Introduction
Polymyositis and myocarditis associated with thymoma
are exceptionally rare and are usually accompanied by myasthenia
gravis (MG). In 1944, Giordano and Haymondo reported the first
autopsied case with the four diseases, MG, thymoma, giant cell
polymyositis and cardiomyositis (1). In 1969, Burke and colleagues who had
observed ST segment depression and T-wave inversion on the
electrocardiogram (ECG) in one case, reported that the patient
suddenly died due to rapid progression of heart failure (2). In their study, Namba and colleagues
reported 13 cases of giant cell polymyositis, cardiomyositis and
thymoma (3). Gidron and colleagues
reported a thymoma case with fatal myocarditis following treatment
with carboplatin and paclitaxel (4). We experienced a similar case.
Case report
A 58-year-old male presented to Nagoya City
University Medical School, Japan, with stage IVa type B2 thymoma.
An asymptomatic, anterior mediastinal mass had been identified 2
years previously upon routine chest X-ray examination, but the
patient had not received any treatment prior to presentation. A
biopsy was performed at a local hospital and the tumor was
diagnosed as a type B2 thymoma. Chest radiography revealed left
pleural effusion and a widened mediastinum with multiple chest wall
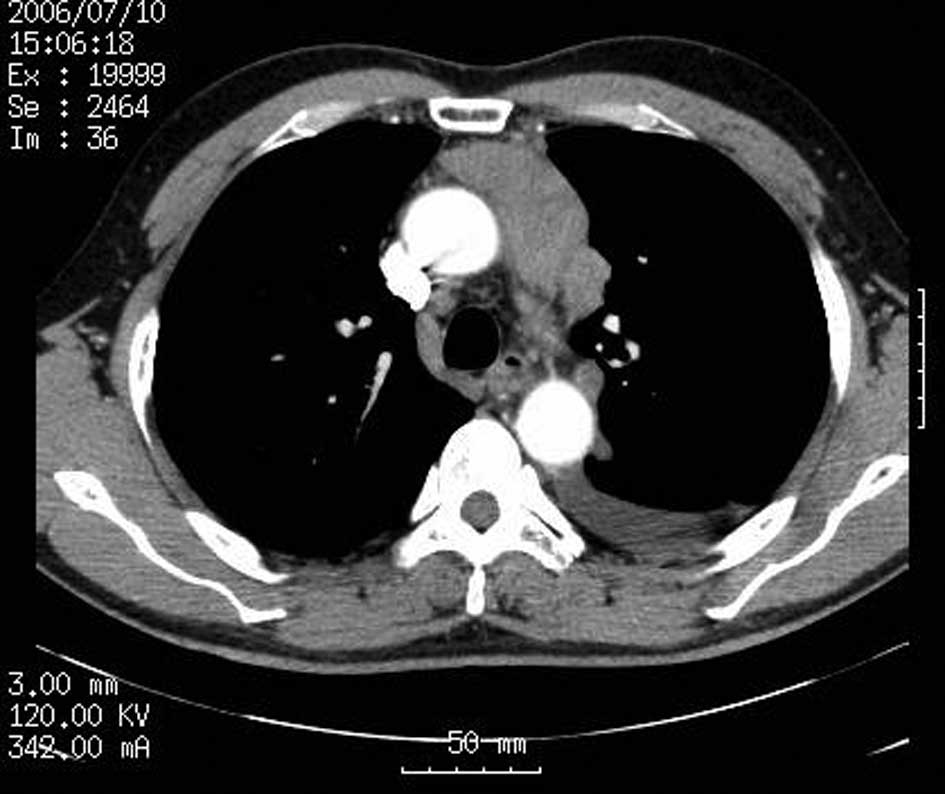
masses. Computed tomography (CT) revealed that the tumor existed in
the anterior mediastinum and that multiple dissemination existed in
the left thoracic cavity, with pleural effusion (Fig. 1). Acetylcholine receptor binding
antibody titers were positive at 42 nmol/l (normal <0.3 nmol/l),
although the patient had no symptoms of MG. The study was approved
by the Institutional Review Board of the hospital. The patient
provided informed consent and received two courses of carboplatin,
550 mg and paclitaxel, 330 mg. No problems were experienced
following the first cycle of chemotherapy.
