Introduction
Cervical cancer is one of the most common malignant
tumors in the modern gynecological clinical practice, which
seriously affects the life and health of patients and their quality
of life (1). Uterine cavity
brachytherapy and intensity modulated radiation therapy (IMRT) is a
basic clinical treatment for cervical cancer (2). In recent years, the application of
modern image-guided technology has been widely used in
brachytherapy of cervical cancer patients. However, during
radiotherapy, the applicator position is prone to error. If the
error is relatively large, the accuracy and effectiveness of the
treatment are affected (3–5). Here, we discuss the error in applicator
position in after-loading combined radiation therapy for cervical
cancer for the first and second sessions to provide valuable
reference to enhance the therapeutic effect of irradiation in
patients with cervical cancer.
Materials and methods
Patient information
We recruited 22 cases of cervical cancer treated
with radiotherapy in Sichuan Cancer Hospital and Institute
(Chengdu, China) from November 2013 to January 2016. The patients
were aged 25–72 years, with a mean age of 47.1±4.4 years. Clinical
stages: IIb 7 cases, IIIa 9 cases, and IIIb 6 cases. Pathological
type: 17 cases of phosphate cell carcinoma and 5 cases of
adenocarcinoma. The study was approved by the Ethics Committee of
Sichuan Cancer Hospital and Institute and written informed consents
were signed by the patients and/or guardians.
Methods
Main instruments and equipment: GE64 spiral CT
(CT-Sim), Nucletron Simulix-HP simulated locator, Varian Clinac
23EX linear accelerator, Oncentra MasterPlan 3.2 nucletron
after-loading planning application system, and the Fletcher
applicator.
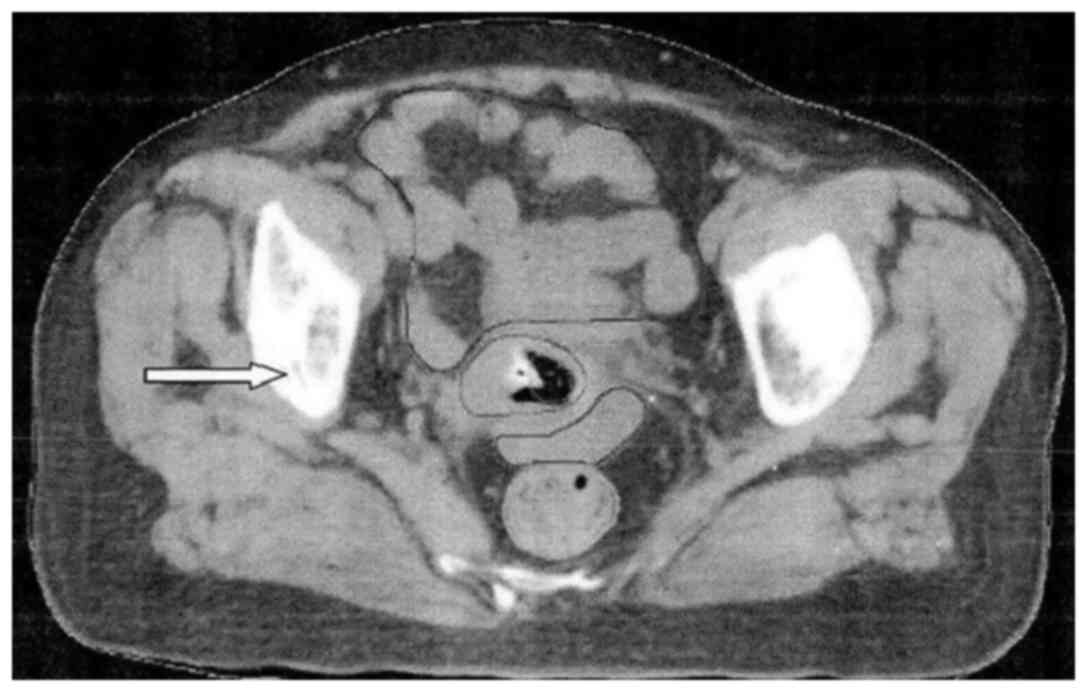
