Introduction
Diagnosing polyneuropathy, organomegaly,
endocrinopathy, and M protein and skin changes (POEMS) syndrome
does not require the patient to present all symptoms in the
aforementioned acronym (1).
Furthermore, the POEMS acronym does not include all POEMS
syndrome-associated symptoms, and there is a Castleman disease
variant of POEMS syndrome that may be associated with clonal plasma
cell disorder (2). POEMS syndrome is
a rare paraneoplastic syndrome associated with an underlying plasma
cell disorder (2). Cases of POEMS
syndrome have been reported in Japan (3–5), France,
the United States, China and India (6–9). However,
the incidence and prevalence of POEMS syndrome is unknown (10). Though the mechanism by which plasma
cells cause POEMS syndrome remains to be fully understood,
increased levels of vascular endothelial growth factor (VEGF) may
be a factor (11).
POEMS syndrome is potentially fatal and is
associated with a substantial deterioration in quality of life
through neuropathy, anasarca, thromboembolic events and cachexia
(12,13). Early diagnosis and a multidisciplinary
approach may increase the likelihood of reducing long-term
irreversible morbidity.
Weakness in the upper and lower limbs is a common
symptom of multiple diseases, including neuromuscular disorders
(14), amyotrophic lateral sclerosis
(15), multiple sclerosis,
Guillain-Barre syndrome, transverse myelitis (16), hypovitaminosis D (17) and POEMS syndrome. Hence, presentation
with weakness in the upper and lower limbs in patients with POEMS
syndrome may not result in the correct diagnosis. The patient with
POEMS syndrome described in the present study initially presented
with weakness in the upper and lower limbs 2 years ago, and
subsequently succumbed to respiratory failure at age 50 due to
delayed diagnosis of POEMS syndrome. The present study intends to
improve the understanding of POEMS syndrome among healthcare
professionals.
Case report
On 3 March 2014, a 50-year-old female patient was
admitted to the Department of Endocrinology, Qilu Hospital of
Shandong University (Jinan, China), complaining of progressive
weakness in her upper and lower limbs, which frequently failed.
Furthermore, the patient was experiencing tingling, numbness and
burning in her feet. The patient had a 3-year history of diffuse
hyperpigmentation and slight anasarca, and a 2-month history of
lumbodynia and debilitation, pain and numbness all over her body.
In addition, the patient was diagnosed with type 2 diabetes at the
Affiliated Hospital of Binzhou Medical School (Binzhou, China).
Written informed consent was obtained from the patient for the
publication of the present case report and any accompanying
images.
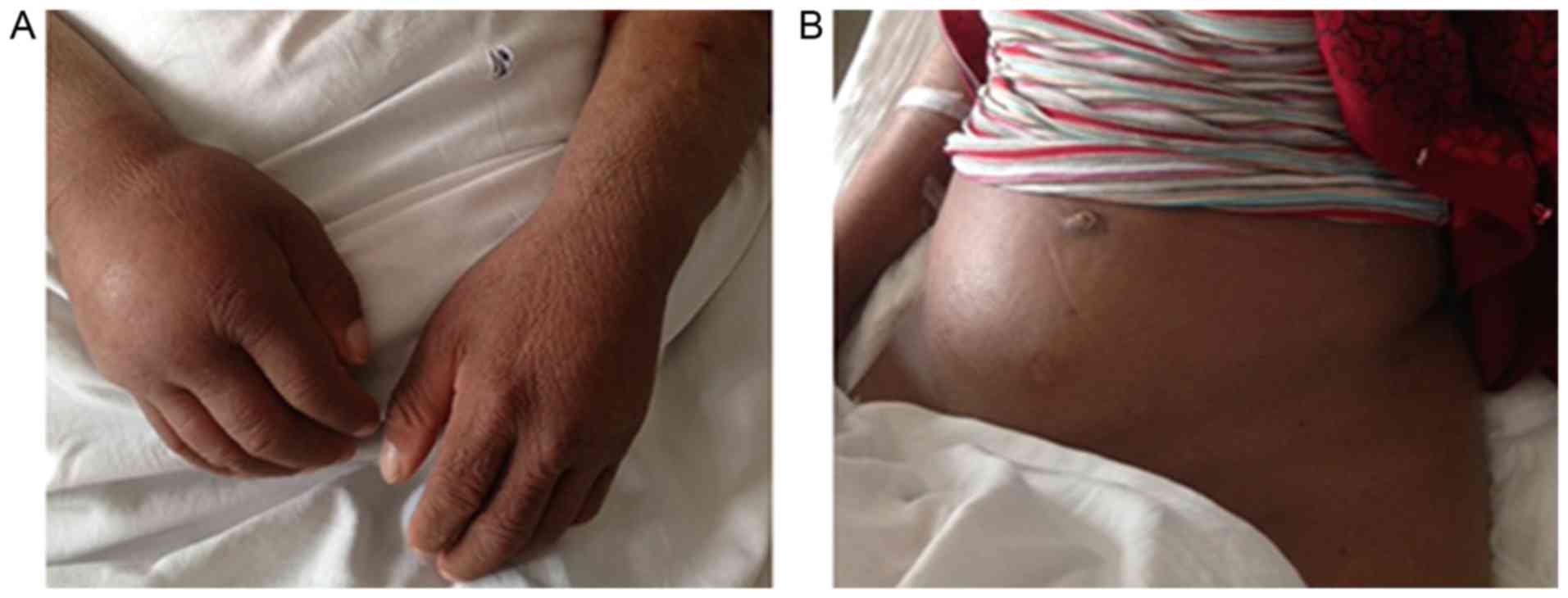
On admission, a physical examination revealed
chronic facies (pale or grey look caused by chronic disease) and
unstable vital signs. Measurements were taken, including body
temperature, 36.0°C (normal range, 36–37°C); respiration rate, 19
breaths/min (normal range, 16–20 breaths/min); heart rate, 78
beats/min (normal range, 60–100 beats/min); and blood pressure,
197/107 mmHg (normal range, ≤120/80 mmHg). Physical examination
revealed diffuse hyperpigmentation, which was particularly severe
on the upper trunk and limbs; dry skin; hypertrichosis (Fig. 1A); and leukonychia. The patient
exhibited continued mild edema in her facial tissues and lower
limbs (Fig. 1B). Palpable, soft
rubbery lymph nodes were revealed in the axillary fossa. The
patient exhibited splenomegaly and amenorrhea. Bilateral rales were
heard with a stethoscope on auscultation. The body mass of the
patient had decreased by ~10 kg in the past year.