However, 18 days after receiving the second cycle of
chemotherapy, the patient developed a low-grade fever. Then, 21
days after receiving chemotherapy, the patient was admitted to
hospital due to general fatigue. Physical examination was notable
for mild diffuse muscle tenderness. Laboratory examination revealed
that serum levels of creatinine phosphokinase (7271 U/l; normal,
62-287 U/l), alanine aminotransferase (469 U/l; normal 6-37 U/l)
and aspartate aminotransferase (561U/l; normal 10-33 U/l) were
elevated. Serum electrolytes and calcium were normal. Viral titers
were negative. An evoked electromyogram showed that electrical
activity produced by the skeletal muscles was within the normal
range. The patient tested negative for Tensilon (edrophonium
chloride). CT revealed that the tumor size had increased. The
patient developed progressive muscle weakness and suddenly
succumbed in hospital on day 9.
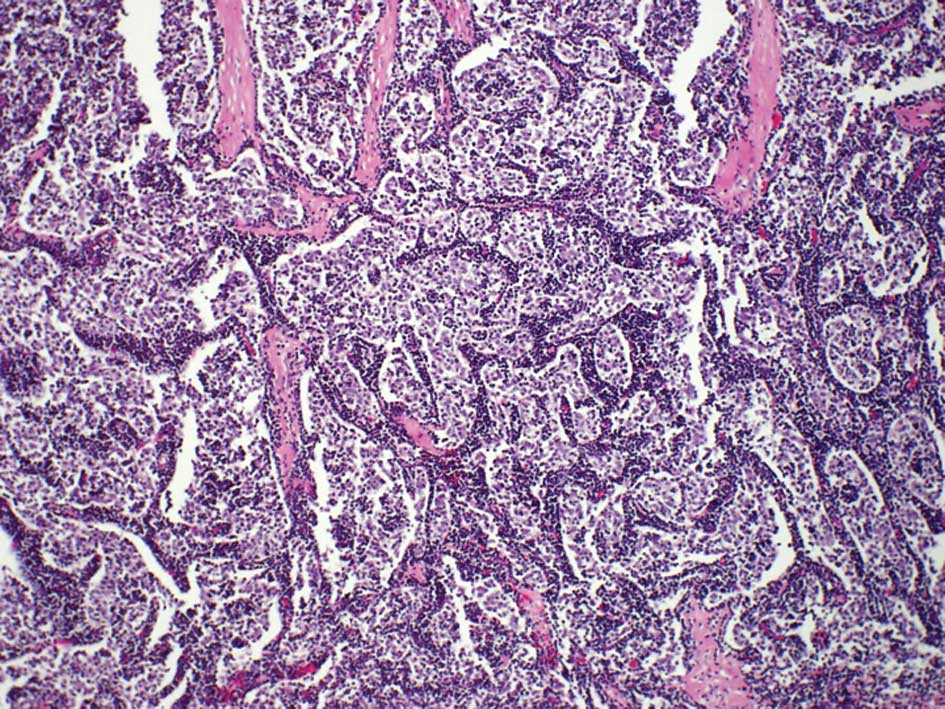
An autopsy revealed that type B2 thymoma (Fig. 2), invasion of the left pleura,
pericardium, diaphragm and multiple dissemination existed in the
left thoracic cavity, with pleural effusion. At autopsy the heart
weighed 330 g and there was no evidence of valvular or significant
coronary artery disease. Numerous skeletal muscle groups and the
myocardium exhibited diffuse lymphocytic infiltration,
predominantly by CD8-positive T cells. The inflammatory cells were
predominantly mononuclear cells, including lymphocytes, plasma
cells and macrophages. Multinucleated giant cells also existed in
muscles and myocardium (Fig. 3). In
the existing literature, certain instances of the syndrome of giant
cell myocarditis and polymyositis associated with invasive thymoma
have been reported, and this case is also thought to belong to this
syndrome.