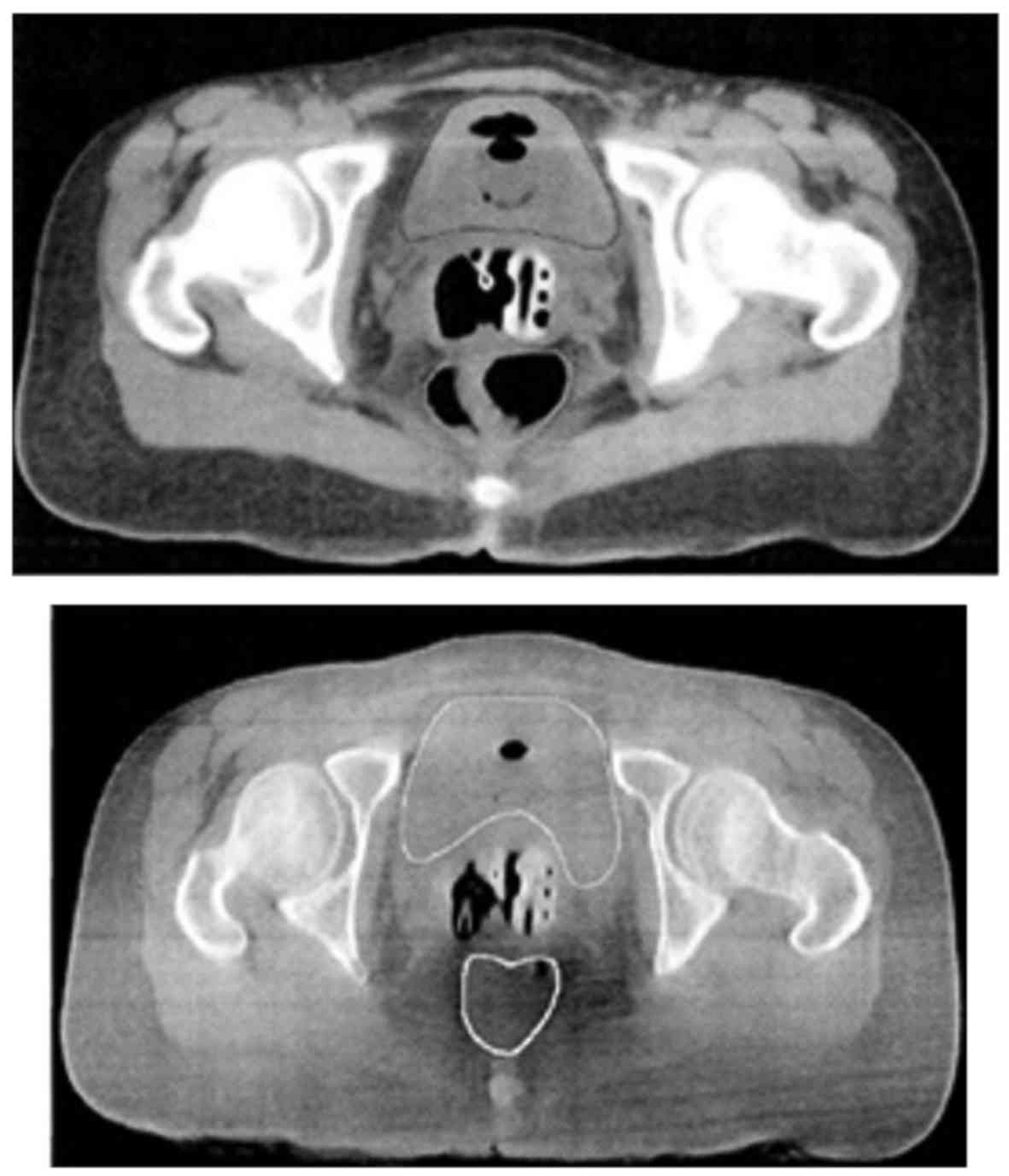
Main treatments: The main links for the radiation
therapy are the evacuation routes of rectal and bladder physiology,
manufacture of vacuum pad and bulk film, and the installation place
of the applicator. Normal saline (250 ml) was injected into the
bladder of the patients. CT-Sim scan, regional delineation of
target location for radiotherapy treatment (Figs. 1 and 2),
scheme design and planning DRR image registration, intra cavity
radiation therapy, electronic portal imaging technology (EPID)
results, in vitro radiation therapy, EPID images, DRR images
fusion (Fig. 3), and the statistics
of error position of the applicator equipment. We also implemented
image fusion processing, applicator position parameter calibration,
and setup verification and other processing technology.
Statistical analysis
IBM SPSS 19.0 (Armonk, NY, USA) was used for all
statistical analysis. Measurement data were expressed as mean ± SD.
The comparison among multiple groups was performed using ANOVA and
the post hoc was Dunnett's test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of the first and second CT-Sim fusion in
the 22 patients in this cohort is shown in Fig. 4. After parameter error calibration,
applicator position errors are shown in Tables I and II. Before calibration, the mean values of
error of the applicator in the horizontal (X-), longitudinal (Y-)
and vertical (Z)-axes were 5.301, 5.216 and 2.576 mm, respectively,
with relatively large errors (Table
I). After calibration, the mean value of error of the
applicator in X-, Y- and Z-axes were 1.876, 2.191 and 1.821 mm,
respectively, and the errors were significantly smaller.
 | Table I.Error parameters of applicator
position of the first and second CT-Sim scan fusion. |
Table I.