The blood cell count demonstrated an increase of
platelets (4.56×1011 cells/l), and a decrease in albumin
(29.3 g/l) and albumin/globulin ratio (0.88:1). However,
electrolytes, liver and renal function were within normal limits.
Analysis of blood coagulation serials revealed increased
prothrombin time, increased standardization of prothrombin time
ratio, decreased prothrombin time activity, activated partial
thromboplastin time, increased plasma D-Dimer. These results
revealed that the patient exhibited coagulation disorders. The
results of endocrine hormone analysis revealed decreased free
triiodothyronine, tetraiodothyronine and thyroglobulin, and
increased thyroid-stimulating hormone, consistent with the symptoms
of hypothyroidism. Symptoms of endocrinopathy included increased
prolactin (PRL) and adrenocorticotropic hormone (ACTH), decreased
testosterone (TEST), hypothyroidism, type 2 diabetes and empty
sella turcica (Table I). Vitamin
B12 levels were 145.3 pg/ml, which also decreased
compared with the lower limits of the normal range (190–940
pg/ml).
 | Table I.Laboratory test results of the initial
assessment of the patient. |
Table I.
Laboratory test results of the initial
assessment of the patient.
| A, Blood cells |
|---|
|
|---|
| Type of blood
cell | Value | Change relative to
normal value | Normal value |
|---|
| Red blood cells,
×109 cells/l | 5.24 |
| 3.50–5.50 |
| White blood cells,
×109 cells/l | 5.80 |
| 4.00–10.00 |
| Neutrophils,
×109 cells/l | 2.80 | ↓ | 3.00–5.00 |
| Lymphocytes,
×109 cells/l | 2.30 |
| 1.00–3.00 |
| Monocytes,
×109 cells/l | 0.50 |
| 0.07–0.33 |
| Eosinophils,
×109 cells/l | 0.10 |
| 0.05–0.50 |
| Basophils,
×109 cells/l | 0.00 | ↓ | 0.02–0.05 |
| Platelets,
×109 cells/l | 456.00 | ↑ | 100.00–300.00 |
