Introduction
Chemotherapy is the main treatment approach for
advanced gastric cancer and adjuvant post-operative gastric cancer;
however, multidrug resistance (MDR) often leads to the failure of
chemotherapy (1). MDR is a distinct
phenomenon enabling tumor cells to simultaneously develop
cross-resistance to multiple structurally dissimilar anticancer
drugs. Gastric cancer exhibits a strong MDR phenotype, resulting in
a response rate to chemotherapy of <50% (2). The 5-year survival rate in advanced
gastric cancer is 30%, which is possibly associated with the
development of MDR. Therefore, approaches to intervene and reverse
MDR in gastric cancer are required to improve the efficacy of
chemotherapy and the survival rate of patients with gastric
cancer.
Parthenolide (PN) is a sesquiterpene lactone
extracted from Feverfew (Tanacetum parthenium), and is
primarily used for the treatment of fever, arthritis and migraine
(3). Previous studies have
demonstrated that PN inhibits the growth and induces the apoptosis
of various tumor cell types in vitro (4–6). Evidence
suggests that PN induces anti-tumor effects primarily by targeting
nuclear factor-κB (NF-κB) (7),
producing reactive oxygen species (8)
and activating c-Jun N-terminal kinase (9). Furthermore, previous studies have
revealed that PN can enhance gastric, non-small cell lung and liver
cancer cell sensitivity to chemotherapy (10); however, the underlying mechanisms
remain unclear. In the present study, the effects and underlying
mechanisms of PN treatment on the sensitivity of drug-resistant
gastric cancer SGC-7901/DDP cells to cisplatin (DDP) were
investigated, in order to provide a theoretical basis for the
clinical application of PN.
Materials and methods
Reagents
The reagents and kits used in the present study were
purchased as follows: PN (Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany); DDP (Shandong Dezhou Taikang Pharmaceutical Co., Ltd.,
Dezhou, China); RPMI-1640 (Sigma-Aldrich; Merck KGaA); fetal bovine
serum (Hangzhou Evergreen Biological Engineering Materials Co.,
Ltd., Hangzhou, China); Annexin V-fluorescein isothiocyanate
(FITC)/propidium iodide (PI) detection kit (Nanjing KGI Biological
Technology Development Co., Ltd., Nanjing, China); MTT (Beijing
Solarbio Science & Technology Co., Ltd., Beijing, China);
enhanced chemiluminescence (ECL; GE Healthcare, Chicago, IL, USA);
and DAPI (Beyotime Institute of Biotechnology, Haimen, China). The
SGC-7901/DDP drug-resistant gastric cancer cell line was purchased
from Shanghai Bogoo Biotechnology Co., Ltd. (Shanghai, China). The
antibodies were obtained from the following: Goat anti-rabbit and
anti-mouse immunoglobulin G secondary antibodies (GE Healthcare
Life Sciences, Chalfont, UK); primary antibodies directed against
phosphorylated-signal transducer and activator of transcription 3
(p-STAT3), apoptosis regulator Bcl-xL and Bcl-2 (Santa Cruz
Biotechnology, Inc., Dallas, TX, USA); β-actin (Sigma-Aldrich;
Merck KGaA); and apoptosis regulator BAX (Bax), caspase-3, cleaved
caspase-3, cellular tumor antigen p53, caspase-9, cleaved
caspase-9, cyclin-dependent kinase inhibitor 1 (p21), cyclin D1 and
STAT3 (Wanleibio Biotechnology Co., Ltd., Shanghai, China).
Antibodies are detailed in Table
I.
 | Table I.Antibodies. |
Table I.
Antibodies.
| Antibody target | Supplier | Catalog no. | Dilution |
|---|
| p-STAT3 | Santa Cruz
Biotechnology, Inc., Dallas, TX, USA | Sc-293059 | 1:100 |
| Bcl-xL, | Santa Cruz
Biotechnology, Inc. | Sc-7195 | 1:300 |
| Bcl-2 | Santa Cruz
Biotechnology, Inc. | Sc-509 | 1:300 |
| β-actin | Sigma-Aldrich;
Merck KGaA, Darmstadt, Germany | SAB2100037 | 1:300 |
Instruments
General electrophoresis, horizontal and vertical
electrophoresis tank, and semi-dry transfer blotter were purchased
from Bio-Rad Laboratories, Inc., (Hercules, CA, USA). The Ti-U
manual fluorescence/inverted phase contrast microscope was obtained
from Nikon Corporation (Tokyo, Japan); BioSpectrum®
Imaging system from UVP Inc., (Upland, CA, USA); microplate reader
from Tecan Group Ltd. (Männedorf, Switzerland); and Alpha Automatic
Image Analysis system from Bio-Techne (ProteinSimple; Minneapolis,
MN, USA).
Cell culture
The human gastric cancer drug-resistant SGC-7901/DDP
cell line was cultured in RPMI-1640 supplemented with 10% fetal
bovine serum at 37°C with 5% CO2.
MTT assay
MTT was used to measure the effect of PN treatment
on SGC-7901/DDP cell proliferation and sensitivity to DDP.
SGC-7901/DDP cells in the exponential growth phase were harvested
and made into single cell suspensions at a concentration of
5×104 cells/ml. The cells were seeded in 96-well plates
(100 µl/well) and incubated for 24 h at 37°C. The SGC-7901/DDP
cells were treated with various concentrations of PN (0, 2.5, 5,
10, 12.5 and 15 µmol/l) and DDP (0, 1.25, 2.5, 5, 10 and 15 µg/ml)
with five-replicates/concentration. A total of 20 µl of 5 g/l MTT
solution was added to each well at 24, 48 and 72 h, and then
incubated for 4 h at 37°C. The supernatant was discarded and 150 µl
dimethyl sulfoxide was added to each well. The plates were
oscillated at a low speed for 2 min at room temperature (23–25°C)
until all crystals were fully dissolved. The absorbance of each
well was measured at a wavelength of 490 nm using a
spectrophotometer. The growth inhibitory rate (%) was calculated
using the following formula: (1-(absorbance of experimental
well/absorbance of blank)) ×100%.
In order to prevent excessive cell death, based on
the results from the above experiments, the combinations of less
toxic concentrations of PN (5 and 10 µmol/l) and DDP (1.25 and 2.5
µg/ml) were selected. Therefore, the SGC-7901/DDP cells were
treated with the following combinations: 5 µmol/l PN+1.25 µg/ml
DDP; 5 µmol/l PN+2.5 µg/ml DDP; 10 µmol/l PN+1.25 µg/ml DDP; or 10
µmol/l PN+2.5 µg/ml DDP. The MTT assay was performed at 24 h
following the treatments. The Zhenjun Jin method (11) was used to determine the synergy
q=E(AB)/(EA+EB-EA × EB) EAB refers to growth inhibitory rate of
combined treatment; and EA and EB refer to the growth inhibitory
rate with either A or B treatment. q<0.85 indicates mutual
antagonism of two drugs; q=0.85–1.15 indicates a simple additive
effect of the two drugs; q>1.15 indicates that the two drugs
have a synergistic effect.
Cell cycle distribution analysis via
flow cytometry
SGC-7901/DDP cells in the exponential growth phase
were seeded in 6-cm petri dishes at a density of 5×105
cells/dish. The medium was changed 12 h following seeding and the
cells were treated with 0, 7.5 or 15 µmol/l of PN for 48 h at 37°C.