Error parameters of applicator
position of the first and second CT-Sim scan fusion.
| Error (mm) | Mean value | Standard
deviation | Standard error | 95% CL lower
limit | 95% CL upper
limit |
|---|
| X-direction | 5.301 | 0.2696 | 0.0604 | 5.175 | 5.427 |
| Y-direction | 5.216 | 0.1928 | 0.0432 | 5.126 | 5.306 |
| Z-direction | 2.576 | 0.2338 | 0.0524 | 2.467 | 5.685 |
| P-value | <0.05 |
|
|
|
|
 | Table II.Error parameters of applicator
position after calibration. |
Table II.
Error parameters of applicator
position after calibration.
| Error (mm) | Mean value | Standard
deviation | Standard error | 95% CL lower
limit | 95% CL upper
limit |
|---|
| X-direction | 1.876 | 0.1294 | 0.290 | 1.8151 | 1.936 |
| Y-direction | 2.191 | 0.2031 | 0.0451 | 2.0901 | 2.281 |
| Z-direction | 1.821 | 0.1362 | 0.0305 | 1.7561 | 1.885 |
| P-value | <0.05 |
|
|
|
|
The results of EPID and DRR image indicate that, in
the process of radiation therapy metastasis, the position errors of
applicator on the direction of X-, Y- and Z-axes were less than 2.0
mm for the 22 cases of patients (Fig.
4). The errors of applicator before and after calibration had
statistical significance (P<0.05).
Discussion
Cervical cancer is a common gynecological malignant
tumor, and its clinical incidence is only second to breast cancer
(6–8).
Study shows that when cervical cancer patients receive timely,
effective, and systematic radiation therapy, the 5-year survival
rate can be increased to 45–51% (9–12). In
recent years, with the rapid development of medical radiation in
China, traditional radiotherapy technology has gradually been
replaced by three-dimensional conformal radiotherapy and other
modern treatment technologies. In this context, the influence of
applicator position error on the final treatment effectiveness has
gradually aroused widespread concern (13–17).
The present study shows that, before calibration,
the mean values of errors of the applicator in the X-, Y- and
Z-axes had relatively large errors. After calibration, the mean
values of error of the applicator in X-, Y- and Z-axes were
significantly smaller. After the first and second CT-Sim contrast
fusion, DR diagram and implementation of DRR registration of
treatment plan, the parameter error of applicator position becomes
small. Further analysis showed that the change of position of the
applicator after registration was concentrated near the bilateral
ovoid. The possible reasons are that location corresponds to the
anatomical location is the vaginal fornix, and the structure of
this position is flabby. During gauze packing in the surgery, it is
easy to change the applicator position by the change of the dome
shape (18,19). Another reason may be that after the
completion of the filling surgery, when the vagina speculum is
removed, because the tension change makes the vagina space change,
the applicator position changes significantly (20,21).
In conclusion image registration technique of
radiotherapy planning for error parameter calibration processing
can reduce the horizontal spatial error of applicator position, and
improve the accuracy and effectiveness during treatment in the
treatment of cervical cancer with intracavity and in vitro
combined radiotherapy. These advantages make this technique worthy
of promotion.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hoskin PJ: Hypoxia dose painting in
prostate and cervix cancer. Acta Oncol. 54:1259–1262. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Assenholt MS, Vestergaard A, Kallehauge
JF, Mohamed S, Nielsen SK, Petersen JB, Fokdal L, Lindegaard JC and
Tanderup K: Proof of principle: Applicator-guided stereotactic IMRT
boost in combination with 3D MRI-based brachytherapy in locally
advanced cervical cancer. Brachytherapy. 13:361–368. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Blanco AI, Meyer LA, George V, Teh BS,
Rios A, Ferachi K, Rodriguez M, Gonzalez A and Dalrymple J: The use
of modern imaging technologies in radiation therapy of cervical
cancer. J Radiat Oncol. 4:1–10. 2015. View Article : Google Scholar
|
|
4
|
Dimopoulos JC, Kirisits C, Petric P, Georg
P, Lang S, Berger D and Pötter R: The Vienna applicator for
combined intracavitary and interstitial brachytherapy of cervical
cancer: Clinical feasibility and preliminary results. Int J Radiat
Oncol Biol Phys. 66:83–90. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hashim N, Jamalludin Z, Ung NM, Ho GF,
Malik RA and Phua VC: CT based 3-dimensional treatment planning of
intracavitary brachytherapy for cancer of the cervix: Comparison
between dose-volume histograms and ICRU point doses to the rectum
and bladder. Asian Pac J Cancer Prev. 15:5259–5264. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ma JK, Mourad WF, Allbright R,
Packianathan S, Harrell LM, Chinchar E, Nguyen A and Vijayakumar S:
Short-term clinical outcome and dosimetric comparison of tandem and
ring versus tandem and ovoids intracavitary applicators. J Contemp
Brachytherapy. 7:218–223. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Salcedo MP, Milbourne AM, Jhingran A,
Eifel PJ, Ramirez PT and Schmeler KM: High-grade cervical dysplasia
following radiation therapy for invasive cervical cancer: A report
of four cases. Case Rep Oncol. 8:217–221. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Klopp A, Mourtada F, Yu Z, Beadle B,
Lawyer A, Jhingran A and Eifel P: Pilot study of a new
ct-compatible intracavitary brachytherapy applicator for treatment
of cervical cancer. Brachytherapy. 9:115–123. 2010. View Article : Google Scholar
|
|
9
|
Ghose S, Holloway L, Lim K, Chan P, Veera
J, Vinod SK, Liney G, Greer PB and Dowling J: A review of
segmentation and deformable registration methods applied to
adaptive cervical cancer radiation therapy treatment planning.