| ESR, mm/h | 13.00 |
| 0.00–20.00 |
|
| B, Proteins |
|
| Type of protein | Concentration | Change relative to
normal concentration | Normal
concentration |
|
| Albumin, g/l | 29.30 | ↓ | 40.00–55.00 |
| Globulin, g/l | 33.20 |
| 0.00–40.00 |
| Albumin/globulin | 0.88:1 | ↓ | 1.20–2.40 |
| Ig G, g/l | 15.00 |
| 7.00–16.00 |
| Ig A, g/l | 5.43 | ↑ | 0.70–4.00 |
| Ig M, g/l | 0.88 |
| 0.40–2.30 |
| Ig E, g/l | 51.50 |
| 0.00–100.00 |
| C3, g/l |
0.56 | ↓ | 0.90–1.80 |
| C4, g/l |
0.16 |
| 0.10–0.40 |
| κ light chain,
g/l |
4.18 | ↑ | 1.70–3.70 |
| λ light chain,
g/l |
2.58 | ↑ | 0.90–2.10 |
| κ/λ | 1.62:1 |
| 1.35–2.65 |
|
| C, Coagulation
serials |
|
|
| Value | Change relative to
normal value | Normal value |
|
| Prothrombin time,
sec | 21.10 | ↑ | 11.00–14.50 |
| INR | 1.90 | ↑ | 0.80–1.20 |
| Prothrombin time
activity, % | 41.00 | ↓ | 70.00–120.00 |
| APTT, sec | 86.30 | ↑ | 28.00–45.00 |
| Fibrinogen,
g/l | 2.11 |
| 2.00–4.00 |
| Plasma D-Dimer,
µg | 3.77 | ↑ | 0.00–0.50 |
|
| D, Hormone |
|
| Type of
hormone | Value | Change relative to
normal value | Normal value |
| Free
triiodothyronine, pmol/l | 2.21 | ↓ | 2.30–6.30 |
| Free
tetraiodothyronine, pmol/l | 6.28 | ↓ | 10.30–24.50 |
| Thyroid-stimulating
hormone, UIU/ml | 6.19 | ↑ | 0.35–5.50 |
| Thyroglobulin,
ng/ml | 0.32 | ↓ | 1.40–7.80 |
| Prolactin,
ng/ml | 48.26 | ↑ | 3.40–24.10 |
| Testosterone,
ng/ml | <0.03 | ↓ | 0.06–0.82 |
| ACTH, pg/ml;
00:00 | 21.63 | ↑ | 0.00–10.00 |
| ACTH, pg/ml;
08:00 | 139.70 | ↑ | 4.70–48.80 |
| ACTH, pg/ml;
16:00 | 14.57 |
| 0.00–46.00 |
| Vitamin
B12, pg/ml | 145.30 | ↓ | 190.00–940.00 |
An electromyography (EMG) test was used to identify
neurological symptoms. The EMG test revealed motor and sensory