The supernatant was discarded and the cells were digested with
EDTA-free trypsin, washed twice with PBS, and fixed with 70%
ethanol at −20°C overnight. Cell were washed twice with PBS,
treated with RNaseA (a final concentration of 250 µg/ml) and
incubated in a 37°C water bath for 30 min. The cells were stained
with 5 µl PI in a dark room for 50 min at room temperature, and
then the cell cycle distribution was measured using a FACSCalibur
flow cytometer and FlowJo 7.6.1 (BD Biosciences, Franklin Lakes,
NJ, USA).
Cell apoptosis detection via flow
cytometry
SGC-7901/DDP cells in the exponential growth phase
were seeded in 6-cm petri dishes at a density of 5×105
cells/dish. After culturing for 12 h, cells were treated with 0,
7.5, or 15 µmol/l PN for 48 h at 37°C. Cells were digested with
EDTA-free trypsin, washed twice with PBS, stained for 15 min at
room temperature in the dark using the Annexin V-FITC Apoptosis
Detection kit and then the apoptosis rate was detected.
Cell apoptosis was detected by DAPI
staining
SGC-7901/DDP cells in the exponential growth phase
were seeded in 24-well culture plates at a density of
5×104 cells/well, and cultured for 24 h at 37°C. Cells
were treated with 0, 7.5, or 15 µmol/l of PN for 24 h at 37°C.
Cells were fixed with 0.1% paraformaldehyde for 30 min, washed with
PBS for 5 min and stained with DAPI for 10 min at room temperature
(23–25°C). The cells were observed using a fluorescence microscope
(magnification, ×100) at an excitation wavelength of 359 nm.
Western blotting
SGC-7901/DDP cells in the exponential growth phase
were seeded in 10 cm dishes at a density of 5×105
cells/ml and cultured for 24 h at 37°C. Cells were treated with
different concentrations of PN (final concentration of 0, 7.5 or 15
µmol/l) and collected 48 h after treatment. The total protein was
extracted using radioimmunoprecipitation assay buffer (P0013J;
Beyotime Institute of Biotechnology) and phenylmethanesulfonyl
fluoride (ST506; Beyotime Institute of Biotechnology). The protein
quantity was determined using a bicinchoninic acid assay kit
(P0011; Beyotime Institute of Biotechnology). Protein samples were
boiled at 100°C for 5 min. A total of 30 µg protein/lane was loaded
and subjected to SDS-PAGE (10% gel). The proteins were transferred
to polyvinylidene difluoride membranes, blocked with 0.5% skim milk
for 1 h (23–25°C) and incubated with the appropriate primary
antibody at 4°C overnight. The membranes were washed with TBS-Tween
20 three times (5 min/wash) and then incubated with the
corresponding secondary antibody at room temperature for 2 h. The
membranes were washed with TBST and detected using an ECL
luminescent liquid with cytometry. The quantitative analysis was
performed with ImageJ software (version 1.45; National Institutes
of Health, Bethesda, MD, USA. The relative expression of the target
protein was calculated as the ratio of grey values of the target
protein to the β-actin internal control.
Scratch migration assay
SGC-7901/DDP cells in the exponential growth phase
were seeded in 6-well plates at a density of 5×105
cells/well and cultured until 70% confluence was achieved. A
scratch was made in each well using a 100-µl pipette tip. The cells
were treated with various concentrations of serum-free PN (0, 2.5
or 5 µmol/l). Images were acquired at 24, 48 and 72 h after
treatment. The scratch width was measured and the mobility was
