1. Introduction
Abdominopelvic pain with an associated pelvic mass
is a common emergency. These patients create a management dilemma
for most emergency physicians. This problem usually stems from the
inability of the physical examination to reliably differentiate
between a potential surgical problem (i.e., torsion of an enlarged
ovary, pelvic abscess) and a non-surgical etiology (i.e., ovarian
cyst, uterine myoma). Ultrasonograpy (US), magnetic resonance (MR)
and/or computed tomography (CT) are the gold standard imaging
modalities used to differentiate pelvic masses in female patients
presenting with abdominopelvic pain as an emergency.
Ovarian tumors and uterine myoma constitute the most
common masses in the female pelvis (1,2). The
torsion of enlarged ovaries is one of the most common surgical
gynecological emergencies (1). The
differential diagnosis includes twisted exophytic ovarian fibroma,
pedunculated myoma, peritoneal lipoma and accessory ovary although
it should be noted that these conditions rarely cause acute
abdominopelvic pain. The purpose of this review was to summarize
the differential diagnosis of pelvic masses associated with acute
abdominal pain when normal-appearing ovaries and uterus are
detected.
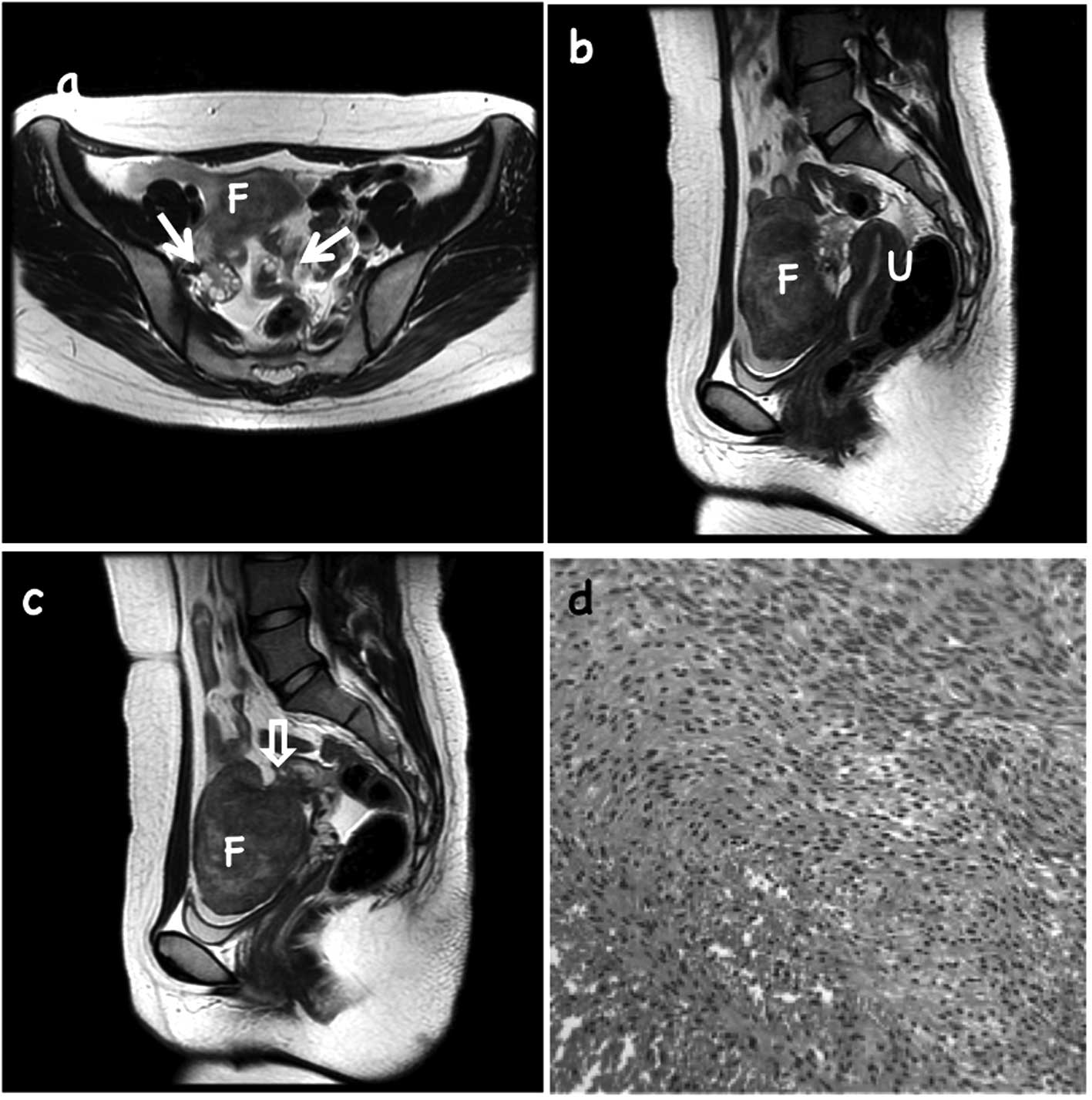
2. Ovarian fibroma
Ovarian fibromas are the most commonly encountered
subtype of sex cord-stromal tumors, accounting for 4–5% of all
ovarian tumors (3–6). It is well known that MR imaging is
useful in diagnosing ovarian fibromas, due to the
characteristically low T1- and T2-weighted signal intensities of
the tumors, caused by the presence of densely packed connective
tissue (3–6). The main differential diagnosis of a
solid adnexal mass with T2 hypointensity includes a uterine