polyneuropathy, with typical demyelination featuring at the
proximal and distal ends of peripheral nerves in the four limbs of
the patient. Administering hydrocortisone sodium succinate (100
mg/day) improved the neurological symptoms of the patient, though
not markedly. An electrocardiogram revealed a low QRS voltage (limb
leading) and a poor R wave progression. A chest radiograph
demonstrated increased bronchovascular shadows, pachyntic pleurae
and an enlarged, pear-shaped heart. An abdominal color Doppler
ultrasonography scan revealed splenomegaly, pyoperitoneum and
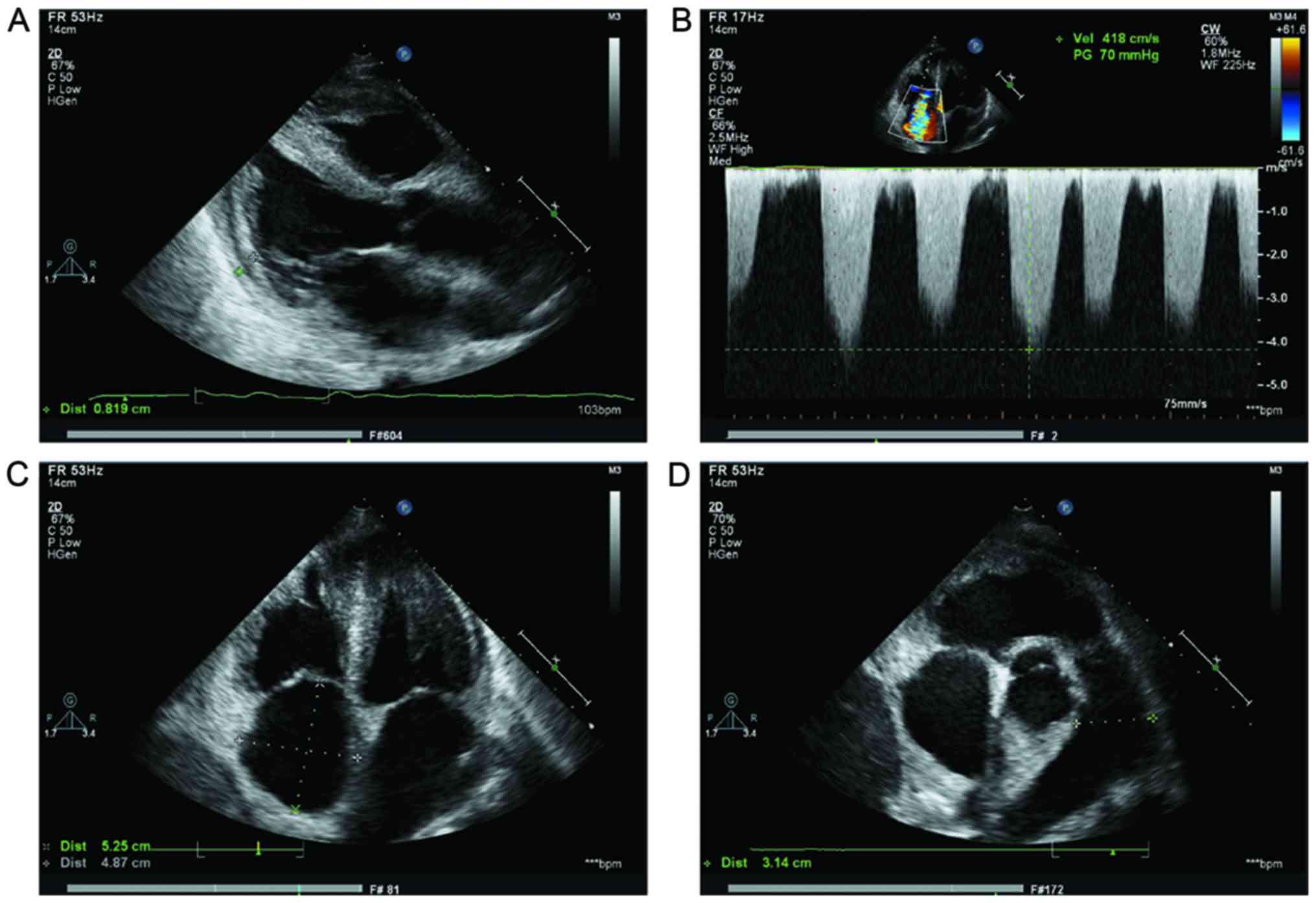
dropsy of the gallbladder wall. Echocardiographical analysis
revealed enlarged atria, a dilatate main pulmonary artery, moderate
mitral regurgitation, mild aortic regurgitation, severe tricuspid
regurgitation, mild pulmonary regurgitation and severe pulmonary
hypertension (Fig. 2). A computed
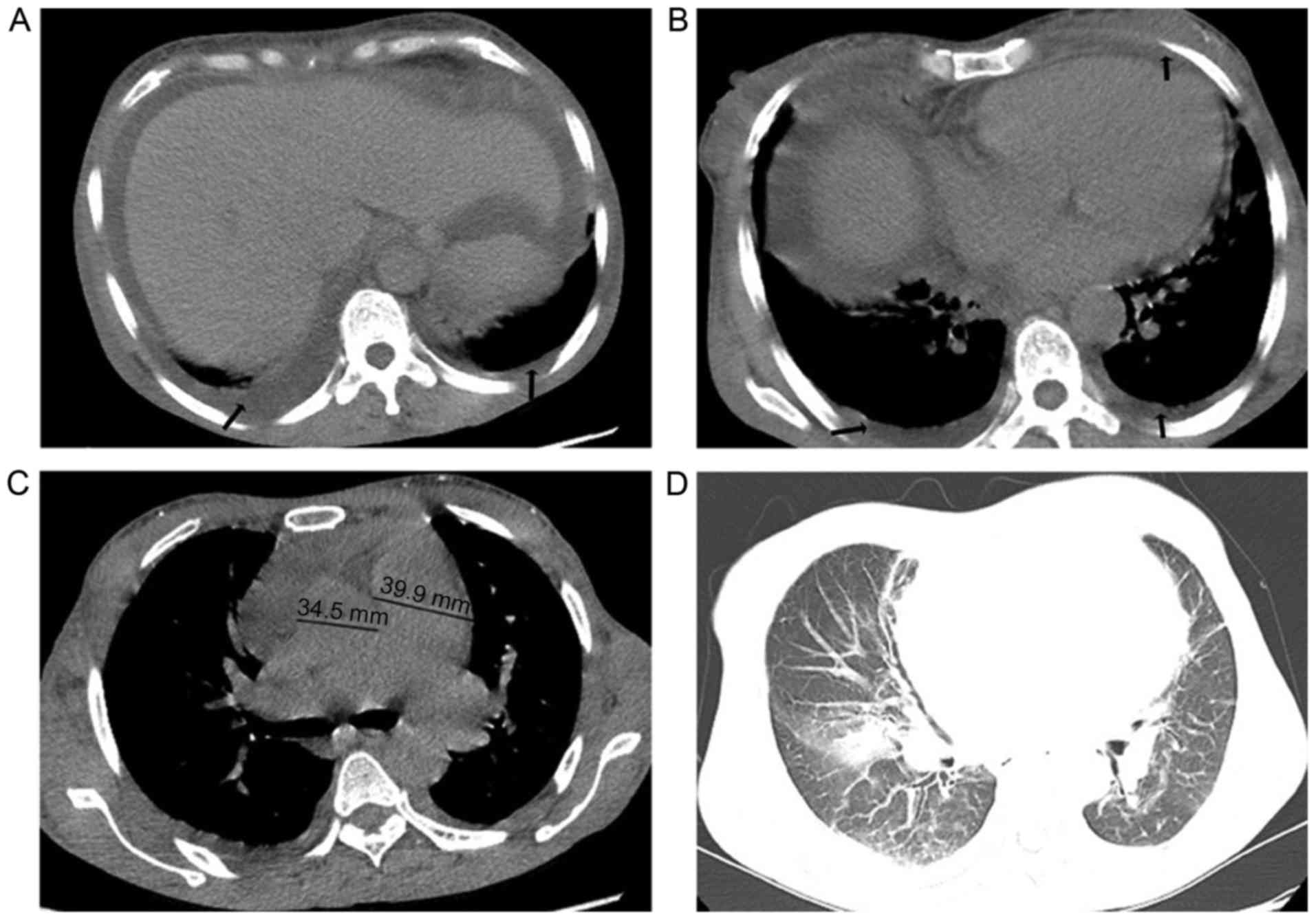
tomography scan demonstrated that the lungs of the patient
exhibited exudative alterations; scattered, and partial
interstitial inflammation a thickened pulmonary artery; pulmonary
hypertension; bilateral pleural; abdominal cavity and pericardial
effusion; thoracic-abdominal wall and mesenterium edema. The
patient also exhibited cholecystitis and multiple lymphadenopathy
at heraxilla. Representative ascites, pleural and pericardial
effusion and pulmonary edema were demonstrated in Fig. 3A pituitary gland magnetic resonance
imaging (MRI) plain scan revealed partially empty sella. Plain
computed tomography of lumbar vertebrae demonstrated a degenerative
lumbar spine (calcification and small bony outgrowths), and L3/4
and L5/S1diskal hernia. MRI revealed osteosclerotic and blastic
nodules and patches on the spine and pelvis.