calculated as follows: (Distance/scratch width) ×100%.
Transwell cell invasion assay
In order to assess the invasive ability of cells,
120 µg Matrigel was added to a Transwell chamber. The gel was
diluted with two volumes of serum-free RPMI-1640 and incubated at
37°C for 30 min until the gel solidified. RPMI-1640 containing 10%
FBS was added to the lower chamber as a chemoattractant.
SGC-7901/DDP cells in the exponential growth phase were digested
with EDTA-free trypsin and viable cell counts were performed by
eye. A 200-µl suspension containing 5×104 cells was
added to each Transwell chamber and cultured for 48 h at 37°C. The
experiment was performed in triplicate. The liquid in the upper
chamber was discarded. The non-invasive cells and Matrigel on the
membrane surface were removed using a wet cotton swab. The membrane
was rinsed with saline, slightly dried, fixed in formalin (4%) for
15 min and stained with crystal violet for 12 min (23–25°C). The
penetrating cell count was performed in three different fields at a
magnification of ×100 using a light microscope.
Statistical analysis
Data are presented as the mean ± standard deviation.
Statistical analysis was performed using SPSS (version 10.0; SPSS,
Inc., Chicago, IL, USA) using one-way analysis of variance.
Comparisons between groups were measured using the post-hoc test.
Multiple comparisons amongst groups were performed using the
Student-Newman-Keuls test. P<0.05 was considered to indicate a
statistically significant difference.
Results
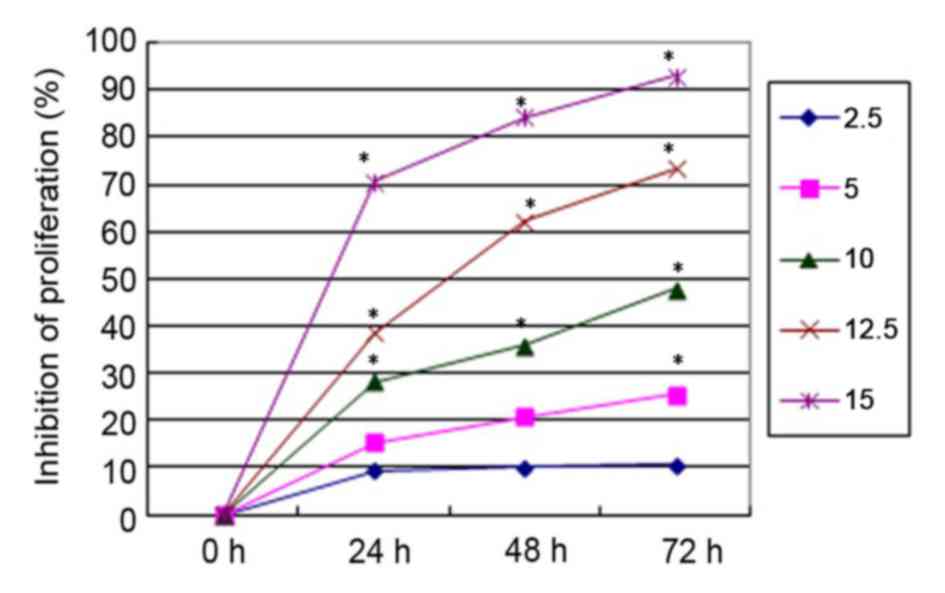
Cell proliferation inhibitory effects
of PN and the changes in the sensitivity of SGC-7901/DDP to
DDP
All concentrations of PN, except 2.5 µmol/l,
significantly inhibited SGC-7901/DDP cell proliferation in a time-
and concentration-dependent manner compared with untreated cells
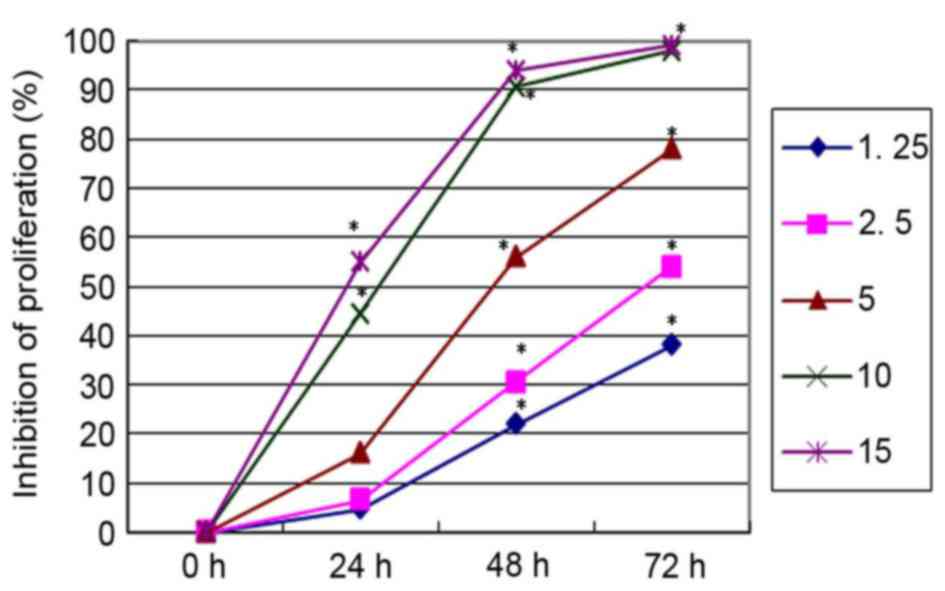
(Fig. 1). DDP inhibited SGC-7901/DDP
cell proliferation in a similar time- and concentration-dependent
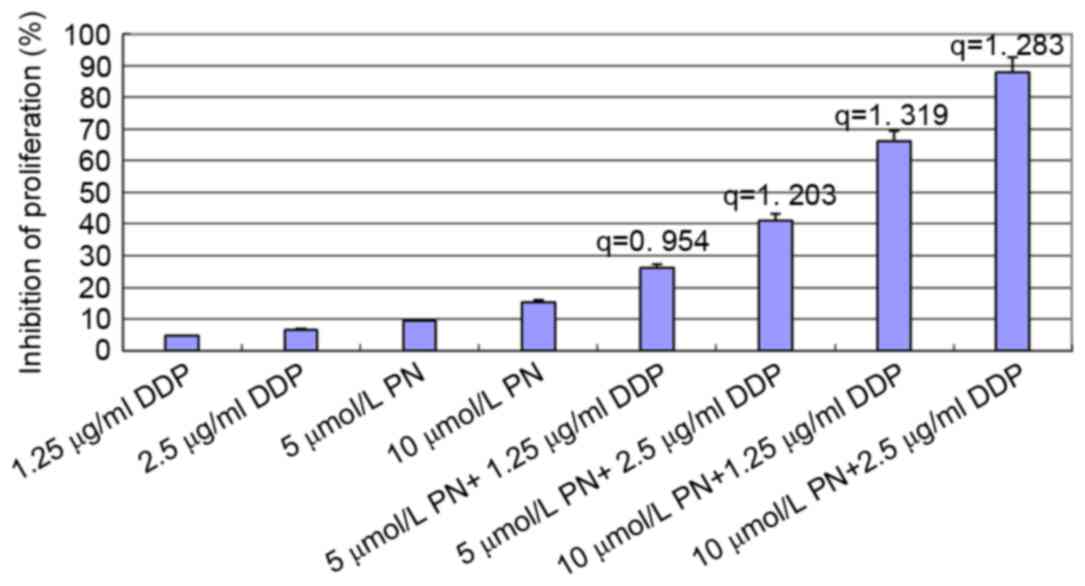
manner (Fig. 2). To investigate the
changes in the sensitivity of SGC-7901/DDP cells to the DDP,
SGC-7901/DDP cells were treated with combinations of PN and DDP as
described above. The rate of proliferation inhibition in each group
is presented in Fig. 3. The q value
for each group was calculated using the Zhenjun Jin method. With
the exception of the minimal concentration group (5 µmol/l PN+1.25
µg/ml DDP), the q values for all other groups were >1.15,
indicating that the two drugs have a synergistic effect.
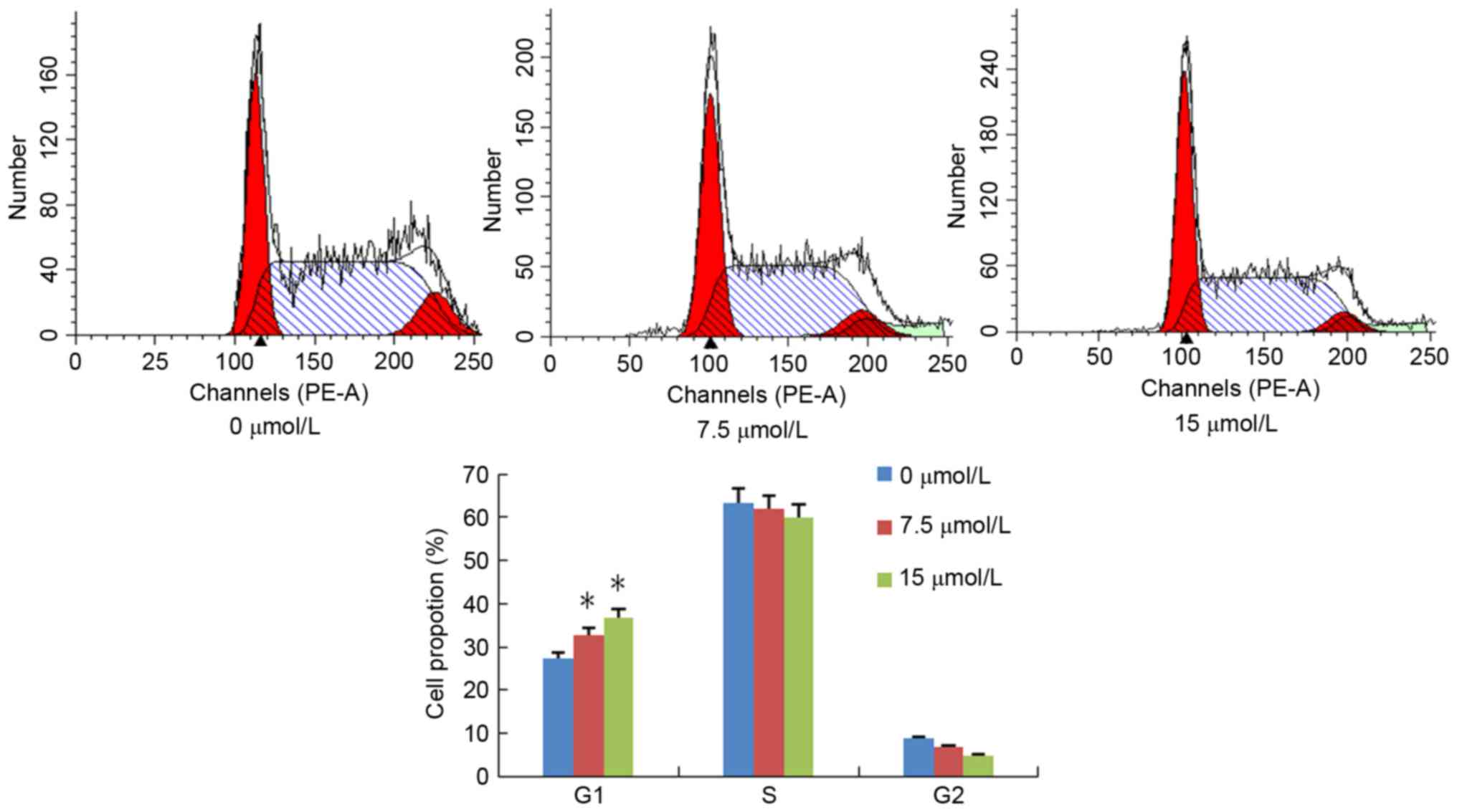
PN induces cell cycle arrest in
SGC-7901/DDP cells
SGC-7901/DDP cells were treated with different
concentrations of PN (0, 7.5 or 15 µmol/l) and the cell cycle
distribution was analyzed 48 h following treatment (Fig. 4). The ratio of
G0/G1 in the untreated and 7.5, and 15 µmol/l
PN groups was 27.2±1.05, 32.7±1.50 and 35.8±1.39%, respectively;
the percentage of S-phase cells was 63.98±2.74, 60.49±2.11, and
58.94±3.10%, respectively. Furthermore, the percentage of
G2/M phase cells was 8.82±0.57, 6.78±0.73 and
4.72±0.46%, respectively. Compared with the untreated control
group, the population of S and G2/M phase cells in the
treatment groups significantly decreased but not significantly, and
G1 phase cells significantly increased in a
concentration-dependent manner (P<0.05; Fig. 4).
