Introduction
Renal angiomyolipoma (AML) is a benign mesenchymal
tumor composed of smooth muscle, adipose tissue and blood vessels.
Although renal AML uniformly follows a benign course, these tumors
are susceptible to provoking life threatening hemorrhages and
replacement of the kidney parenchyma, resulting in renal failure.
To date, the only treatments for renal AML are excision or
embolization.
Various hypotheses have been proposed to explain the
tumorigenesis of renal AML; however, the cellular origin and
histogenesis remain unknown. Lim et al hypothesized that the
tumor originates from a pluripotent cell derived from the neural
crest, which may give rise to smooth muscle cells and melonocytes
(1). Bonetti et al suggested
that lung AMLs are derived from distinctive perivascular
epithelioid cells, a cell type of which no normal counterpart has
been convincingly demonstrated (2).
Barnard and Lajoie proposed that the cell of origin is a smooth
muscle cell resembling a pericyte that exhibits unusual features,
including melanocytic differentiation (3).
As a mesenchymal tumor, classic renal AML is
histologically composed of smooth muscle, adipose tissue and thick
blood vessel walls. This tripartite-tissue composition had lead us
to the hypothesis that renal AML may arise from mesenchymal stem
cells (MSCs). MSCs, which are present in adult bone marrow, are
considered to be multipotent cells, and have the potential to
differentiate into the full lineage of mesenchymal tissues,
including bone, cartilage, fat, muscle and endothelial cells of
blood vessels (4). It has been
demonstrated that MSCs reside in the connective tissues of numerous
organs, including normal and neoplastic kidneys (5–9).
However, stem cell characteristics have not been studied in classic
renal AML and the distribution of MSCs in renal AML remains
unknown.
In this study, we aimed to verify this hypothesis by
establishing a culture method to isolate MSC-like cells from
classic renal AML. Further characterizations of these MSC-like
cells were also confirmed in this study.
Subjects and methods
Subjects
A total of 6 female patients with classic renal AML
underwent partial or radical nephrectomy between March 2009 and
September 2010 at the PLA General Hospital, Beijing, China. The age
of the patients ranged from 16–48 years, with an average age of
40.7±12.4 years. The mean tumor diameter was 11.9±6.2 cm. Classic
AML was diagnosed radiographically based on the presence of fat,
and histologically based on the presence of a combination of smooth
muscle, adipose tissue and thick blood vessel walls. During
surgery, renal AML tissues were obtained from each patient.
Hematoxylin and eosin (H&E) and immunohistochemical staining
for α-smooth muscle actin and HMB-45 was evaluated for each tissue
section by a reporting pathologist to confirm the original
diagnosis. The Ki67 protein was used as a marker to distinguish
between the epithelioid variant of AML (Ki67-positive) and classic
AML (Ki67-negative) (10). Informed
consent was obtained from each patient prior to surgery and the
study was approved by the Institutional Review Board of PLA General
Hospital.
Isolation and primary cell culture of
MSCs from renal AML
Fresh and sterile renal AML tissues were collected
during surgery. The surface of the tumor tissues was removed and
the inner parts were cut into 1–3 mm3-sized pieces. Once
contaminating debris and red blood cells were removed using sterile
phosphate-buffered saline (PBS), the tissues were minced using
scalpels in a tissue culture dish. They were then enzymatically
dissociated in 5 ml 0.075% collagenase (type I; Sigma-Aldrich, St.
Louis, MO, USA) in PBS for 30 min at 37°C with gentle agitation.
The collagenase was inactivated using an equal volume of Dulbecco’s
modified Eagle’s medium (DMEM) containing 10% fetal bovine serum
(FBS). A single-cell suspension was incubated in α-minimun
essential medium (MEM) without ribonucleosides and
deoxyribonucleosides (Invitrogen, Carlsbad, CA, USA) containing 10%
selected FBS, 0.45 mM monothioglycerol (MTG; Sigma-Aldrich), 100
units/ml penicillin (Hyclone, Logan, UT, USA), 100 ng/ml
streptomycin (Hyclone) and 1 ng/ml bFGF (R&D Systems,
Minneapolis, MN, USA). The medium was changed every 2 days and the
adherent cells were harvested by trypsinization when 80–90%
confluence was reached. The cells were then passaged at a ratio of
1:3 for further expansion.