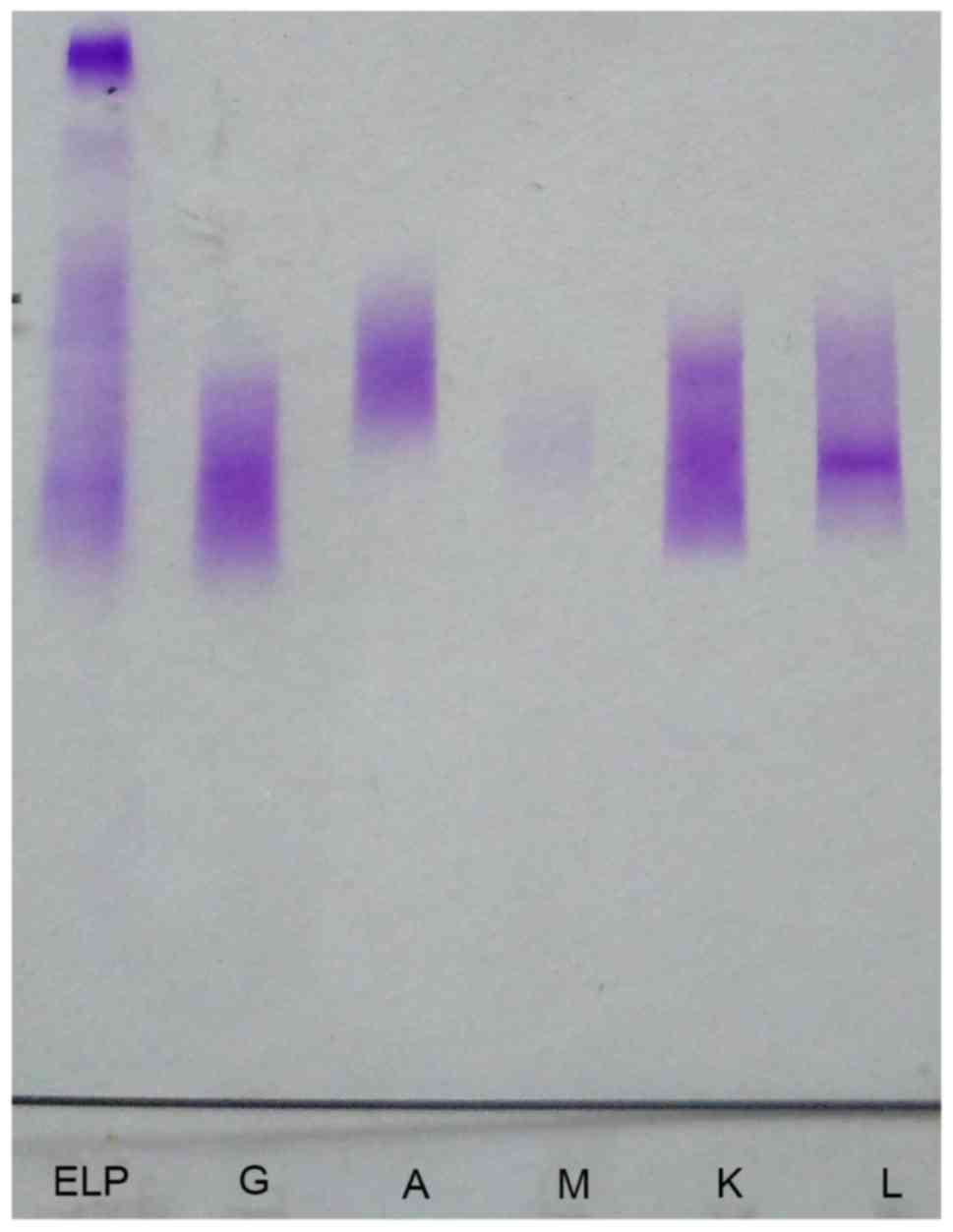
In contrast with the hypoalbuminemia, immunoglobulin
(Ig)G, and λ and κ light chains were increased. Immunofixation
electrophoresis was performed using the HYDRAGEL IF kit, according
to the manufacturer's protocol (cat. no. PN4301; Sebia, Evry,
France). The commercial HYDRAGEL IF (Sebia) was used, with a
HYDRASYS 2 automated electrophoresis system (Sebia). The serum was
diluted three times and the loading amount of each lane was 10 µl
and 2 repeats of serum protein electrophoresis with immunofixation
were performed. For immunofixation, antibodies were provided by the
HYDRAGEL commercial kit (cat. no. PN4301; Sebia) and were used as
purchased. All durations and temperatures of incubations for
electrophoresis with immunofixation were automated by HYDRASYS 2
(Sebia). The results of the present study demonstrated that γ
(IgG), κ and L were positive, but α (IgA), µ (IgM), δ (IgD) were
negative. The typical bands of protein electrophoresis are depicted
in Fig. 4. Serological tests for
tumor markers and rheumatism demonstrated negative results. Bone
marrow puncture revealed reactive bone marrow and the presence of
well-differentiated plasma cells.
