Introduction
Squamous cell carcinoma (SCC) is the most common
malignant tumor of the cervix, comprising 70–80% of cervical
malignancies. Cervical SCC generally invades directly into the
uterine wall with or without parametrial involvement. Cervical SCC
that spreads superficially to the inner surface of the uterus and
replaces the endometrium with carcinoma cells is called superficial
spreading SCC and has been extremely rarely reported (1–4). In
the present study, we report two additional cases of superficial
spreading SCC of the cervix involving the endometrium and discuss
the possible molecular mechanism of this unusual spreading form of
cervical SCC. This study was approved by the Ethics Committee of
Shiga, University of Medical Science, Shiga, Japan. Consent was
obtained from the patients.
Patients and methods
Case reports
Case 1
A 64-year-old Japanese female presented with
persistent post-menopausal vaginal bleeding. Cervical biopsy at a
gynecological clinic revealed invasive SCC and the patient was
referred to Shiga University of Medical Science Hospital. The
patient was pre-operatively classified as clinical stage IIA1 since
vaginal examination revealed vaginal involvement of the cervical
cancer and the tumor size was 1 cm. The patient underwent total
hysterectomy and bilateral salpingo-oophorectomy.
The post-operative course has been uneventful, and
the patient has been free from tumor recurrence or metastasis for
10 months.
Case 2
A 59-year-old Japanese female presented with
persistent post-menopausal vaginal bleeding. Cervical smear at a
gynecological clinic revealed presence of a high-grade squamous
intraepithelial lesion and the patient was referred to Shiga
University of Medical Science Hospital. Magnetic resonance imaging
revealed a cervical tumor, measuring ∼4x4 cm, directly invading
into the parametrium. Histopathological study of the cervical
biopsy specimen showed invasive SCC. The patient was
pre-operatively classified as clinical stage IIB and underwent
total hysterectomy and bilateral salpingooophorectomy.
The post-operative course has been uneventful, and
the patient has been free from tumor recurrence or metastasis for 6
months.
Materials and methods
The formalin-fixed, paraffin-embedded tissue blocks
of the resected specimens were cut into 3-μm-thick sections,
deparaffinized and rehydrated. Each section was stained with
hematoxylin and eosin and then used for immunostaining.
Immunohistochemical analyses were performed using an autostainer
(XT system Benchmark, Ventana Medical System, Tucson, AZ, USA)
according to the manufacturer’s instructions. A mouse monoclonal
antibody against CD138 (syndecan-1; B-A38, Cell Marque, Rocklin,
CA, USA) was used.
Results
Case 1
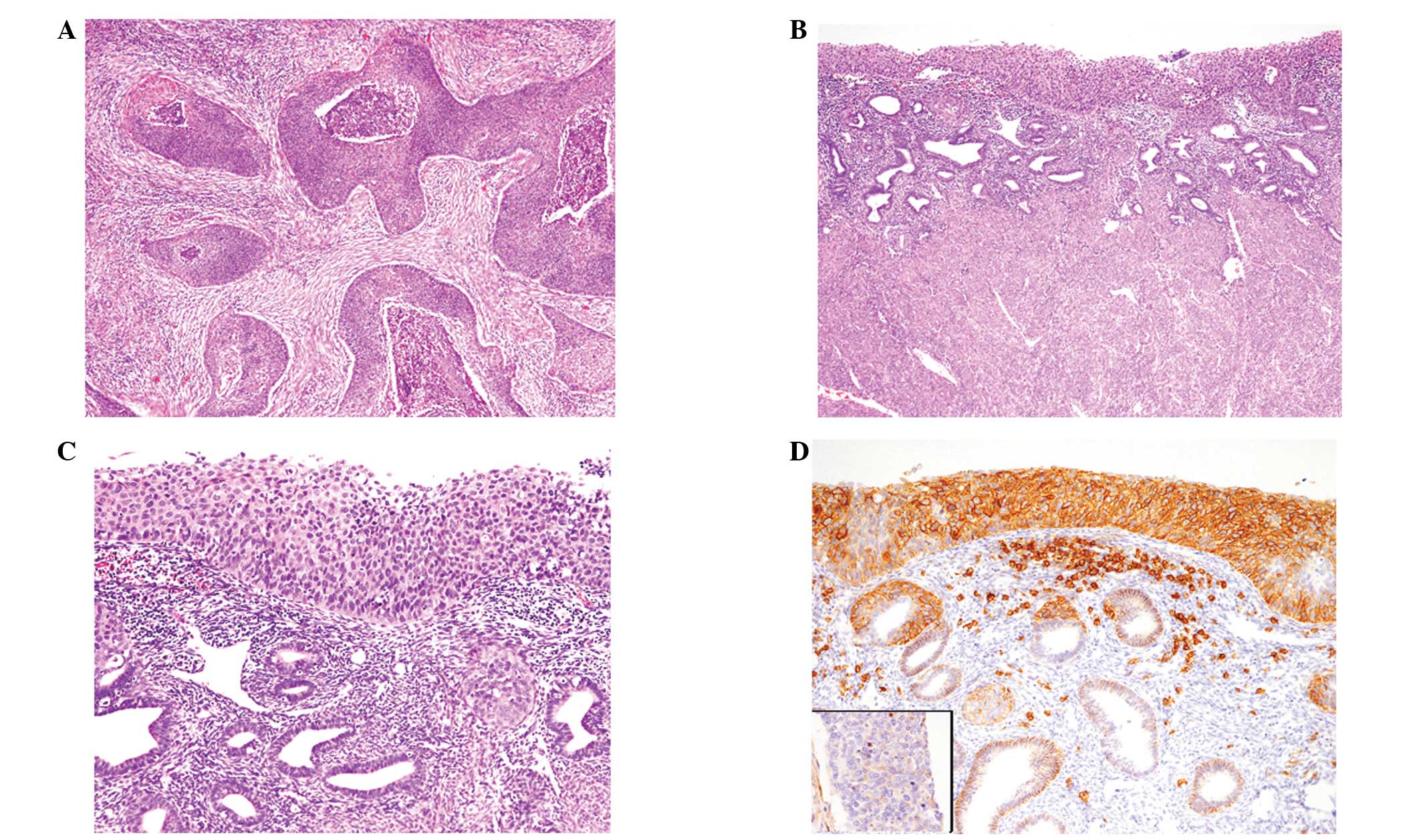
Proliferation of atypical squamous cells with large
oval nuclei and a single nucleolus was observed in the entire
squamous epithelium of the cervix and mitotic figures were noted in
the upper portion of the squamous epithelium. Most of the cervical