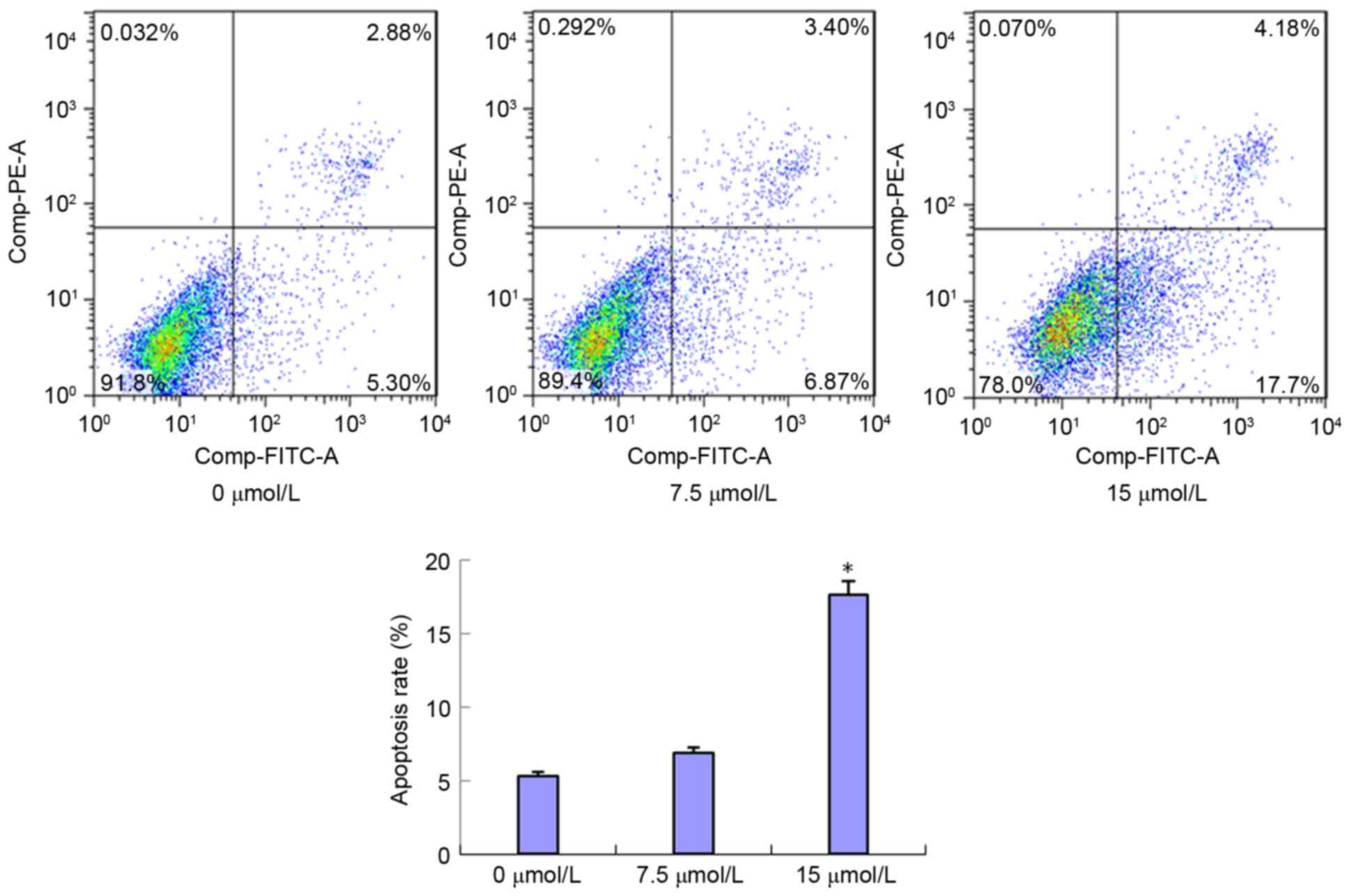
PN induces SGC-7901/DDP cell
apoptosis
SGC-7901/DDP cells were treated with 7.5 and 15
µmol/l of PN and the cell apoptosis rates were detected 48 h
following treatment (Fig. 5). The
early apoptosis rates in the 7.5 and 15 µmol/l treated groups were
6.87±0.63 and 17.7±1.15%, respectively. Compared with the control
group (5.30±1.31%), the early apoptosis rate was markedly increased
in the 7.5 µmol/l group and significantly increased in the 15
µmol/l group (P<0.05) compared with that in the untreated
control group. The late apoptosis rates were 2.88±0.54, 3.4±0.61
and 4.18±0.78% following no treatment, and treatment with 7.5 and
15 µmol/l PN, respectively. No statistically significant
differences were identified between these groups (data not
shown).