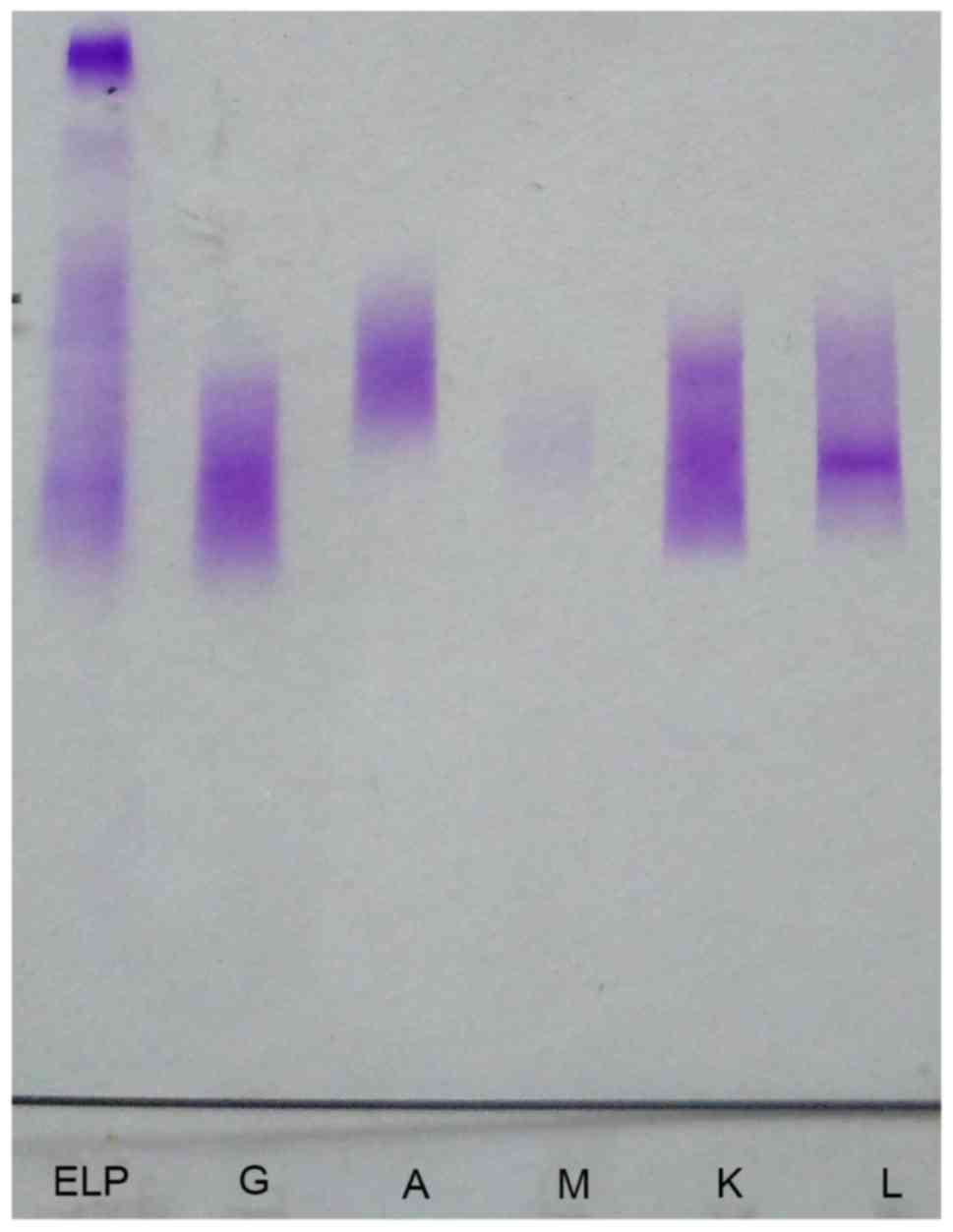 | Figure 4.Serum protein electrophoresis with
immunofixation revealed IgG, κ and L were positive, and that IgA
and IgM were negative. L, K, M, A, G and ELP represent λ light
chain, κ light chain, IgM, IgA, IgG and reference light protein,
respectively. Ig, immunoglobulin; ELP, elastin-like
polypeptide. |
POEMS syndrome was diagnosed using a combination of
history and examination results according to the 2014 update on
diagnosis, risk-stratification and management of POEMS syndrome
(18). The presence of polyneuropathy
(demyelinating in the majority of cases of POEMS syndrome);
monoclonal plasma cell disorder (typically λ-restricted in cases of
POEMS syndrome); sclerotic lesions on the spine and pelvis;
organomegaly, including hepatomegaly, splenomegaly and
lymphadenopathy; edema; pleural effusion; adrenal, thyroidal,
pituitary, gonadal and pancreatic endocrinopathy; skin alterations,
including hyperpigmentation, dry skin and hypertrichosis;
thrombocytosis; pulmonary hypertension; low vitamin B12
values; and weight loss supported the diagnosis of POEMS
syndrome.
Subsequently, the patient received a low-dose
steroid treatment (oral prednisolone 10 mg/day). However, when the
patient refused further positive medication, conservative treatment
was used to alleviate the pain and relieve symptoms. Respiratory
failure induced mortality in the patient 9 days following admission
to the hospital; the patient was aged 50.
Discussion
In 1980, Bardwick et al reported POEMS
syndrome for the first time (19).
Subsequently POEMS syndrome has been diagnosed based on a composite
of clinical and laboratory features (12), and is misdiagnosed in patients that
present with it if the syndrome is not considered. The pathogenesis
of the syndrome remains to be fully understood. Overproduction of
proinflammatory cytokines, including interleukin (IL)-1β, IL-6,
tumor necrosis factor-α, and VEGF, have been reported and may serve
important etiological functions (20–22). Of
these proinflammatory cytokines, only increased VEGF serves as a
major criterion for the diagnosis of POEMS syndrome (12). VEGF potentially causes effusions,
pulmonary hypertension and disseminated intravascular coagulation
(23,24), and is associated with POEMS syndrome
activity (25).
The diagnosis of POEMS syndrome depends on a
thorough history and a full examination of systems. The majority of
authors agree that the presence of two major and at least one minor
criteria are confirmatory (25). The
mandatory major criteria for POEMS syndrome is
polyradiculoneuropathy (typically demyelinating) and monoclonal
plasma cell disorder. The patient described by the present study
exhibited lumbodynia, pain and numbness all over the body, and the
EMG test revealed extensive motor and sensory polyneuropathy, with
typical demyelination at the proximal and distal ends of peripheral
nerves in all four limbs. Serum-protein electrophoresis detected
high levels of IgG, λ and κ light chains; serum immunofixation
demonstrated that IgG, κ and L were positive, and that IgA and IgM
were negative, which matched with the results demonstrated by
Dispenzieri et al (1).