Discussion
Thymoma is one of the most common tumors in the
anterior mediastinum. Thymoma typically grows slowly when it is at
the early stages. Conversely, a number of studies have shown poorer
prognosis for patients with invasive thymomas (5,6). Since
complete resection is often impossible for advanced-stage thymoma,
multimodal treatment strategies are required (7).
Polymyosis and myocarditis associated with thymoma
are exceptionally rare and usually accompanied by MG (8,9). In a
review of 377,841 autopsies over a 20-year period, Wakafuji and
Okada (10) found myocarditis in
0.11% and giant cell myocarditis in 0.007% of cases. Giant cell
myocarditis generally affects young to middle-aged adults of either
gender (11). It is characterized
by acute heart failure, ventricular arrhythmias or heart block,
which progress rapidly to mortality, usually within 10 days
(12); although some cases showed a
good response to steroid, azathioprine and cyclosporine therapy
(9,13,14).
However, the mechanisms remain unknown, and it has been speculated
in previous reports that antimyocardial or antiskeletal muscle
antibodies may be responsible for the abnormalities.
Giant cell myocarditis usually occurs in isolation,
but has been reported in association with a variety of autoimmune
diseases (12,15,16)
and chronic infections (17,18).
It is diagnosed in approximately 1% of patients with thymoma
(12). Almost 30 cases have been
reported worldwide thus far, and the present patient was the fourth
case of thymoma associated with myositis and myocarditis in Japan
(8,19,20).
However, all four were fatal cases. Tanahashi and colleagues
reported that glucocorticoid pulse therapies were not effective
(8). Anecdotal reports and animal
studies have suggested that immunosuppressive treatment may be
effective (14,21,22),
but there are no randomized controlled trials to support this
theory. There is some evidence to suggest an autoimmune process,
and activated T lymphocytes appear to be important for myocarditis
development. Myocarditis has been reported to recur in transplanted
hearts (22,23). The defective immunity found in
patients with thymoma is thought to result in a giant cell immune
reaction against myofibers (16).
While on chemotherapy for invasive thymoma, our patient developed
fatal fulminant polymyositis and myocarditis without clinical
evidence of MG. An autoimmune mechanism was indicated by the
diffuse infiltration of muscles by lymphocytes. Whether
chemotherapy triggered this syndrome remains to be determined.
Notably, 18 days after receiving the second cycle of chemotherapy,
the patient developed high-grade fever. The infection may be
correlated with neutropenia caused by chemotherapy, which may
trigger the syndrome. Increased awareness of giant cell myocarditis
in association with thymoma should lead to early recognition and
treatment. This case was the second associated with fatal
myocarditis and polymyositis following treatment with carboplatin
and paclitaxel (4).
Acknowledgements
This study was supported in part by the Health and
Labour Sciences Research Grant on Intractable Diseases
(neuroimmunological diseases) from the Ministry of Health, Labour
and Welfare of Japan.
References
|
1
|
Giordano A and Haymondo J: Myasthenia
gravis: a report of two cases with necropsy findings. Am J Clin
Pathol. 14:253–265. 1944.
|
|
2
|
Burke JS, Medline NM and Katz A: Giant
cell myocarditis and myositis. Associated with thymoma and
myasthenia gravis. Arch Pathol. 88:359–366. 1969.PubMed/NCBI
|
|
3
|
Namba T, Brunner NG and Grob D: Idiopathic
giant cell polymyositis. Report of a case and review of the
syndrome. Arch Neurol. 31:27–30. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gidron A, Quadrini M, Dimov N, et al:
Malignant thymoma associated with fatal myocarditis and
polymyositis in a 32-year-old woman with a history of hairy cell
leukemia. Am J Cin Oncol. 29:213–214. 2006.PubMed/NCBI
|
|
5
|
Masaoka A, Monden Y, Nakahara K, et al:
Follow-up study of thymomas with special reference to their
clinical stages. Cancer. 48:2485–2492. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kondo K and Monden Y: Therapy for thymic
epithelial tumors: a clinical study of 1320 patients from Japan.