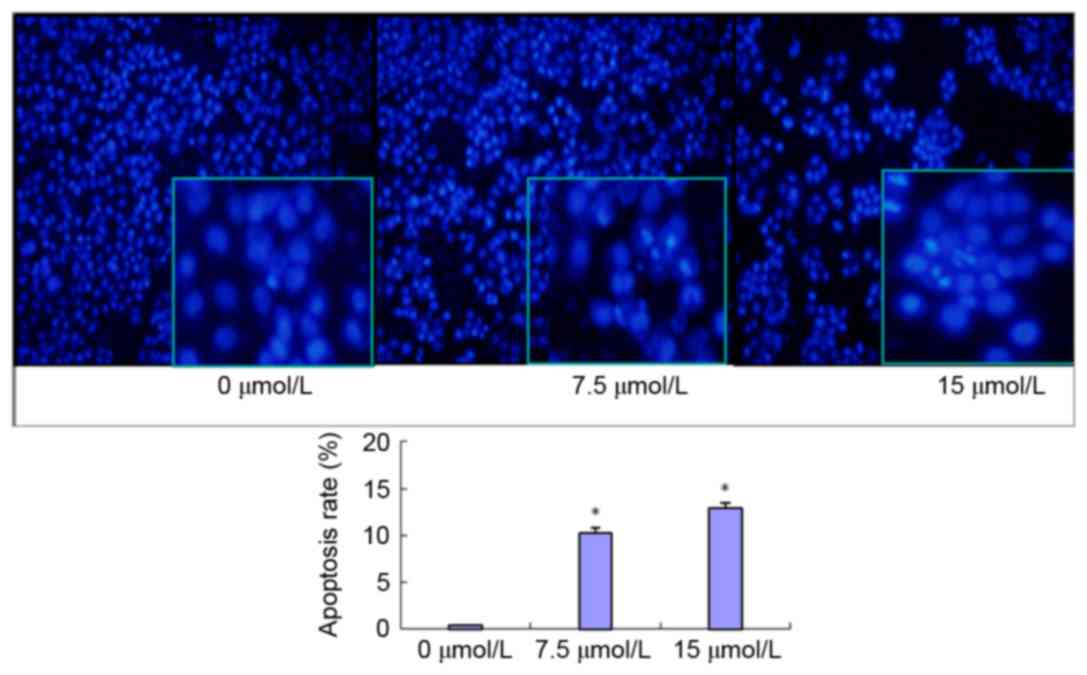
PN induces SGC-7901/DDP cell apoptosis
as determined using DAPI staining
SGC-7901/DDP cells were treated with 7.5 or 15
µmol/l PN and observed using DAPI staining after 24 h (Fig. 6). The cells in the untreated control
group possessed normally shaped nuclei (round or oval) with uniform
staining and evenly distributed nuclear chromatin. The shrinkage,
cohesion and fragmentation (spherical or particulate matter) of
nuclei were observed 48 h after PN treatment. The number of
apoptotic cells increased in a PN concentration-dependent manner,
as indicated by the number of dense fluorescent particles (Fig. 6). The SGC-7901/DDP cell apoptosis
rates were 0.88±0.05, 10.56±0.82 and 18.85±1.13% in the untreated,
7.5, and 15 µmol/l PN groups, respectively. The increases in
apoptosis rates in the 7.5 and 15 µmol/l groups were significant
compared with the untreated control group (P<0.05; Fig. 6).
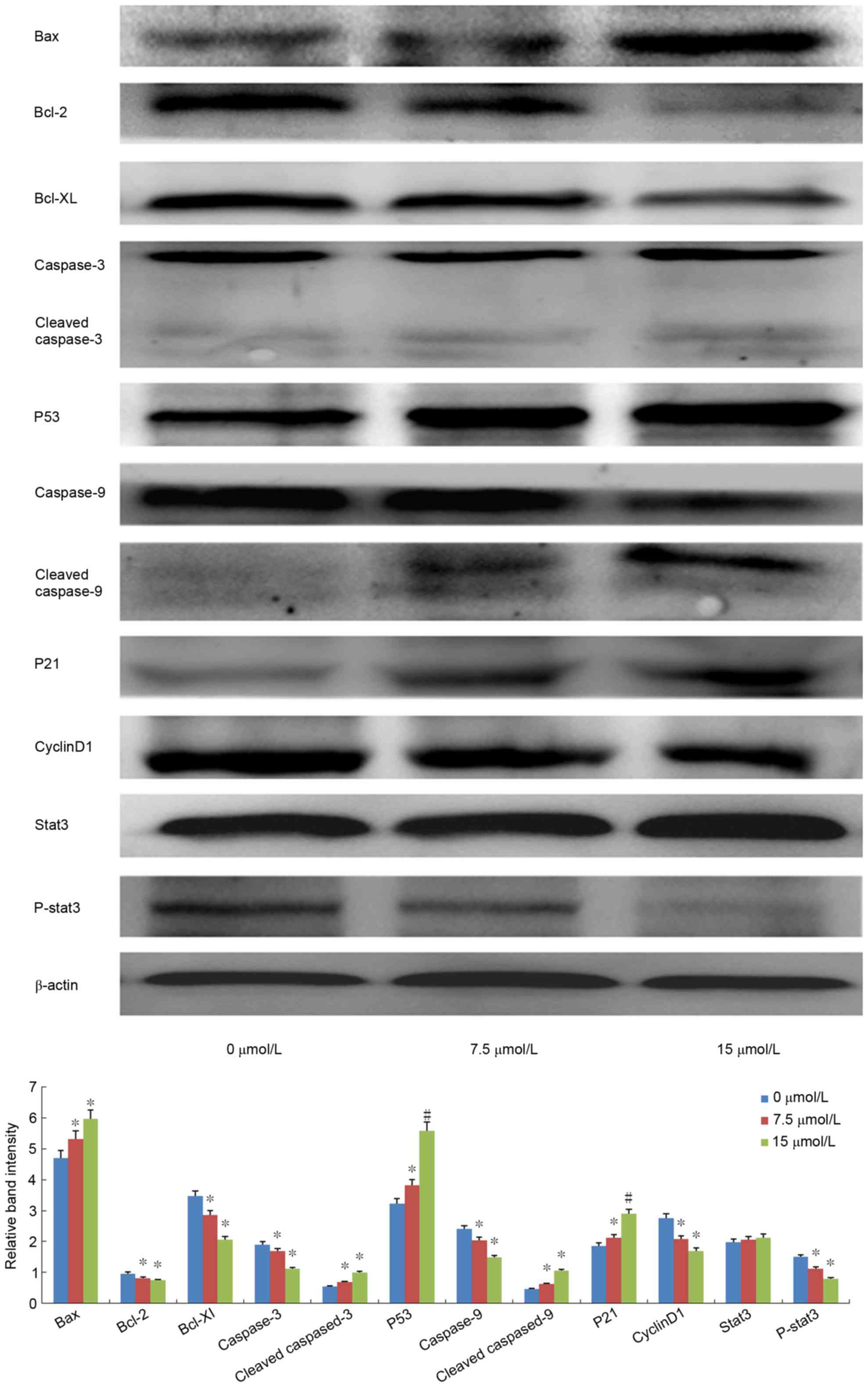
Expression of apoptosis- and cell
cycle-associated proteins
Among the apoptosis-associated proteins, following
PN treatment (7.5 or 15 µmol/l) Bax and p53 expression was
significantly upregulated, Bcl-xL and Bcl-2 was significantly
downregulated, and cleaved caspase-3 and −9 was significantly
increased in a dose-dependent manner as compared with the
expression in the untreated control groups (all P<0.05; Fig. 7). Among the cell cycle-associated
proteins, cyclin D1 expression was significantly decreased, p21 was
significantly increased, and P-STAT3 activation was significantly
inhibited (all P<0.05; Fig.
7).