tumor was composed of this intraepithelial lesion with glandular
involvement, however, focal superficial invasive growth was noted
(Fig. 1A). Keratinization was not
evident. Intraepithelial involvement and superficial invasive
growth of carcinoma cells in the vagina were also observed.
According to these findings, a diagnosis of non-keratinizing SCC of
the cervix (pTIIA1) was made.
The notable finding of the present case was that
atypical squamous cells were extending and replacing the
endometrium directly from the cervix (Fig. 1B). Glandular involvement of atrophic
endometrial glands was observed (Fig.
1B and C), but no invasive growth was noted in the endometrium.
Bilateral tubes and ovaries were free from carcinoma spread. In
addition, no lymph node metastasis was detected.
Immunohistochemically, all the carcinoma cells that
were spreading superficially in the endometrium (Fig. 1D), in the mildly invasive lesion of
the cervix and vagina (Fig. 1D,
inset) and in the intraepithelial lesions of the cervix and vagina
were diffusely and strongly positive for CD138.
Case 2
Invasive neoplastic growth composed of irregular
islands or large nests was observed in the entire cervix (Fig. 2A). Neoplastic cells had large
slightly eosinophilic cytoplasm and large oval nuclei with a
conspicuous nucleolus. Intercellular bridges and individual cell
keratinization were observed, however, keratinizaion was not
evident and keratin pearls were not observed. The tumor had
directly invaded into the parametrium, but not into the vagina.
Therefore, a diagnosis of non-keratinizing SCC of the cervix
(pTIIB) was made.
Neoplastic squamous cells were extending and
replacing the endometrium directly from the cervix (Fig. 2B). Glandular involvement of the
atrophic endometrial glands was observed (Fig. 2B and C), but no myometrial invasion
was noted. The entire endometrium was replaced by carcinoma cells,
however, bilateral tubes and ovaries were free from carcinoma
spread. In addition, no lymph node metastasis was detected.
Immunohistochemical analyses revealed that CD138 was
strongly and diffusely expressed in the neoplastic squamous cells
superficially spreading in the endometrium (Fig. 2D) and the intraepithelial lesion of
the cervix, however CD138 expression was hardly observed in the
neoplastic squamous cells of the invasive lesion of the cervix
(Fig. 2D, inset).
Discussion
In the present study, we described two additional
cases of superficial spreading SCC of the cervix involving the
endometrium. The clinicopathological features of the 26 previously
reported cases of superficial spreading SCC of the cervix and the
two present cases are as follows: i) the age of all patients was
over 50 years (average, 61.9 years; range, 52–78 years; information
on the patients’ age was available in 14 cases); ii) the most
common clinical presentation was genital bleeding; and iii)
Fallopian tube with or without ovarian involvement was present in 9
cases (1–4).