Flow cytometry and immunofluorescence
staining
Single-cell suspensions of MSCs were stained
(11). Aliquots of 3×105
cells were labeled with fluorescein isothiocyanate (FITC)- or
phycoerythrin (PE)-conjugated monoclonal antibodies against human
CD14, CD19, CD29, CD31, CD34, CD44, CD73, CD105, CD144, CD166 and
HLA-DR for 30 min at 4°C. The cells were washed 3 times in cold PBS
and analyzed using a BD FACSCalibur (BD Biosciences, San Jose, CA,
USA). Antibodies recognizing CD14, CD19, CD34, CD73, CD105, CD166
and HLA-DR were purchased from BD Biosciences. Antibodies against
CD29 and CD44 were purchased from BioLegend (San Diego, CA, USA),
and antibodies against CD31 and CD144 were obtained from
eBioscience (San Diego, CA, USA).
Adipogenic and osteogenic differentiation
assay
For adipogenic differentiation, the cultures were
incubated in high-glucose DMEM containing 10% FBS, supplemented
with 10% horse serum, 10−6 M dexamethasone, 0.5 μM
isobutylmethylxanthine, 5 ng/ml insulin, 60 μM indomethacin and
10−4 M hydrocortisone (Sigma-Aldrich) for 1 week.
Characterization of adipocytes was performed using Oil-Red-O
staining. For osteogenic differentiation, cells were incubated in
high-glucose DMEM containing 10% FBS, supplemented with 0.2 mM
ascorbic acid, 10−7 M dexamethasone and 10 mM β-glycerol
phosphate (Sigma-Aldrich) for 2 weeks. The osteogenic
differentiation was evaluated using alkaline phosphatase (ALP)
staining.
Results
Diagnosis and development of cell culture
from renal AML
Specimens from all 6 cases of human renal AML
revealed uniform H&E staining of the thick blood vessel walls
and varying amounts of adipose tissue and smooth muscles.
Immunohistochemical studies revealed uniform expression of the
melanocytic markers HMB-45 and α-smooth muscle actin. All sections
were negative for Ki67, which confirmed classic renal AML.
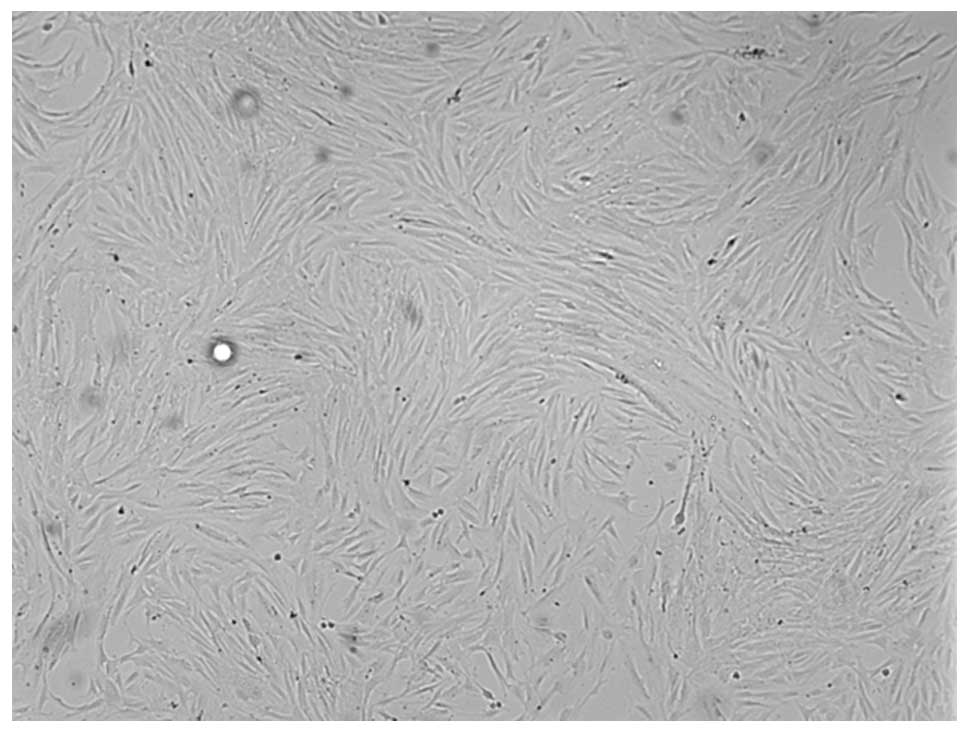
Following 1 day of cell culture, the medium revealed
that the majority of the cells or cell aggregates, including
erythrocytes, were in the suspension of the minced AML tissue. The
culture was then washed to remove these cells and few attached
single cells or cell clumps were observed. Following 4 days in 25
cm2 flasks these attached cells actively proliferated
and reached 80–90% confluency. The morphological observations
demonstrated that these cells had a typical MSC-like appearance
(Fig. 1).