However, analysis of the bone marrow of the patient revealed no
osteolytic lesions or plasma cell myeloma. MRI demonstrated a
degenerative lumbar spine, L3/4 and L5/S1 diskal hernia and
sclerotic bone lesion-associated osteosclerotic nodules on spine
and pelvis. VEGF is associated with POEMS syndrome activity
(24). However, since our hospital
(Qilu Hospital of Shandong University) was not able to detect serum
VEGF level, the present study did not determine the VEGF levels of
the patient. In addition, organomegaly in POEMS syndrome typically
occurs in the liver, spleen, and lymph nodes. The patient in the
present study presented with splenomegaly and lymphadenopathy of
bilateral axilla. Extravascular volume overload, including edema;
pleural, abdominal cavity and pericardial effusion and ascites
supported a diagnosis of POEMS syndrome. The presence of
autoantibodies against the thyroid gland, type 2 diabetes,
increased PRL and ACTH, decreasing TEST, and an empty sella turcica
were considered to be evidence of endocrinopathy. Hyperpigmentation
was the most common abnormality of skin alterations. A routine
blood test identified thrombocytosis. Weight loss, pulmonary
hypertension, thrombotic diatheses and low vitamin B12
levels also aided in the diagnosis of POEMS syndrome.
Currently, treatments for POEMS syndrome include
radiation, chemotherapy, bone marrow transplantation and the use of
other drugs, including alkylators, corticosteroids, bevacizumab,
rituximab, bortezomib, and thalidomide (26,27).
Surgical resection maybe a potential treatment in the event of
infection-associated complications, or the presence of a solitary
tumor (28). Although an anti-VEGF
strategy appears to be effective, limitations have been reported
(29). Due to financial limitations
and the severity of her condition, the patient in the present study
refused any further positive therapy, using only pain-alleviating
corticosteroids.
POEMS syndrome exhibits a chronic clinical course.
Follow-up data revealed that the median survival time of patients
is 165 months from the Mayo Clinic dysproteinmia database (1). A Chinese survey revealed that, 25 months
on from the initial diagnosis, 80% of patients were alive after 25
months and 10% of these patients survived >60 months (8). Cardiorespiratory failure, along with
pneumonia, was the most common means by which mortality occurred
(1). Respiratory failure induced
mortality in the patient described by the present study 24 months
following the initial onset of difficulty walking and numbness in
the lower limbs. The patient was aged 50.
POEMS syndrome is a rare paraneoplastic disorder
consisting of peripheral neuropathy, organomegaly, endocrinopathy,
and M protein and skin changes. The present study described a novel
case of POEMS syndrome associated with the inconspicuous symptom of
progressive weakness in the upper and lower limbs. The patient
first entered hospital with the same symptom 2 years prior to her
diagnosis. However, these symptoms were not identified as those of
POEMS syndrome. Therefore, the present study recommends that more
case reports concerning abnormal symptom-associated POEMS syndrome
should be considered to improve the future diagnosis and treatment
of POEMS syndrome, and enhance understanding of the syndrome.
Glossary
Abbreviations
Abbreviations:
|
VEGF
|
vascular endothelial growth factor
|
|
PRL
|
prolactin
|
|
ACTH
|
adrenocorticotropic hormone
|
|
TEST
|
testosterone
|
|
IgG
|
immunoglobulin G
|
|
EMG
|
electromyography
|
|
MRI
|
magnetic resonance tomography
|
|
IL
|
interleukin
|
References
|
1
|
Dispenzieri A, Kyle RA, Lacy MQ, Rajkumar
SV, Therneau TM, Larson DR, Greipp PR, Witzig TE, Basu R, Suarez
GA, et al: POEMS syndrome: Definitions and long-term outcome.
Blood. 101:2496–2506. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dispenzier A: POEMS syndrome: 2011 update
on diagnosis, risk-stratification and management. Am J Hematol.
86:592–601. 2011.
|
|
3
|
Sanada S, Ookawara S, Karube H, Shindo T,
Goto T, Nakamichi T, Saito M, Matsubara M and Suzuki M: Marked
recovery of severe renal lesions in POEMS syndrome with high-dose
melphalan therapy supported by autologous blood stem cell
transplantation. Am J Kidney Dis. 47:672–679. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakamoto Y, Imai H, Yasuda T, Wakui H and
Miura AB: A spectrum of clinicopathological features of nephropathy
associated with POEMS syndrome. Nephrol Dial Transplant.
14:2370–2378. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Watanabe O, Arimura K, Kitajima I, Osame M
and Maruyama I: Greatly raised vascular endothelial growth factor
(VEGF) in POEMS syndrome. Lancet. 347:7021996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Singh D, Wadhwa J, Kumar L, Raina V,
Agarwal A and Kochupillai V: POEMS syndrome: Experience with
fourteen cases. Leuk Lymphoma. 44:1749–1752. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Soubrier MJ, Dubost JJ and Sauvezie BJ:
POEMS syndrome: A study of 25 cases and a review of the literature.
