
thus to killing of tumor cells. RFA has already achieved good
effect in liver cancer treatment. Since there is ample blood
circulation and breathing heat elimination in the lung, the heat
can dissipate, it has been shown that the amount of blood
circulation is low in lung tumor tissue, while a high amount of air
in lung can speed the accumulation of heat, which causes rapid
temperature increase, known as ‘side-effect’, therefore, RFA has
obvious advantage when applied to lung cancer treatment (3,4). RFA can
kill the cancer cells in treatment area, reduce tumor load, as well
as increase the sensitivity of cancer cells to chemotherapy
medicine, which is an important component of the comprehensive
treatment to middle and late period NSCLC patients (5). Compared to traditional surgery
treatment, RFA has obvious advantages including precise treatment
effect, small lesion, short surgery time, fast recovery, capacity
of repeated treatment, less complications and high safety level
(6,7).
The main complications are pneumothorax, fever, thoracalgia, cough
and hemoptysis. Most complications have slight symptoms and only a
few need special treatment.
Chemotherapy for NSCLC is currently mainly based on
platinum, which greatly improves the survival time and quality of
life of the patients (8). There is a
study comparing the clinical effect of three generations of
anticancer drugs. Docetaxel and cisplatin or TP plan has become the
first-tier chemotherapy plan for NSCLC (8).
In the present study, RFA accomplished precise
localization under the guidance of CT, and we designed a needle
spread plan according to CT image and treatment range of RFA,
making the radiofrequency treatment range fully cover the tumor
tissue. It can treat multiple tumor lesions at one time or treat
the same lesion many times, as there is no blood supply at the
tumor tissue clotting necrosis area after RFA treatment (9). However, the tumor size may not change or
even increases, considering it may be related to tumor tissue
clotting necrosis, oedema or surrounding acute inflammation
(10). Therefore, we can assess the
treatment effect according to the results of
postoperative-intensified CT, and take multiple RFA according to
the results to kill the remaining tumor tissue or completely block
the blood supply of tumor tissue, to achieve better treatment
effect. The research findings have shown that the lesion may
increase 1–3 months after RFA, and gradually decrease after months
(11). If there is not obvious
decrease of the tumor volume but intensified CT examination shows
no change of the CT value, then it indicates the treatment is
effective (11). This study showed
that in some patients, follow-up CT scan revealed no obvious tumor
volume changes in short-term after RFA or a small portion of cases
had their tumor volume increased, and all of the CT scan values
significantly decreased compared to before, and some cases it
showed obvious cavity and diffluented necrosis in the tumor tissue.
It suggested the effectiveness of the treatment, which was
consistent with research results by different group (12). The CT value of the RFA combined
chemotherapy group significantly decreased, while its effective
rate (CR+PR) was higher than that of the RFA and chemotherapy
groups, indicating effective treatment.
The findings of the present study show that RFA and
chemotherapy have an important function in the treatment of middle
and late period NSCLC. In the treatment of the middle and late
period NSCLC, RFA combined chemotherapy can improve the treatment
effect, and retard pathogenetic progress, with convenient
operation, small side-effects and can be repeatedly applied, which
is worthy of generalization. Some studies indicated that although
compared to traditional chemoradiotherapy, single RFA treatment for
lung cancer has the advantage of being able to control local lesion
and improving life quality of patients, although it cannot improve
survival rate of patients with local late period NSCLC (13,14).
However, this study only investigated the short-term effect of
RFA-combined chemotherapy on the middle and late period NSCLC.
Further studies are required to investigate whether it can improve
the long-term effect of factors such as tumor recurrence and
metastasis, survival period and quality of life.
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Raz DJ, Zell JA, Ou SH, Gandara DR,
Anton-Culver H and Jablons DM: Natural history of stage I non-small
cell lung cancer: implications for early detection. Chest.
132:193–199. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Liu B, Liu L, Li Y, Wang H, Hu M, Qian K,
Wang R and Zhi X: Survival after radiofrequency ablation for 100
cases of lung neoplasms. Zhongguo Fei Ai Za Zhi. 14:335–339.
2011.(In Chinese). PubMed/NCBI
|
|
4
|
Oshima F, Yamakado K, Akeboshi M, Takaki
H, Nakatsuka A, Makita M and Takeda K: Lung radiofrequency ablation
with and without bronchial occlusion: experimental study in porcine
lungs. J Vasc Interv Radiol. 15:1451–1456. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhao J, Wu Y, Wang Y, et al: Treatment of
local late period NSCLC by RFA combined chemoradiotherapy. Cancer
Res Prev Treat. 8:495–497. 2004.
|
|
6
|
Iguchi T, Hiraki T, Gobara H, Mimura H,
Fujiwara H, Tajiri N, Sakurai J, Yasui K, Date H and Kanazawa S:
Percutaneous radiofrequency ablation of lung tumors close to the
heart or aorta: evaluation of safety and effectiveness. J Vasc
Interv Radiol. 18:733–740. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Qian K, Zhang Y, Zhi XY, Liu BD, Su L, Li
Y and Wang H: Study on the safety of radiofrequency ablation in
patients with lung cancer above 70 years old. Chinese J Clinicians
(Electronic Edition). 7:5332–5334. 2013.(In Chinese).
|
|
8
|
Grossi F, Aita M, Defferrari C, Rosetti F,
Brianti A, Fasola G, Vinante O, Pronzato P and Pappagallo G: Impact
of third- generation drugs on the activity of first-line
chemotherapy in advanced non-small cell lung cancer: a
meta-analytical approach. Oncologist. 14:497–510. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goldberg SN, Gazelle GS and Mueller PR:
Thermal ablation therapy for focal malignancy: a unified approach
to underlying principles, techniques, and diagnostic imaging
guidance. AJR Am J Roentgenol. 174:323–331. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Liu B, Zhi X, Liu L, Hu M, Wang R, Xu Q,
Zhang Y and Su L: Evaluation of three-dimensional reconstruction CT
in percutaneous radiofrequency ablation (RFA) of the unresectable
lung tumor with a clustered electrode. Zhongguo Fei Ai Za Zhi.
12:775–779. 2009.(In Chinese). PubMed/NCBI
|
|
11
|
Anderson EM, Lees WR and Gillams AR: Early
indicators of treatment success after percutaneous radiofrequency
of pulmonary tumors. Cardiovasc Intervent Radiol. 32:478–483. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Higaki F, Okumura Y, Sato S, Hiraki T,
Gobara H, Mimura H, Akaki S, Tsuda T and Kanazawa S: Preliminary
retrospective investigation of FDG-PET/CT timing in follow-up of
ablated lung tumor. Ann Nucl Med. 22:157–163. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang J, Wang Y and Zhao J: Short-term and
long-term effect of RFA on local late period NSCLC. Int Med Health
Guidance News. 12:20–23. 2006.(In Chinese).
|
|
14
|
Mohamed Lotayef, Azza Taher, Hanna Attia,
Azza Nasr, El Hossieny Hisham, Mohammed Mahmoud and Noha Essam: A
clinic-epidemilogical study of cases of locally advanced non small
cell lung cancer (NSCLC) that received radiotherapy at NCI Cairo in
the period from 2001–2010. J Cancer Ther. 5:542–551. 2014.
View Article : Google Scholar
|