pedunculated myoma and an ovarian fibroma. In a retrospective
analysis, crescent-shaped ovarian tissue may be detected along the
periphery of the tumor in approximately 50% of ovarian fibroma
cases and a normal-appearing ovary closely attached to the tumor in
certain lesions may be misdiagnosed as a subserosal leiomyoma
(5–8). Thus, careful evaluation of the
ipsilateral ovary may aid the differentiation between ovarian
fibroma and uterine leiomyoma. The cystic degeneration of fibromas
has been reported to lead to the pre-operative misdiagnosis of
malignant ovarian epithelial and collision tumors in certain cases
(5,6). Larger or twisted tumors may result in
various MR imaging findings which reflect the degenerative changes,
including cystic degeneration, edematous changes, hemorrhagic
infarction or necrosis as a result of torsion and myxomatous
changes (4,9). Oh et al (5) reported that the ipsilateral ovaries
were identified in half of the ovarian fibroma cases included in
the study. The ovaries had a preserved, normal-appearing ovoid
shape, suggesting the exophytic growth of the fibroma from the
periphery of the ovary. Considering the high incidence (50%) of a
long pedicle in ovarian fibromas reported by certain groups
(5,6,10), the
exophytic growth of fibromas is not uncommon. Torsion may occur
incidentally (Fig. 1).
The remaining ovary on the same side as the fibroma
is commonly detected on MR imaging, especially in premenopausal
women, as is the exophytic growth of fibroma from the periphery of
the ovary. Careful evaluation of the relationship between the
ipsilateral ovary and an adnexal mass may be a significant clue in
the differential diagnosis of ovarian fibroma from uterine
leiomyoma, in addition to the characteristic morphology and signal
intensities (5).