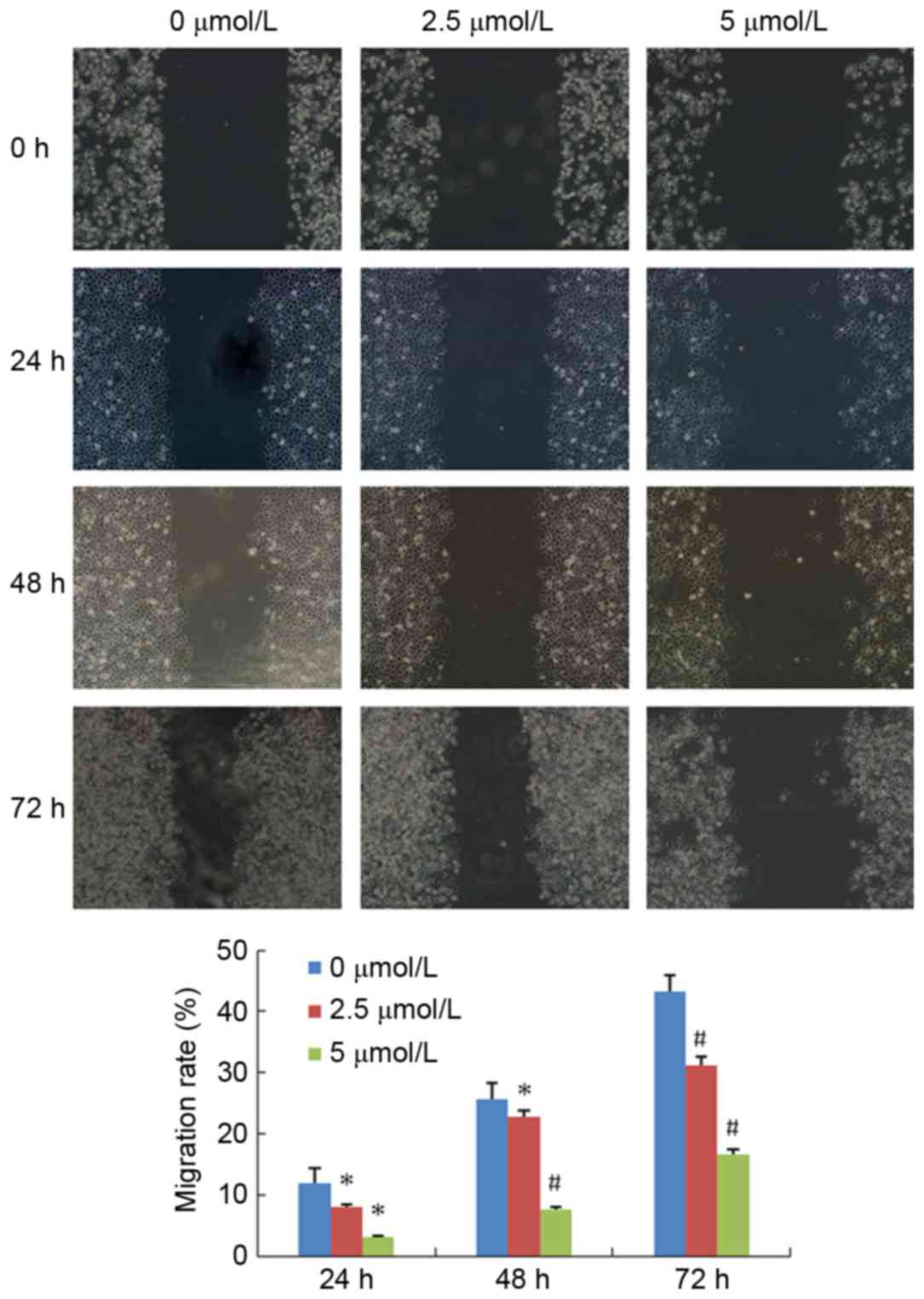
PN decreases SGC-7901/DDP cell
migration
The effect of PN on SGC-7901/DDP cell migration is
presented in Fig. 8. The mobility
rate of the untreated control group at 24, 48 and 72 h were
11.85±2.55, 25.57±2.75, and 43.32±2.52%, respectively. The mobility
rate of the 2.5 µmol/l PN group at 24, 48 and 72 h were 8.09±0.83,
22.70±2.92, and 31.11±3.85%, respectively. The mobility rate of the
5 µmol/l PN group at 24, 48 and 72h were 3.13±0.76, 7.62±1.17, and
16.54±3.02%, respectively. The differences between the 2.5 and 5
µmol/l PN groups, and the untreated control group at each time
point were statistically significant (P<0.05).
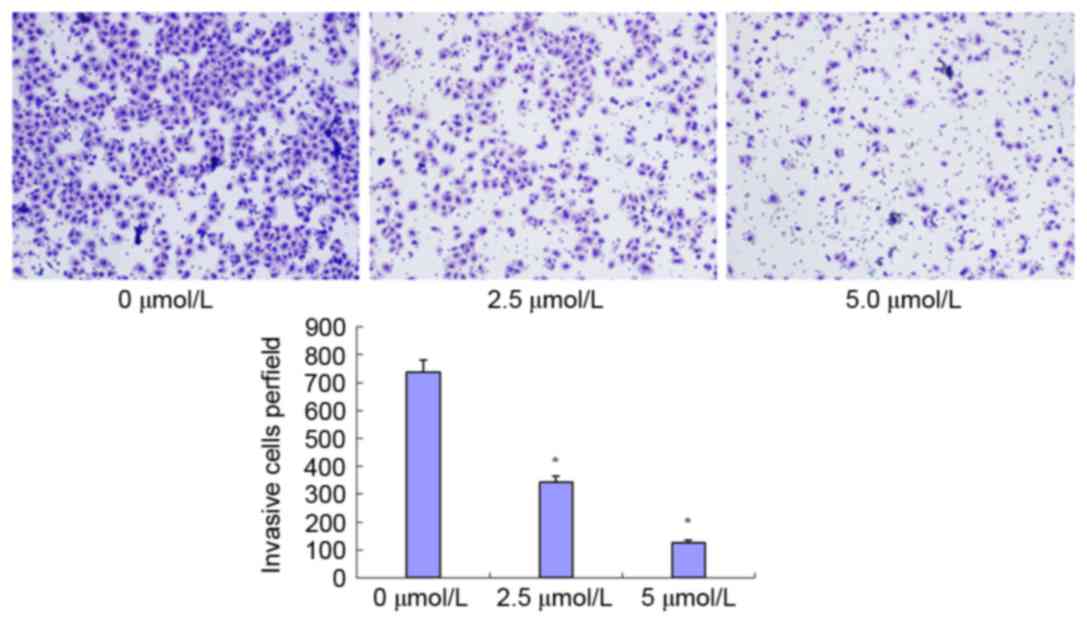
PN decreases SGC-7901/DDP cell
invasion ability
The effect of PN on invasion ability is presented in
Fig. 9. The number of transmembrane
cells in the untreated control, and 2.5 and 5 µmol/l PN groups were
737±33.57, 344±12.81, and 127±8.02, respectively. The differences
between the treated groups and the untreated control group were
statistically significant (P<0.05).