Phenotype
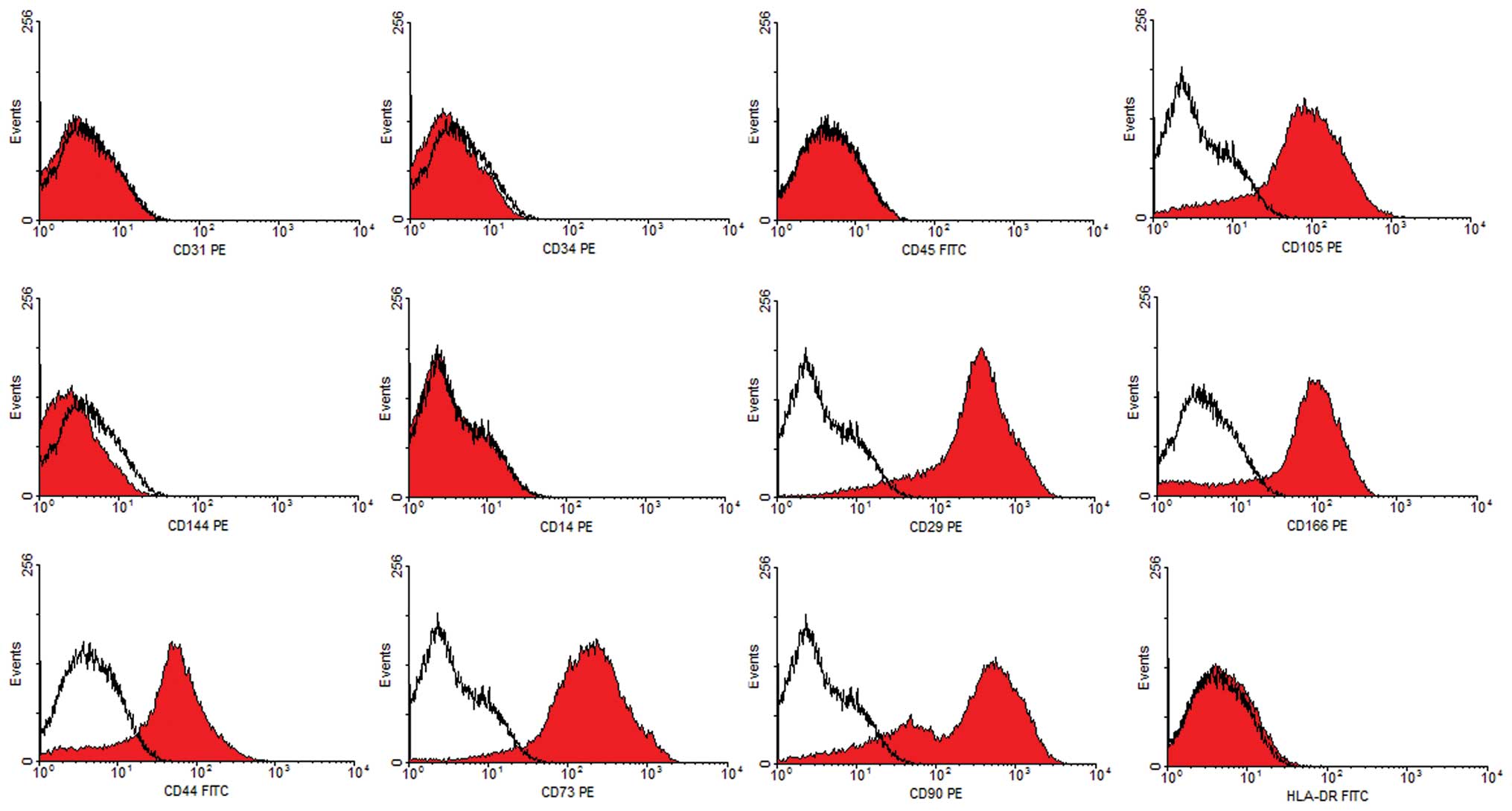
Flow cytometry analyses were used to determine the
immunophenotype of these putative AML-MSCs. We compared the
expression levels of specific surface markers associated with stem
cells. Cultured cells did not express CD14, CD31, CD34, CD45 or
CD144; excluding the growth in the cultures of contaminating
endothelial or hematopoietic cells. Cells expressed all commonly
accepted MSC markers, including CD29, CD44, CD73, CD90 and CD105.
Additionally, they were negative for HLA-DR (Fig. 2). It was demonstrated that these
cells possessed a characteristic MSC immunophenotype, which
parallels the phenotypic profile of human bone marrow
derived-MSCs.
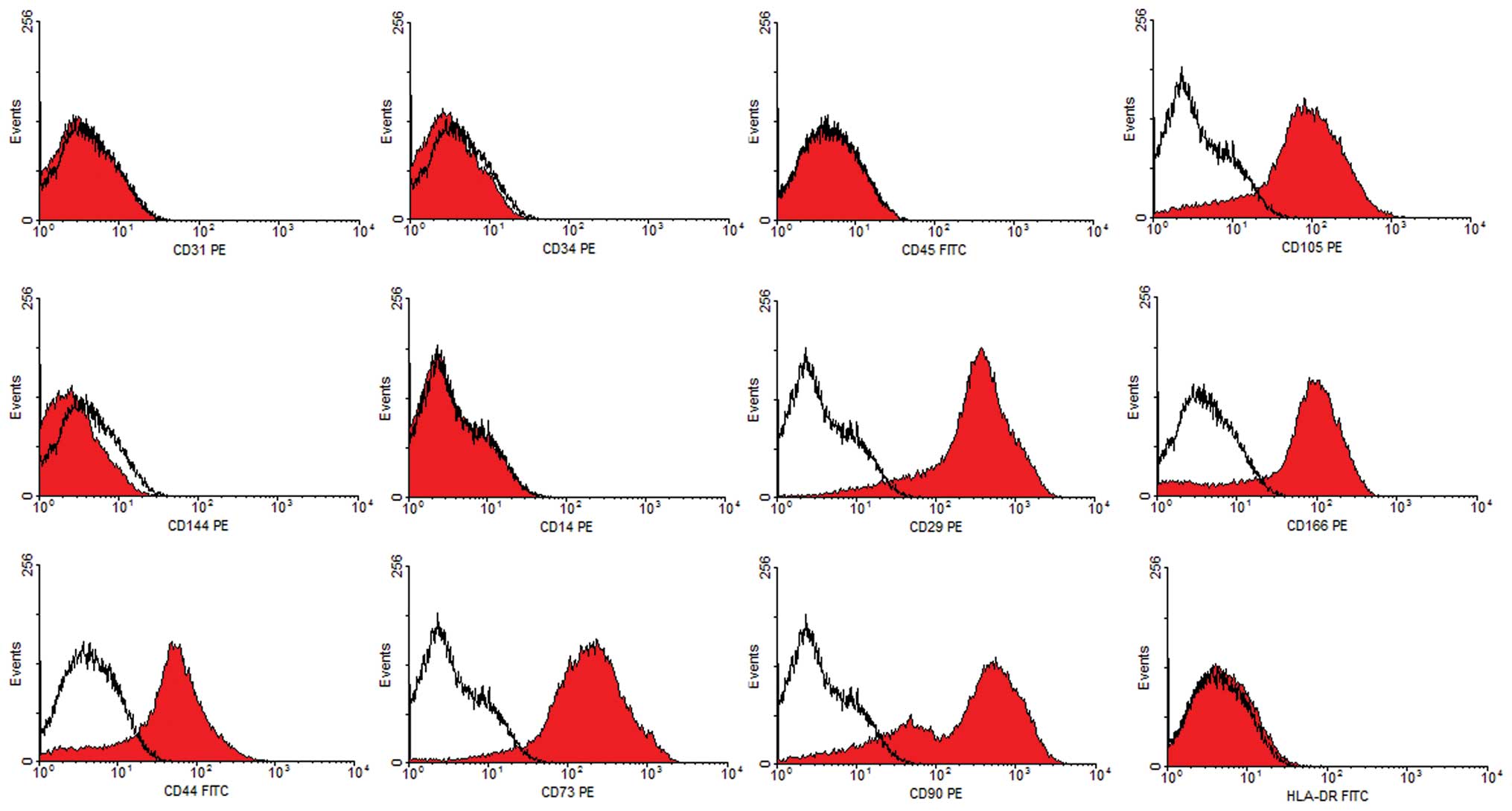 | Figure 2Surface antigens of MSC-like cells
from renal AML. Representative FACS analysis demonstrated
positivity for MSC markers CD29, CD44, CD73, CD90, CD105 and CD166,
but negativity for CD14, CD31, CD34, CD45, CD144 and HLA-DR. Dark
lines indicate the isotypic control. FITC, fluorescein
isothiocyanate; PE, phycoerythrin. MSC, mesenchymal stem cells;
AML, angiomyolipoma. |
Induction of multilineage mesenchymal
cell differentiation