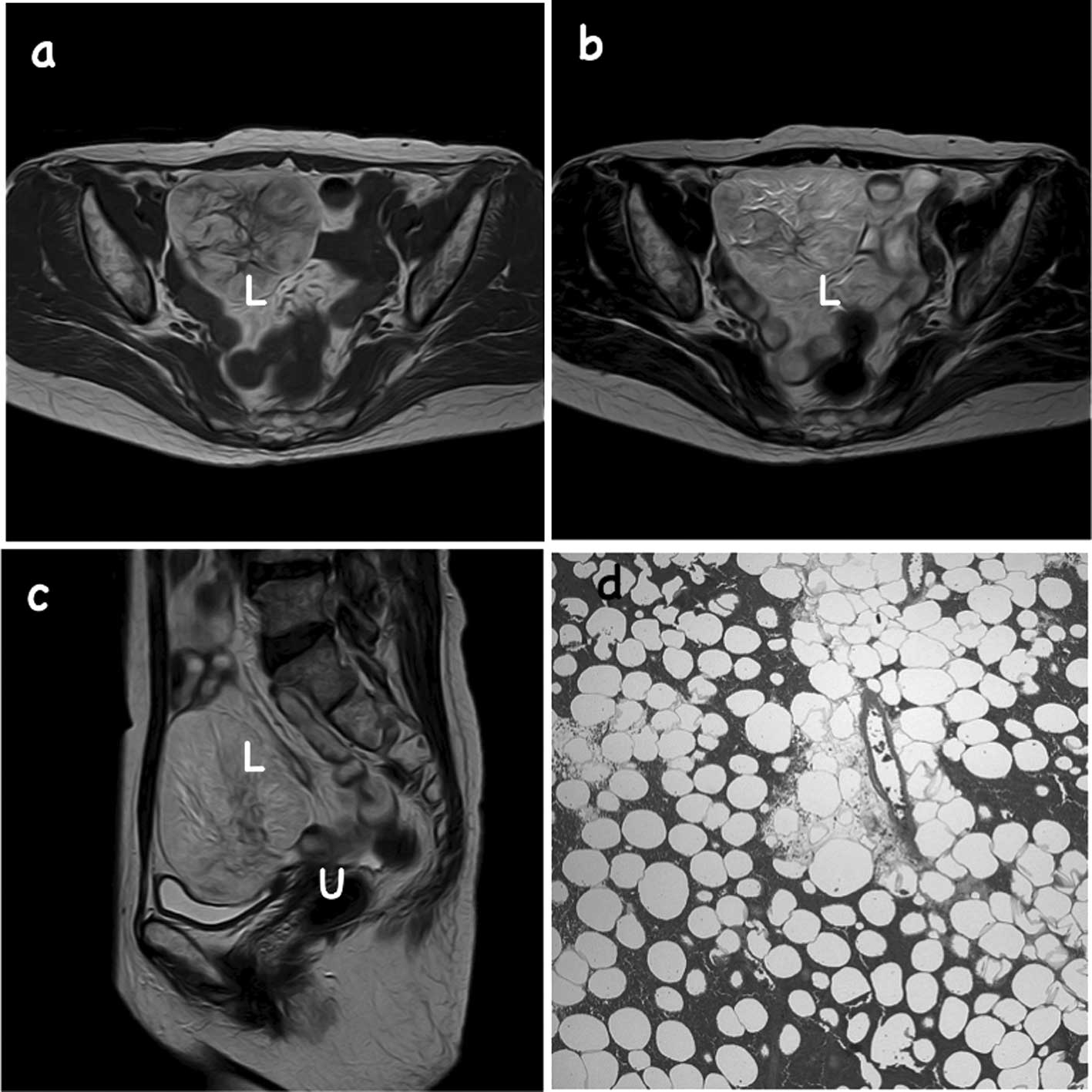
3. Fat-containing tumors in the pelvic
cavity
There are numerous types of fat-containing lesions
which may be found in the intraperitoneal cavity and
retroperitoneal space and treatment varies according to the
classification. Mesenteric panniculitis and pseudolipoma of
Glisson’s capsule may be treated medically or not at all. Adrenal
adenoma, myelolipoma, angiomyolipoma, ovarian teratoma and lipoma
may be surgically resected when the lesions reach a large size or
begin to cause symptoms, whereas liposarcoma and retroperitoneal
teratoma should be resected at an earlier stage (11). Stalk torsion of a lipoma may present
with acute abdominal pain and is an indication for emergency
surgery (Fig. 2) (12,13).
Lipomas are commonly observed benign fat-containing
soft-tissue tumors which may occur singly or, as in lipomatosis, in
larger numbers, and have either a superficial or deep localization.
Lipomas are mostly diagnosed in patients aged 40–60 years and, in
adults, are often located in the trunk. However, previous studies
have reported cases of deep lipomas located in the thorax,
mediastinum, chest wall and retroperitoneum. Cases of
intraperitoneal lipoma are extremely rare (12,14,15).
When visualised with US, adipose tissues, with some
exceptions, are typically hyperechoic. Fat tissues in CT scans have
a low attenuation, ranging from −10 to −100 Hounsfield units (HUs).