Discussion
Previous studies have demonstrated that PN can
inhibit the proliferation of tumor cells and enhance the
sensitivity of certain cancer cell lines to anti-cancer drugs
(7,12). Gao et al (13) suggested that PN enhances the
sensitivity of non-small cell lung cancer cells to chemotherapy
drugs via modulation of the NF-κB/I-κB kinase (IKK) signal cascade
through IKKβ. Furthermore, Liu et al (14) and another study (15) revealed that PN is able to enhance the
sensitivity of drug-resistant hepatocellular carcinoma cells to
chemotherapy drugs through inhibition of NF-κB activity, the
downregulation of P-glycoprotein, multidrug resistance-associated
protein, Bcl-2 and proto-oncogene Wnt family member 1 expression
levels, and the upregulation of p53 expression. The present study
demonstrated that PN significantly inhibited the proliferation of
the drug-resistant gastric cancer cell line SGC7901/DDP in a time-
and concentration-dependent manner. Additionally, PN and DDP
co-treatment demonstrated a synergistic effect. The inhibitory
effect of PN on SGC7901/DDP cell proliferation may be due to cycle
arrest and the induction of apoptosis. PN treatment was
demonstrated to induce early phase apoptosis and G1
phase cycle arrest. Furthermore, the results in the present study
revealed that the anticancer effects of PN are associated with the
upregulation of p53 and Bax, the downregulation of Bcl-2 and
Bcl-xL, and the activation of capase-9 and caspase-3. Previously,
these proteins have all been demonstrated to be involved in the
regulation of apoptosis (12,16), thus these results suggest that PN
treatment activates the apoptotic signaling pathway. In addition,
the results of the current study revealed that PN significantly
decreased cyclin D1, increased p21 expression and inhibited STAT3
activation.
STAT3 in the cytoplasm is a bifunctional protein.
Previous studies (17,18) have revealed that the STAT3 downstream
target genes, including Bcl-xL, Bcl-2, induced myeloid leukemia
cell differentiation protein Mcl-1, cyclin D1, proto-oncogene
c-Myc, Jun proto-oncogene AP-1 transcription factor subunit, Fas
cell surface death receptor and vascular endothelial growth factor,
which are closely associated with cell proliferation, apoptosis,
and angiogenesis. Under normal physiological conditions, the
activation of STATs is rapid and transient. Sustained activation of
this signaling pathway in tumor cells can induce the upregulation
of cell cycle regulatory factors and anti-apoptotic proteins,
consequently promoting abnormal proliferation, and migration of
malignant tumors (19). Therefore,
STAT3 is considered an oncogene (19). Previous studies demonstrated that
STAT3 signaling pathway may be associated with tumor cell
drug-resistance to chemotherapy (20,21). The
aberrant activation of STAT3 can aid in the evasion of cancer cell
death caused by drugs, thus inducing drug resistance. The
inhibition of the STAT3 signaling pathway may become a potential
cancer therapeutic target in the future. For example, Yue et
al (22) demonstrated that the
overactivation of STAT3 promotes DDP-resistant ovarian cancer
progression, and can be used as a gene marker for drug resistance
and cancer recurrence. Ovarian cancer cells with high expression
levels of STAT3 and Bcl-xL exhibit DDP, and Taxol resistance;
whereas, low STAT3 expression cell lines are sensitive to the drug
treatment (23). Inhibiting the STAT3
signaling pathway can promote apoptosis of drug-resistance cancer
cells and increase the sensitivity of cancer cells to various drugs
(23). In addition, a previous study
demonstrated that STAT3 activation-induced expression of Bcl-xL can
enhance the survival and drug resistance capability of human tumor
cells; and that silencing of the STAT3 gene downregulates the
expression of Bcl-xL (24). In
addition, inhibition of Bcl-xL protein expression through siRNA
knockdown in the gastric cancer MGC-803 cell line promotes
programmed cell death (24).
STAT3 overactivation has been identified in various
types of tumor cells, including breast and ovarian cancer, and head
and neck squamous cell carcinoma (25,26). In
addition, Yu et al (27)
demonstrated that the activity of STAT3 in gastric cancer cell
lines is higher compared with that in normal gastric epithelial
cells. STAT3-DNA binding activity is higher in poorly
differentiated gastric adenocarcinoma cell lines (SGC7901, MKN45
and AGS) compared with in highly differentiated gastric cancer cell
lines (MKN28 and NCI-SNU-1) (27).
Furthermore, p-STAT3 expression in poorly differentiated gastric
cancer tissue is higher compared with in the adjacent normal
mucosa, suggesting that the overactivation of STAT3 serves a role
in gastric cancer (27).
The results of the present study revealed that PN
significantly inhibited STAT3 phosphorylation, modulated the
expression levels of the downstream cell cycle-associated proteins,
including cyclin D1 and p21, and downregulated the
apoptosis-associated protein expression, including Bcl-2 and
Bcl-XL. Cyclin D1 is an essential protein in the regulation of the
cell cycle G1 phase. p21 is an important member of the
cell cycle protein kinase inhibitor gene family. Decreased cyclin
D1 and increased p21 expression results in increased cell cycle
arrest at the G1 phase. Bcl-2 and Bcl-xL are important
members of the anti-apoptotic protein family. Bcl-2 and Bcl-XL
downregulation can enhance tumor cell susceptibility to
drug-induced apoptosis. Song et al (28) revealed that PN inhibits the activation
of STAT3 signaling pathway; Carlisi et al (29) also demonstrated that PN significantly
reduces STAT3 and STAT5 phosphorylation, and increases the
sensitivity of liver cells to apoptosis. Cheng et al and
Ghantous et al (30–32) also confirmed that the anti-tumor
effects of PN are not only due to the inhibition of NF-κB, but also
associated with p21 upregulation, and the downregulation of cyclin
D1 and Bcl-xL. The results of the current study are consistent with
these previous studies. However, STAT3 converges various
carcinogenic kinase signaling pathways, including the epidermal
growth factor, interleukin-6/Janus kinase and Src signaling
pathways. The mechanisms underlying the interactions of PN with the
upstream and downstream factors in these complex signaling pathways
warrants further investigation. In addition, the present study
revealed that PN can inhibit SGC7901/DDP cell migration and
invasion. These results suggest that PN is a promising anticancer
drug for the treatment of patients with gastric cancer.
Acknowledgements
The present study was supported by the Natural
Science Foundation of Liaoning Province Funded Project (grant no.
2013022070) and the Liaoning Medical Youth Science and Technology
Start-up Funding Project (grant no. Y2012Z004).
References
|
1
|
Fodale V, Pierobon M, Liotta L and
Petricoin E: Mechanism of cell adaptation: When and how do cancer
cells develop chemoresistance? Cancer J. 17:89–95. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shi H, Lu D, Shu Y, Shi W, Lu S and Wang
K: Expression of multidrug resistance-related proteins
p-glycoprotein, glutathione-s-transferases, topoisomerase-II and
lung resistance protein in primary gastric cardiac adenocarcinoma.