To investigate the differentiation potential of
these MSC-like cells from AML tissues, we cultured cells under
conditions that favored osteogenic or adipogenic differentiation.
When cultured in an adipogenic differentiation medium for 4 days,
preadipocytes with bright lipid droplets appeared. The lipid
vacuoles became larger following further induction and were clearly
visible without staining under a phase microscope. Following
Oil-Red-O staining, the lipid nature of these red vacuoles was
evident (Fig. 3). When cultured in
osteogenic differentiation medium for 2 weeks, MSC-like cells
differentiated into osteocytes, which stained positive for ALP
(Fig. 3). Non-treated control cells
revealed no significant spontaneous adipocyte or osteoblast
formation.
Discussion
In this study, we successfully isolated adherent
fibroblastoid cells from 6 cases of classic renal AML and
investigated their biological characteristics. These AML-derived
cells share a panel of surface antigens similar to MSCs isolated
from other tissues, and are functionally able to differentiate into
mesenchymal cells, including osteocytes and adipocytes.
MSCs have been isolated from various tumors, and
have been suggested to contribute in human and mouse cancer models.
Spontaneous malignant transformation has been reported in cultured
murine MSCs, which transforms into osteosarcoma or fibrosarcoma.
Malignant transformations have also been reported in long-term
cultured human MSCs and are considered to play a key role in
age-related tumors (12–15). Ewing’s sarcoma was recently reported
to be derived from MSCs, and cells isolated from this type of tumor
tissue are able to differentiate along the adipogenic and
osteogenic lineages (16). It is
also reported that Wilms tumor cell lines are highly similar to
human MSCs and express the MSC-specific surface proteins CD105,
CD90 and CD73. The stem cell-like nature of the tumor cells is
further supported by their adipogenic, chondrogenic and osteogenic
differentiation potentials (17).
Although MSCs may be the cell origin of malignant
tumors (18), MSCs in benign tumors
have not been greatly studied. Additionally, no study has addressed
the possible presence of stem cells in renal AML. As a member of
the perivascular epithelioid cell tumors (PECOMAS) family, renal
AML tumors are recognized as clonal neoplasms of the perivascular
epithelial cells, which are mainly pericytes (19,20).