Ann Thorac Surg. 76:878–885. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Venuta F, Rendina EA, Pescarmona EO, et
al: Multimodality treatment of thymoma: a prospective study. Ann
Thorac Surg. 64:1585–1592. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tanahashi N, Sato H, Nogawa S, et al: A
case report of giant cell myocarditis and myositis observed during
the clinical course of invasive thymoma associated with myasthenia
gravis. Keio J Med. 53:30–42. 2004.PubMed/NCBI
|
|
9
|
Ko KF, Ho T and Chan KW: Autoimmune
chronic active hepatitis and polymyositis in a patient with
myasthenia gravis and thymoma. J Neurol Neurosurg Psychiatry.
59:558–559. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wakafuji S and Okada R: Twenty year
autopsy statistics of myocarditis incidence in Japan. Jpn Circ J.
50:1288–1293. 1986.PubMed/NCBI
|
|
11
|
Glennon PE, Petersen ME and Sheppard MN:
Fatal giant cell myocarditis after resection of thymoma. Heart.
75:531–532. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Davies MJ, Pomerance A and Teare RD:
Idiopathic giant cell myocarditis - a distinctive
clinoco-pathological entity. Br Heart J. 37:192–195. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ren H, Poston RS, Hruban RH, et al: Long
survival with giant cell myocarditis. Mod Pathol. 6:402–407.
1993.PubMed/NCBI
|
|
14
|
Desjardins V, Pelletier G, Leung TL and
Waters D: Successful treatment of severe heart failure caused by
idiopathic giant cell myocarditis. Can J Cardiol. 8:788–792.
1992.PubMed/NCBI
|
|
15
|
Roberts WC, Kehoe JA, Carpenter DF, et al:
Cardiac valvular lesions in rheumatoid arthritis. Arch Intern Med.
122:141–146. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Humbert P, Faivre R, Fellman D, et al:
Giant cell myocarditis: an autoimmune disease? Am Heart J.
115:485–487. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Reingold IM: Myocardial lesions in
disseminated coccidioidomycosis. Am J Clin Pathol. 20:1044–1049.
1950.PubMed/NCBI
|
|
18
|
Buchibinder NA and Robert WC: Left-sided
valvular active infective endocarditis: a study of forty-five
necropsy patients. Am J Med. 53:20–35. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Suzuki H, Mizuno Y, Kurita T, et al: Rare
type myositis and myocarditis revealed in myasthenia gravis with
malignant thymoma. Saishin-igaku (in Japanese). 31:2417–2424.
1976.
|
|
20
|
Tomimoto H, Akiguchi I, Kameyama M, et al:
Giant cell myositis and myocarditis associated with myasthenia
gravis and thymoma-an autopsy case. Rinsho Shinkeigaku (in
Japanese). 25:688–693. 1985.PubMed/NCBI
|
|
21
|
Zhang S, Kodama M, Hanawa H, et al:
Effects of cyclosporine, predonisolone and aspirin on rat
autoimmune giant cell myocarditis. J Am Coll Cardiol. 21:1254–1260.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kong G, Madden B, Spyrou N, et al:
Response of recurrent giant cell myocarditis in a transplanted
heart to intensive immunosuppression. Eur Heart J. 12:554–557.
1991.PubMed/NCBI
|
|
23
|
Gries W, Farkas D, Winters GL, et al:
Giant cell myocarditis: first report of disease recurrence in the
transplanted heart. J Heart Lung Transplant. 11:370–374.
1992.PubMed/NCBI
|