Hepatogastroenterology. 55:1530–1536. 2008.PubMed/NCBI
|
|
3
|
Kishida Y, Yoshikawa H and Myoui A:
Parthenolide, a natural inhibitor of nuclear factor-kappaB,
inhibits lung colonization of murine osteosarcoma cells. Clin
Cancer Res. 13:59–67. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kawasaki BT, Hurt EM, Kalathur M, Duhagon
MA, Milner JA, Kim YS and Farrar WL: Effects of the sesquiterpene
lactone parthenolide on prostate tumor-initiating cells: An
integrated molecular profiling approach. Prostate. 69:827–837.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liu JW, Cai MX, Xin Y, Wu QS, Ma J, Yang
P, Xie HY and Huang DS: Parthenolide induces proliferation
inhibition and apoptosis of pancreatic cancer cells in vitro. J Exp
Clin Cancer Res. 29:1082010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang W, Adachi M, Kawamura R, Sakamoto H,
Hayashi T, Ishida T, Imai K and Shinomura Y: Parthenolide-induced
apoptosis in multiple myeloma cells involves reactive oxygen
species generation and cell sensitivity depends on catalase
activity. Apoptosis. 11:2225–2235. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dai Y, Guzman ML, Chen S, Wang L, Yeung
SK, Pei XY, Dent P, Jordan CT and Grant S: The NF (Nuclear
factor)-κB inhibitor parthenolide interacts with histone
deacetylase inhibitors to induce MKK7/JNK1-dependent apoptosis in
human acute myeloid leukaemia cells. Br J Haematol. 151:70–83.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shanmugam R, Kusumanchi P, Cheng L, Crooks
P, Neelakantan S, Matthews W, Nakshatri H and Sweeney CJ: A
water-soluble parthenolide analogue suppresses in vivo prostate
cancer growth by targeting NFkappaB and generating reactive oxygen
species. Prostate. 70:1074–1086. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Holcomb BK, Yip-Schneider MT, Waters JA,
Beane JD, Crooks PA and Schmidt CM: Dimethylamino parthenolide
enhances the inhibitory effects of gemcitabine in human pancreatic
cancer cells. J Gastrointest Surg. 16:1333–1340. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yip-Schneider MT, Nakshatri H, Sweeney CJ,
Marshall MS, Wiebke EA and Schmidt CM: Parthenolide and sulindac
cooperate to mediate growth suppression and inhibit the nuclear
factor-kappa B pathway in pancreatic carcinoma cells. Mol Cancer
Ther. 4:587–594. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang SQ, Zhang SH, Xue XH, Wang XJ and
Jiang JT: Synergism between a siRNA targeted to survivin and 5-FU
in inhibiting MCF-7 cell proliferation in vitro. Nan Fang Yi Ke Da
Xue Xue Bao. 26:251–254. 2006.PubMed/NCBI
|
|
12
|
Gunn EJ, Williams JT, Huynh DT, Iannotti
MJ, Han C, Barrios FJ, Kendall S, Glackin CA, Colby DA and Kirshner
J: The natural products parthenolide and andrographolide exhibit
anti-cancer stem cell activity in multiple myeloma. Leuk Lymphoma.
52:1085–1097. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gao ZW, Zhang DL and Guo CB: Paclitaxel
efficacy is increased by parthenolide via nuclear factor-kappaB
pathways in in vitro and in vivo human non-small cell lung cancer
models. Curr Cancer Drug Targets. 10:705–715. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu D, Liu Y, Liu M, Ran L and Li Y:
Reversing resistance of multidrug-resistant hepatic carcinoma cells
with parthenolide. Future Oncol. 9:595–604. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sohma I, Fujiwara Y, Sugita Y, Yoshioka A,
Shirakawa M, Moon JH, Takiguchi S, Miyata H, Yamasaki M, Mori M and
Doki Y: Parthenolide, an NF-κB inhibitor, suppresses tumor growth
and enhances response to chemotherapy in gastric cancer. Cancer
Genomics Proteomics. 8:39–47. 2011.PubMed/NCBI
|
|
16
|
Al-Fatlawi AA, Al-Fatlawi AA, Irshad M,
Rahisuddin and Ahmad A: Effect of parthenolide on growth and
apoptosis regulatory genes of human cancer cell lines. Pharm Biol.
53:104–109. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Caldera V, Mellai M, Annovazzi L, Valente
G, Tessitore L and Schiffer D: Stat3 expression and its correlation
with proliferation and apoptosis/autophagy in gliomas. J Oncol.
2008:2192412008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kunigal S, Lakka SS, Sodadasu PK, Estes N
and Rao JS: Stat3-siRNA induces Fas-mediated apoptosis in vitro and
in vivo in breast cancer. Int J Oncol. 34:1209–1220.
2009.PubMed/NCBI
|
|
19
|
Barré B, Vigneron A, Perkins N, Roninson
IB, Gamelin E and Coqueret O: The STAT3 oncogene as a predictive
marker of drug resistance. Trends Mol Med. 13:4–11. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huang S, Chen M, Shen Y, Shen W, Guo H,
Gao Q and Zou X: Inhibition of activated Stat3 reverses drug
resistance to chemotherapeutic agents in gastric cancer cells.
Cancer Lett. 315:198–205. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kohsaka S, Wang L, Yachi K, Mahabir R,
Narita T, Itoh T, Tanino M, Kimura T, Nishihara H and Tanaka S:
STAT3 inhibition overcomes temozolomide resistance in glioblastoma
by downregulating MGMT expression. Mol Cancer Ther. 11:1289–1299.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yue P, Zhang X, Paladino D, Sengupta B,
Ahmad S, Holloway RW, Ingersoll SB and Turkson J: Hyperactive EGF
receptor, Jaks and Stat3 signaling promote enhanced colony-forming
ability, motility and migration of cisplatin-resistant ovarian
cancer cells. Oncogene. 31:2309–2322. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Duan Z, Ames RY, Ryan M, Hornicek FJ,
Mankin H and Seiden MV: CDDO-Me, a synthetic triterpenoid, inhibits
expression of IL-6 and Stat3 phosphorylation in multi-drug
resistant ovarian cancer cells. Cancer Chemother Pharmacol.
63:681–689. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lei XY, Zhong M, Feng LF, Yan CY, Zhu BY,
Tang SS and Liao DF: Silencing of Bcl-XL expression in human
MGC-803 gastric cancer cells by siRNA. Acta Biochim Biophys Sin
(Shanghai). 37:555–560. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Min H and Wei-hong Z: Constitutive
activation of signal transducer and activator of transcription 3 in
epithelial ovarian carcinoma. J Obstet Gynaecol Res. 35:918–925.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Peyser ND, Freilino M, Wang L, Zeng Y, Li
H, Johnson DE and Grandis JR: Frequent promoter hypermethylation of
PTPRT increases STAT3 activation and sensitivity to STAT3
inhibition in head and neck cancer. Oncogene. 35:1163–1169. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yu LF, Zhu YB, Qiao MM, Zhong J, Tu SP and
Wu YL: Constitutive activation and clinical significance of Stat3
in human gastric cancer tissues and cell lines. Zhonghua Yi Xue Za
Zhi. 84:2064–2069. 2004.(In Chinese). PubMed/NCBI
|
|
28
|
Song JM, Qian X, Upadhyayya P, Hong KH and
Kassie F: Dimethylaminoparthenolide, a water soluble parthenolide,
suppresses lung tumorigenesis through down-regulating the STAT3
signaling pathway. Curr Cancer Drug Targets. 14:59–69. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Carlisi D, D'Anneo A, Angileri L,
Lauricella M, Emanuele S, Santulli A, Vento R and Tesoriere G:
Parthenolide sensitizes hepatocellular carcinoma cells to TRAIL by
inducing the expression of death receptors through inhibition of
STAT3 activation. J Cell Physiol. 226:1632–1641. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Czyz M, Lesiak-Mieczkowska K, Koprowska K,
Szulawska-Mroczek A and Wozniak M: Cell context-dependent
activities of parthenolide in primary and metastatic melanoma
cells. Br J Pharmacol. 160:1144–1157. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Cheng G and Xie L: Parthenolide induces
apoptosis and cell cycle arrest of human 5637 bladder cancer cells
in vitro. Molecules. 16:6758–6768. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ghantous A, Saikali M, Rau T,
Gali-Muhtasib H, Schneider-Stock R and Darwiche N: Inhibition of
tumor promotion by parthenolide: Epigenetic modulation of p21.
Cancer Prev Res (Phila). 5:1298–1309. 2012. View Article : Google Scholar : PubMed/NCBI
|