It has also been demonstrated that MSC-like cells originate from
pericytes surrounding capillaries and microvessels. These cells,
either freshly isolated or cultured over a long time, are
indistinguishable from classic MSCs (21,22).
Previous studies have demonstrated the similarities between MSCs
and pericytes; however, neither cell sorting nor stringent cell
characterization has been performed to further support a
correlation between these cell types, and the term pericyte has
been used in its anatomic literal sense without any functional
connotation (23). These pioneering
studies suggest a perivascular origin for MSCs and other adult
progenitor cells.
In the present study, the AML-derived cells
demonstrated fibroblastoid morphology, plastic adherence and
continuous expansion in vitro, which lead us to examine
their MSC nature. Their ability to differentiate into adipocytes
and osteoblasts when cultured in the appropriate differentiation
medium, and their specific cell-surface phenotype labeling proved
that they were MSC-like cells. Identification of MSCs in the renal
AML tissue further supports the hypothesis that MSCs may be an
important component of the tumor, and their presence may contribute
to the development and formation of renal AML.
Several questions remain to be answered in future
studies. Firstly, the source of MSCs in AML is unclear. Due to the
similarities between AML MSC-like cells and bone marrow MSCs, it is
reasonable to speculate that MSCs in renal AML may migrate from
bone marrow and may have an intimate association with the formation
of AML. Previous studies indicate that the MSC compartment extends
throughout the body postnatally as a result of its perivascular
location (7). Secondly, the
abundance and localization of these cells in AML tissues has not
yet been explored. Although cultured MSC-like cells have been
functionally well-characterized, the identity and localization of
the native MSCs ancestor in vivo remains elusive. Thirdly,
it is unknown whether these MSC-like cells are likely to
differentiate into the triphasic histology in AML, although they
are bipotent in the in vitro study. It is also not
elucidated whether these MSC-like cells, as well as their
decedents, constitute the entity of the AML tumor. In our in
vivo study, MSC-like cells only formed tumors within 3 months
of grafting into the nude mice (data not shown). As a benign tumor,
classic renal AML is associated with a slow and consistent growth
rate (0.088 cm/year) (24). This
biological characteristic explains the loss of the tumorigenic
ability of these cells.
In conclusion, we present the first study of the
existence of MSC-like cells isolated from fresh classic renal AML
tissues. Cells derived from these tumors bear MSC markers and may
be induced to differentiate along at least two mesenchymal
lineages. Isolation and identification of MSC-like cells
contributes to our knowledge of classic renal AML and suggests an
MSC origin of renal AML. Targeting mesenchymal progenitors may open
new opportunities for designing alternative therapeutic strategies
against renal AML.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (Grant No. 30600613).
References
|
1
|
Lim SD, Stallcup W, Lefkove B,
Govindarajan B, Au KS, Northrup H, et al: Expression of the neural
stem cell markers NG2 and L1 in human angiomyolipoma: are
angiomyolipomas neoplasms of stem cells? Mol Med. 13:160–165.
2007.PubMed/NCBI
|
|
2
|
Bonetti F, Pea M, Martignoni G, Doglioni
C, Zamboni G, Capelli P, et al: Clear cell (‘sugar’) tumor of the
lung is a lesion strictly related to angiomyolipoma - the concept
of a family of lesions characterized by the presence of the
perivascular epithelioid cells (PEC). Pathology. 26:230–236.
1994.
|
|
3
|
Barnard M and Lajoie G: Angiomyolipoma:
immunohistochemical and ultrastructural study of 14 cases.
Ultrastruct Pathol. 25:21–29. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cao H, Xu W, Qian H, Zhu W, Yan Y, Zhou H,
et al: Mesenchymal stem cell-like cells derived from human gastric
cancer tissues. Cancer Lett. 274:61–71. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bussolati B, Bruno S, Grange C, Ferrando U
and Camussi G: Identification of a tumor-initiating stem cell
population in human renal carcinomas. FASEB J. 22:3696–3705. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gupta S, Verfaillie C, Chmielewski D, Kren
S, Eidman K, Connaire J, et al: Isolation and characterization of
kidney-derived stem cells. J Am Soc Nephrol. 17:3028–3040. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
da Silva Meirelles L, Chagastelles PC and
Nardi NB: Mesenchymal stem cells reside in virtually all post-natal
organs and tissues. J Cell Sci. 119:2204–2213. 2006.PubMed/NCBI
|
|
8
|
Plotkin MD and Goligorsky MS: Mesenchymal
cells from adult kidney support angiogenesis and differentiate into
multiple interstitial cell types including erythropoietin-producing
fibroblasts. Am J Physiol Renal Physiol. 291:F902–F912. 2006.