Artif Intell Med. 64:75–87. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ghadjar P, Budach V, Köhler C, Jantke A
and Marnitz S: Modern radiation therapy and potential fertility
preservation strategies in patients with cervical cancer undergoing
chemoradiation. Radiat Oncol. 10:502015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Low DA, Grigsby PW, Dempsey JF, Mutic S,
Williamson JF, Markman J, Chao KS, Klein EE and Purdy JA:
Applicator-guided intensity-modulated radiation therapy. Int J
Radiat Oncol Biol Phys. 52:1400–1406. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chakraborty S, Geetha M, Dessai S and
Patil VM: How well do elderly patients with cervical cancer
tolerate definitive radiochemotherapy using RapidArc? Results from
an institutional audit comparing elderly versus younger patients. E
Cancer Med Sci. 8:4842014.
|
|
13
|
Yong JS, Ung NM, Jamalludin Z, Malik RA,
Wong JH, Liew YM and Ng KH: Dosimetric impact of applicator
displacement during high dose rate (hdr) cobalt-60 brachytherapy
for cervical cancer: A planning study. Radiat Phys Chem.
11:264–271. 2016. View Article : Google Scholar
|
|
14
|
Rezaeealam B: Applicator modeling for
electromagnetic thermotherapy of cervix cancer. Electromagn Biol
Med. 34:43–47. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Thompson SR, Delaney GP, Gabriel GS and
Barton MB: Patterns of care study of brachytherapy in New South
Wales: Cervical cancer treatment quality depends on caseload. J
Contemp Brachytherapy. 6:28–32. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nomden CN, de Leeuw AA, Moerland MA,
Roesink JM, Tersteeg RJ and Jürgenliemk-Schulz IM: Clinical use of
the Utrecht applicator for combined intracavitary/interstitial
brachytherapy treatment in locally advanced cervical cancer. Int J
Radiat Oncol Biol Phys. 82:1424–1430. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kirchheiner K, Nout RA, Lindegaard JC,
Haie-Meder C, Mahantshetty U, Segedin B, Jürgenliemk-Schulz IM,
Hoskin PJ, Rai B, Dörr W, et al: EMBRACE Collaborative Group:
Dose-effect relationship and risk factors for vaginal stenosis
after definitive radio(chemo)therapy with image-guided
brachytherapy for locally advanced cervical cancer in the EMBRACE
study. Radiother Oncol. 118:160–166. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dewitt KD, Hsu IC, Speight J, Weinberg VK,
Lessard E and Pouliot J: 3D inverse treatment planning for the
tandem and ovoid applicator in cervical cancer. Int J Radiat Oncol
Biol Phys. 63:1270–1274. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Petric P, Hudej R, Hanuna O, Marolt P,
Al-Hammadi NM, Riyas MP and Segedin B: MRI-assisted cervix cancer
brachytherapy pre-planning, based on application in paracervical
anaesthesia: Final report. Radiol Oncol. 48:293–300. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mazeron R, Castelnau-Marchand P, Dumas I,
del Campo ER, Kom LK, Martinetti F, Farha G, Tailleur A, Morice P,
Chargari C, et al: Impact of treatment time and dose escalation on
local control in locally advanced cervical cancer treated by
chemoradiation and image-guided pulsed-dose rate adaptive
brachytherapy. Radiother Oncol. 114:257–263. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yin G, Wang P, Lang J, Tian Y, Luo Y, Fan
Z and Tam KY: Dosimetric study for cervix carcinoma treatment using
intensity modulated radiation therapy (IMRT) compensation based on
3D intracavitary brachytherapy technique. J Contemp Brachytherapy.
8:221–232. 2016. View Article : Google Scholar : PubMed/NCBI
|