However, in certain cases it is difficult to reliably identify fat
tissues using CT, as the mean CT number increases if the proportion
of fat in a voxel is low (11,16).
Finally, MR imaging has a higher sensitivity for microscopic fat
than CT and US imaging (Fig. 2)
(17). In T1-weighted MR images,
adipose tissue appears hyperintense and in T2-weighted fast spin
and gradient-echo images, fat appears immediate- to hyperintense.
MR is based on differences in the resonance frequencies of protons
in different environments, in fat and water for instance, and
methods such as in-phase/opposed-phase chemical shift imaging and
the frequency-selective fat suppression technique mean that fat may
be more reliably identified using MR images than CT or US (11,18).
Although cases of lipoma in the parietal peritoneum
are rare, this type of tumor should be considered in the
differential diagnosis of patients who present with an abdominal
mass and acute abdomen.
4. Pedunculated myoma
Although uterine myomas are the most common type of
tumor in females of reproductive age, the acute torsion of a
subserosal uterine leiomyoma is a rare complication (2,19). The
torsion of the vascular pedicle of a subserosal leiomyoma may cause
ischemic gangrene and peritonitis (2,20,21).
The diagnosis is difficult and is usually made during exploratory
laparotomy.
There are a number of techniques that may be used in
the identification of subserosal leiomyoma. The tumor may appear as
a lesion lateral to the uterus in transvaginal US, but the pedicle
of the subserous leiomyoma may be thin and invisible to US, meaning
that a definitive diagnosis is rarely made using this technique
(22). A CT scan may be performed
as an alternative investigation and certain authors have reported
signs which distinguish between ovarian and uterine masses,
including a pedunculated myoma node (22,23).
MR imaging is another non-invasive method used to detect and
analyze uterine leiomyomas. This method is more sensitive and
specific than US, has a good contrast resolution and produces a
characteristic signal for uterine leiomyomas (2,21,24).
Non-complicated myomas appear hypointense and homogenous in
T2-weighted images and isointense in T1-weighted images compared
with the myometrium (25,26). Necrotic leiomyomas, however, have a
heterogeneous and hyperintense T2 signal and a hyper- or isointense
T1 signal, dependent on whether the necrosis is due to hemorrhage
or ischemia. MR imaging also aids diagnosis by facilitating the
study of the anatomy and topography of the pelvis. Following a
definitive or suspected diagnosis, surgical exploration is
indicated and the lesion is typically resolved by excision
(19,26).
5. Tumor within an accessory ovary
With an estimated incidence of between 1/29,000 and
1/700,000 gynecological admissions, ectopic ovarian tissue is
rarely observed. It is difficult to make a narrower estimate of the
incidence due to the lack of a clear and uncontroversial
classification system. A definition of an accessory ovary as being
in close proximity to, and having an association with, a eutopic
ovary and its blood supply was proposed by Wharton (27). Accessory ovaries are commonly
attached to a Fallopian tube or the ligamentous structure of the
ovarian-uterine complex (28,29).
Wharton also defined a supernumerary ovary as ovarian tissue which
has a separate blood supply and is located at a distance from the
eutopic ovaries. Supernumerary ovaries may be located at any point
along the embryological migratory path of the ovarian primordium,
including the mesentery, retroperitoneal space and omentum
(30). Certain studies have
described cases of tumors and/or their torsion arising from an
accessory ovary (31,32). These tumors may preserve the normal
oval shape of the ovary.
6. Pelvic hematoma
Nelson (33)
reported an unusual cause of a pelvic mass caused by domestic
violence. If the social history and high incidence of domestic
violence had been considered, the cause of the mass may have been
diagnosed earlier. Instead, the patient was tested for other
diagnostic entities which occur relatively infrequently.
7. Other problems
Abdominopelvic problems which originate from the
gastrointestinal tract have been documented in previous studies
(34–37). Two cases with torsion of a wandering
spleen detected by pelvic CT have been reported (38). In cases of acute abdomen with a
palpable painful abdominal mass and the absence of the spleen from
its normal location, torsion of a wandering spleen should be
considered in the differential diagnosis.