View Article : Google Scholar
|
|
9
|
Humphreys BD and Bonventre JV: Mesenchymal
stem cells in acute kidney injury. Annu Rev Med. 59:311–325. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ooi SM, Vivian JB and Cohen RJ: The use of
the Ki-67 marker in the pathological diagnosis of the epithelioid
variant of renal angiomyolipoma. Int Urol Nephrol. 41:559–565.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sun S, Guo Z, Xiao X, Liu B, Liu X, Tang
PH, et al: Isolation of mouse marrow mesenchymal progenitors by a
novel and reliable method. Stem Cells. 21:527–535. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aractingi S, Kanitakis J, Euvrard S, Le
Danff C, Peguillet I, Khosrotehrani K, et al: Skin carcinoma
arising from donor cells in a kidney transplant recipient. Cancer
Res. 65:1755–1760. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Barozzi P, Luppi M, Facchetti F, Mecucci
C, Alù M, Sarid R, et al: Post-transplant Kaposi sarcoma originates
from the seeding of donor-derived progenitors. Nat Med. 9:554–561.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Houghton J, Stoicov C, Nomura S, Rogers
AB, Carlson J, Li H, et al: Gastric cancer originating from bone
marrow-derived cells. Science. 306:1568–1571. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li H, Fan X, Kovi RC, Jo Y, Moquin B, Konz
R, et al: Spontaneous expression of embryonic factors and p53 point
mutations in aged mesenchymal stem cells: a model of age-related
tumorigenesis in mice. Cancer Res. 67:10889–10898. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tirode F, Laud-Duval K, Prieur A, Delorme
B, Charbord P and Delattre O: Mesenchymal stem cell features of
Ewing tumors. Cancer Cell. 11:421–429. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Royer-Pokora B, Busch M, Beier M, Duhme C,
de Torres C, Mora J, et al: Wilms tumor cells with WT1 mutations
have characteristic features of mesenchymal stem cells and express
molecular markers of paraxial mesoderm. Hum Mol Genet.
19:1651–1668. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li N, Yang R, Zhang W, Dorfman H, Rao P
and Gorlick R: Genetically transforming human mesenchymal stem
cells to sarcomas: changes in cellular phenotype and multilineage
differentiation potential. Cancer. 115:4795–4806. 2009. View Article : Google Scholar
|
|
19
|
Varma S, Gupta S, Talwar J, Forte F and
Dhar M: Renal epithelioid angiomyolipoma: a malignant disease. J
Nephrol. 24:18–22. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Paradis V, Laurendeau I, Vieillefond A,
Blanchet P, Eschwege P, Benoît G, et al: Clonal analysis of renal
sporadic angiomyolipomas. Hum Pathol. 29:1063–1067. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Crisan M, Yap S, Casteilla L, Chen CW,
Corselli M, Park TS, et al: A perivascular origin for mesenchymal
stem cells in multiple human organs. Cell Stem Cell. 3:301–313.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Crisan M, Chen CW, Corselli M, Andriolo G,
Lazzari L and Péault B: Perivascular multipotent progenitor cells
in human organs. Ann NY Acad Sci. 1176:118–123. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Corselli M, Chen CW, Crisan M, Lazzari L
and Péault B: Perivascular ancestors of adult multipotent stem
cells. Arterioscler Thromb Vasc Biol. 30:1104–1109. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mues AC, Palacios JM, Haramis G, Casazza
C, Badani K, Gupta M, et al: Contemporary experience in the
management of angiomyolipoma. J Endourol. 24:1883–1886. 2010.
View Article : Google Scholar : PubMed/NCBI
|