French Study Group on POEMS syndrome. Am J Med. 97:543–553. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li J, Zhou DB, Huang Z, Jiao L, Duan MH,
Zhang W, Zhao YQ and Shen T: Clinical characteristics and long-term
outcome of patients with POEMS syndrome in China. Ann Hematol.
90:819–826. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kulkarni GB, Mahadevan A, Taly AB, Yasha
TC, Seshagiri KS, Nalini A, Satishchandra P, Veerendrakumar M and
Shankar SK: Clinicopathological profile of polyneuropathy,
organomegaly, endocrinopathy, M protein and skin changes (POEMS)
syndrome. J Clin Neurosci. 18:356–360. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Plata Bello J and Garcia-Marin V: POEMS
syndrome (polyneuropathy, organomegaly, endocrinopathy, multiple
myeloma and skin changes) with cranial vault plasmocytoma and the
role of surgery in its management: A case report. J Med Case Rep.
7:2452013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lee FY and Chiu HC: POEMS syndrome with
calciphylaxis: A case report. Acta Derm Venereol. 91:96–97. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dispenzieri A: POEMS syndrome: 2014 update
on diagnosis, risk-stratification, and management. Am J Hematol.
89:214–223. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nakamura Y, Nishimura M, Terano T,
McNamara KM, Sasano H, Kurosu A and Joh K: A patient with POEMS
syndrome: The pathology of glomerular microangiopathy. Tohoku J Exp
Med. 231:229–234. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kaya P, Alemdaroğlu I, Yilmaz Ö, Karaduman
A and Topaloğlu H: Effect of muscle weakness distribution on
balance in neuromuscular disease. Pediatr Int. 57:92–97. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Devine MS, Kiernan MC, Heggie S, McCombe
PA and Henderson RD: Study of motor asymmetry in ALS indicates an
effect of limb dominance on onset and spread of weakness and an
important role for upper motor neurons. Amyotroph Lateral Scler
Frontotemporal Degener. 15:481–487. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kuo DC, Bilal S and Koller P: Asymmetric
weakness and west nile virus infection. J Emerg Med. 49:274–276.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Iolascon G, de Sire A, Calafiore D,
Moretti A, Gimigliano R and Gimigliano F: Hypovitaminosis D is
associated with a reduction in upper and lower limb muscle strength
and physical performance in post-menopausal women: A retrospective
study. Aging Clin Exp Res. 27 Suppl 1:S23–S30. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dispenzieri A: POEMS Syndrome: 2014 update
on diagnosis, risk-stratification and management. Am J Hematol.
89:213–223. 2014. View Article : Google Scholar
|
|
19
|
Bardwick NJ, Zvaifler GN, Gill GN, Newman
D, Greenway G and Resnick DL: Plasma cell dyscrasia with
polyneuropathy, organomegaly, endocrinopathy, M protein, and skin
changes: The POEMS syndrome. Report on two cases and a review of
the literature. Medicine (Baltimore). 59:311–322. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rose C, Zandecki M, Copin MC, Gosset P,
Labalette M, Hatron PY, Jauberteau MO, Devulder B, Bauters F and
Facon T: POEMS syndrome: Report on six patients with unusual
clinical signs, elevated levels of cytokines, macrophage
involvement and chromosomal aberrations of bone marrow plasma
cells. Leukemia. 11:1318–1323. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hitoshi S, Suzuki K and Sakuta M: Elevated
serum interleukin-6 in POEMS syndrome reflects the activity of the
disease. Intern Med. 33:583–587. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Soubrier M, Sauron C, Souweine B, Larroche
C, Wechsler B, Guillevin L, Piette JC, Rousset H and Deteix P:
Growth factors and proinflammatory cytokines in the renal
involvement of POEMS syndrome. Am J Kidney Dis. 34:633–638. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tokashiki T, Hashiguchi T, Arimura K,
Eiraku N, Maruyama I and Osame M: Predictive value of serial
platelet count and VEGF determination for the management of DIC in
the Crow-Fukase (POEMS) syndrome. Intern Med. 42:1240–1243. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Niimi H, Arimura K, Jonosono M, Hashiguchi
T, Kawabata M, Osame M and Kitajima I: VEGF is causative for
pulmonary hypertension in a patient with Crow-Fukase (POEMS)
syndrome. Intern Med. 39:1101–1104. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dispenzieri A: How I treat POEMS syndrome.
Blood. 119:5650–5658. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kawano Y, Nakama T, Hata H, Kimura E,
Maruyoshi N, Uchino M and Mitsuya H: Successful treatment with
rituximab and thalidomide of POEMS syndrome associated with
Waldenstrom macroglobulinemia. J Neurol Sci. 297:101–104. 2012.
View Article : Google Scholar
|
|
27
|
Ohwada C, Nakaseko C, Sakai S, Takeda Y,
Abe D, Takeuchi M, Sakaida E, Masuda S, Shimizu N, Cho R, et al:
Successful combination treatment with bevacizumab, thalidomide and
autologous PBSC for severe POEMS syndrome. Bone Marrow Transplant.
43:739–740. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kotani Y, Ito M, Abumi K, Yasui K and
Minami A: Neurological recovery from pentaplegia after resection
for sacral plasmacytoma presenting with POEMS syndrome. J Neurosurg
Spine. 10:324–328. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Allam JS, Kennedy CC, Aksamit TR and
Dispenzieri A: Pulmonary manifestations in patients with POEMS
syndrome: A retrospective review of 137 patients. Chest.
133:969–974. 2008. View Article : Google Scholar : PubMed/NCBI
|