8. Conclusion
The conditions discussed in this review, although
extremely rare, must be considered in the differential diagnosis of
acute abdomen when a palpable painful pelvic mass is present on
physical and imaging examinations and the two ovaries and uterus
are detected in their normal anatomical locations on radiological
examination. An accurate diagnosis may be most frequently made at
the time of exploratory laparotomy.
References
|
1
|
Lambert M and Villa M: Gynecologic
ultrasound in emergency medicine. Emerg Med Clin North Am.
22:683–696. 2004. View Article : Google Scholar
|
|
2
|
Gupta S and Manyonda I: Acute
complications of fibroids. Best Pract Res Clin Obstet Gynaecol.
23:609–617. 2009. View Article : Google Scholar
|
|
3
|
Bazot M, Daraï E, Nassar-Slaba J, Lafont C
and Thomassin-Naggara I: Value of magnetic resonance imaging for
the diagnosis of ovarian tumors: A review. J Comput Assist Tomogr.
32:712–723. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kitajima K, Kaji Y and Sugimura K: Usual
and unusual MRI findings of ovarian fibroma: Correlation with
pathologic findings. Magn Reson Med Sci. 7:43–48. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Oh S, Rha S, Byun J, Lee Y, Jung S, Jung C
and Kim M: MRI features of ovarian fibromas: Emphasis on their
relationship to the ovary. Clin Radiol. 63:529–535. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Thomassin-Naggara I, Daraï E, Nassar-Slaba
J, Cortez A, Marsault C and Bazot M: Value of dynamic enhanced
magnetic resonance imaging for distinguishing between ovarian
fibroma and subserous uterine leiomyoma. J Comput Assist Tomogr.
31:236–242. 2007. View Article : Google Scholar
|
|
7
|
Troiano R, Lazzarini K, Scoutt L, Lange R,
Flynn S and McCarthy S: Fibroma and fibrothecoma of the ovary: MR
imaging findings. Radiology. 204:795–798. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Outwater E, Siegelman E, Talerman A and
Dunton C: Ovarian fibromas and cystadenofibromas: MRI features of
the fibrous component. J Magn Reson Imaging. 7:465–471. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Takehara M, Saito T, Manase K, Suzuki T,
Hayashi T and Kudo R: Hemorrhagic infarction of fibroma. MR imaging
appearance. Arch Gynecol Obstet. 266:48–49. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sivanesaratnam V, Dutta R and Jayalakshmi
P: Ovarian fibroma - clinical and histopathological
characteristics. Int J Gynaecol Obstet. 33:243–247. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shin N, Kim M, Chung J, Chung Y, Choi J
and Park Y: The differential imaging features of fat-containing
tumors in the peritoneal cavity and retroperitoneum: The
radiologic-pathologic correlation. Korean J Radiol. 11:333–345.
2010. View Article : Google Scholar
|
|
12
|
Barut I, Tarhan O, Cerci C, Ciris M and
Tasliyar E: Lipoma of the parietal peritoneum: an unusual cause of
abdominal pain. Ann Saudi Med. 26:388–390. 2006.PubMed/NCBI
|
|
13
|
Beattie G and Irwin S: Torsion of an
omental lipoma presenting as an emergency. Int J Clin Pract Suppl.
147:130–131. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ozel S, Apak S, Ozercan I and Kazez A:
Giant mesenteric lipoma as a rare cause of ileus in a child: Report
of a case. Surg Today. 34:470–472. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sato M, Ishida H, Konno K, Komatsuda T,
Naganuma H, Segawa D, Watanabe S and Ishida J: Mesenteric lipoma:
report of a case with emphasis on US findings. Eur Radiol.
12:793–795. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Prasad S, Wang H, Rosas H, Menias C, Narra
V, Middleton W and Heiken J: Fat-containing lesions of the liver:
Radiologic-pathologic correlation. Radiographics. 25:321–331. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kim T, Murakami T, Oi H, Tsuda K,
Matsushita M, Tomoda K, Fukuda H and Nakamura H: CT and MR imaging
of abdominal liposarcoma. Am J Roentgenol. 166:829–833. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Pereira J, Sirlin C, Pinto P and Casola G:
CT and MR imaging of extrahepatic fatty masses of the abdomen and
pelvis: techniques, diagnosis, differential diagnosis, and
pitfalls. Radiographics. 25:69–85. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gaym A and Tilahun S: Torsion of
pedunculated subserous myoma - a rare cause of acute abdomen.