Kushima et al reported five cases of
superficial spreading SCC of the cervix involving the endometrium
and/or Fallopian tube and ovary (3). They concluded that most tumors of this
type were monoclonal neoplasia originating from the cervical mucosa
with subsequent superficial spreading to the upper genital mucosa
according to loss of heterozygosity analyses (3). The two present cases were also thought
to be of cervical mucosa origin that had spread superficially in
the endometrium.
The molecular mechanism of the superficial spreading
of carcinoma cells is not well understood. CD138, also known as
syndecan-1, is a cell-surface heparan sulfate proteoglycan and
participates in cell-cell and cell-extracellular matrix
interactions (5). CD138 is
expressed in normal epithelial cells, including stratified squamous
epithelium, as well as plasma cells. A correlation between CD138
expression and carcinogenesis has been investigated in various
organs. Increased expression of CD138 has been reported in
endometrial and ovarian carcinomas (6,7). By
contrast, decreased expression of CD138 has been reported to
correlate with tumor invasion and progression of cervical cancer
(8–10). Shinyo et al reported that the
loss of CD138 expression is an early event in cervical
carcinogenesis, as this molecule is strongly expressed in cervical
intraepithelial neoplasia (CIN) I and II. However, its expression
is reduced in CIN III, and CD138 expression in microinvasive and
invasive SCC is lower compared with CIN III (9). In the two present cases, CD138 was
strongly expressed in the intraepithelial lesions of the cervix as
well as in the cells that were superficially spreading in the
endometrium. Therefore, the findings of the present cases suggest
that CD138 expression in carcinoma cells may participate in
superficial spreading by regulating cell-cell interactions and, by
contrast, carcinoma cells lacking CD138 expression show overt
invasive growth.
References
|
1
|
Gungor T, Altinkaya SO, Ozat M, Akbay S
and Mollamahmutoglu L: Unusual form of superficial spreading
squamous cell carcinoma of cervix involving the endometrium,
bilateral tubes and ovaries: a case report with literature review.
Arch Gynecol Obstet. 283:323–327. 2011. View Article : Google Scholar
|
|
2
|
Tan GC, Isa MR, Ng SP and Jamil MA:
Unusual form of superficial spreading microinvasive squamous cell
carcinoma of uterine cervix involving the endometrium of uterus. J
Obstet Gynaecol Res. 30:363–367. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kushima M, Fujii H, Murakami K, et al:
Simultaneous squamous cell carcinomas of the uterine cervix and
upper genital tract: loss of heterozygosity analysis demonstrates
clonal neoplasms of cervical origin. Int J Gynecol Pathol.
20:353–358. 2001. View Article : Google Scholar
|
|
4
|
Pins MR, Young RH, Crum CP, Leach IH and
Scully RE: Cervical squamous cell carcinoma in situ with
intraepithelial extension to the upper genital tract and invasion
of tubes and ovaries: report of a case with human papilloma virus
analysis. Int J Gynecol Pathol. 16:272–278. 1997. View Article : Google Scholar
|
|
5
|
Bernfield M, Götte M, Park PW, et al:
Functions of cell surface heparan sulfate proteoglycans. Ann Rev
Biochem. 68:729–777. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Oh JH, Kim JH, Ahn HJ, et al: Syndecan-1
enhances the endometrial cancer invasion by modulating matrix
metalloproteinase-9 expression through nuclear factor kappa B.
Gynecol Oncol. 114:509–515. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Davies EJ, Blackhall FH, Shanks JH, et al:
Distribution and clinical significance of heparan sulfate
proteoglycans in ovarian cancer. Clin Cancer Res. 10:5178–5186.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Numa F, Hirabayashi K, Kawasaki K, et al:
Syndecan-1 expression in cancer of the uterine cervix: association
with lymph node metastasis. Int J Oncol. 20:39–43. 2002.PubMed/NCBI
|
|
9
|
Shinyo Y, Kodama J, Hasengaowa, Kusumoto T
and Hiramatsu Y: Loss of cell-surface heparan sulfate expression in
both cervical intraepithelial neoplasm and invasive cervical
cancer. Gynecol Oncol. 96:776–783. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim YI, Lee A, Lee BH and Kim SY:
Prognostic significance of syndecan-1 expression in cervical
cancers. J Gynecol Oncol. 22:161–167. 2001. View Article : Google Scholar : PubMed/NCBI
|