Ethiop Med J. 45:203–207. 2007.PubMed/NCBI
|
|
20
|
Bennett G, Slywotzky C and Giovanniello G:
Gynecologic causes of acute pelvic pain: spectrum of CT findings.
Radiographics. 22:785–801. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Maubon A, Aubard Y, Berkane V,
Camezind-Vidal M, Marès P and Rouanet J: Magnetic resonance imaging
of the pelvic floor. Abdom Imaging. 28:217–225. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lee J, Jeong Y, Park J and Hwang J:
‘Ovarian vascular pedicle’ sign revealing organ of origin of a
pelvic mass lesion on helical CT. Am J Roentgenol. 181:131–137.
2003.
|
|
23
|
Roy C, Bierry G, El Ghali S, Buy X and
Rossini A: Acute torsion of uterine leiomyoma: CT features. Abdom
Imaging. 30:120–123. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Robert Y, Launay S, Mestdagh P, Moisan S,
Boyer C, Rocourt N and Cosson M: MRI in gynecology. J Gynecol
Obstet Biol Reprod (Paris). 31:417–439. 2002.(In French).
|
|
25
|
Hricak H, Tscholakoff D, Heinrichs L,
Fisher M, Dooms G, Reinhold C and Jaffe R: Uterine leiomyomas:
Correlation of MR, histopathologic findings, and symptoms.
Radiology. 158:385–391. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Marcotte-Bloch C, Novellas S, Buratti M,
Caramella T, Chevallier P and Bruneton J: Torsion of a uterine
leiomyoma: MRI features. Clin Imaging. 31:360–362. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wharton L: Two cases of supernumerary
ovary and one of accessory ovary, with analysis of previously
reported cases. Am J Obstet Gynecol. 78:1101–1119. 1959.PubMed/NCBI
|
|
28
|
Nichols J, Zhang X and Bieber E: Case of
accessory ovary in the round ligament with associated
endometriosis. J Minim Invasive Gynecol. 16:216–218. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Benbara A, Tigaizin A and Carbillon L:
Accessory ovary in the utero-ovarian ligament: an incidental
finding. Arch Gynecol Obstet. 283(Suppl 1): 123–125. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kuga T, Esato K, Takeda K, Sase M and
Hoshii Y: A supernumerary ovary of the omentum with cystic change:
report of two cases and review of the literature. Pathol Int.
49:566–570. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fei Ngu S, Lok Tiffany Wan H, Tam Y and
Cheung V: Torsion of a tumor within an accessory ovary. Obstet
Gynecol. 117:477–478. 2011.PubMed/NCBI
|
|
32
|
Liu A, Sun J, Shao W, Jin H and Song W:
Steroid cell tumors, not otherwise specified (NOS), in an accessory
ovary: a case report and literature review. Gynecol Oncol.
97:260–265. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nelson S: An unusual cause of pelvic mass.
Tenn Med. 94:205–207. 2001.
|
|
34
|
Beddy D, DeBlacam C and Mehigan B: An
unusual cause of an acute abdomen - a giant colonic diverticulum. J
Gastrointest Surg. 14:2016–2017. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Banerjee S, Farrell R and Lembo T:
Gastroenterological causes of pelvic pain. World J Urol.
19:166–173. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Barros A, Linhares E, Valadão M, Gonçalves
R, Vilhena B, Gil C and Ramos C: Extragastrointestinal stromal
tumors (EGIST): a series of case reports. Hepatogastroenterology.
58:865–868. 2011.PubMed/NCBI
|
|
37
|
Zighelboim I, Henao G, Kunda A, Gutierrez
C and Edwards C: Gastrointestinal stromal tumor presenting as a
pelvic mass. Gynecol Oncol. 91:630–635. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Dirican A, Burak I, Ara C, Unal B, Ozgor D
and Meydanli M: Torsion of wandering spleen. Bratisl Lek Listy.
110:723–725. 2009.PubMed/NCBI
|