Introduction
Thymic neuroendocrine carcinomas (NECs) are rare and
have been estimated to account for 2–4% of all anterior mediastinal
tumors (1). Local and distal
metastases frequently develop following surgical excision of these
tumors (2–4). A previous study by Fukai et al
showed that recurrence occurred 4–99 months after surgery (3) and recurrence after as long as 9 years
has been described (5,6). However, to the best of our knowledge,
no studies have discussed the development of recurrence >20
years after total excision. Although the optimal therapeutic
modality for the treatment of recurrent disease has not been
determined, more aggressive treatment, including re-excision of
recurrent tumors, may be required to reduce the incidence of local
recurrence and distant metastasis and to improve survival. The
current study presents a rare case of a recurrent neuroendocrine
tumor in the thymus developing 24 years after total excision.
Written informed consent was obtained from the patient.
Case report
Clinical presentation
A 77-year-old male was referred for an evaluation of
an acute onset of chest pain. The patient had undergone a
thymectomy via a median sternotomy for an anterior mediastinal
tumor 24 years previously. The pathological diagnosis was of a
World Health Organization (WHO) type B3 thymoma classified as
pathological stage I due to the absence of capsular invasion
(Masaoka classification). Regular medical check-ups had been
performed twice a year for 20 years after the surgery and had been
completed without evidence of recurrence. However, ∼3 years after
the final check-up, a sudden onset of left-sided chest pain was
reported and the patient was referred again. Laboratory
examinations revealed elevated C-reactive protein levels (3.53
mg/dl), but no other abnormal levels of any tumor markers,
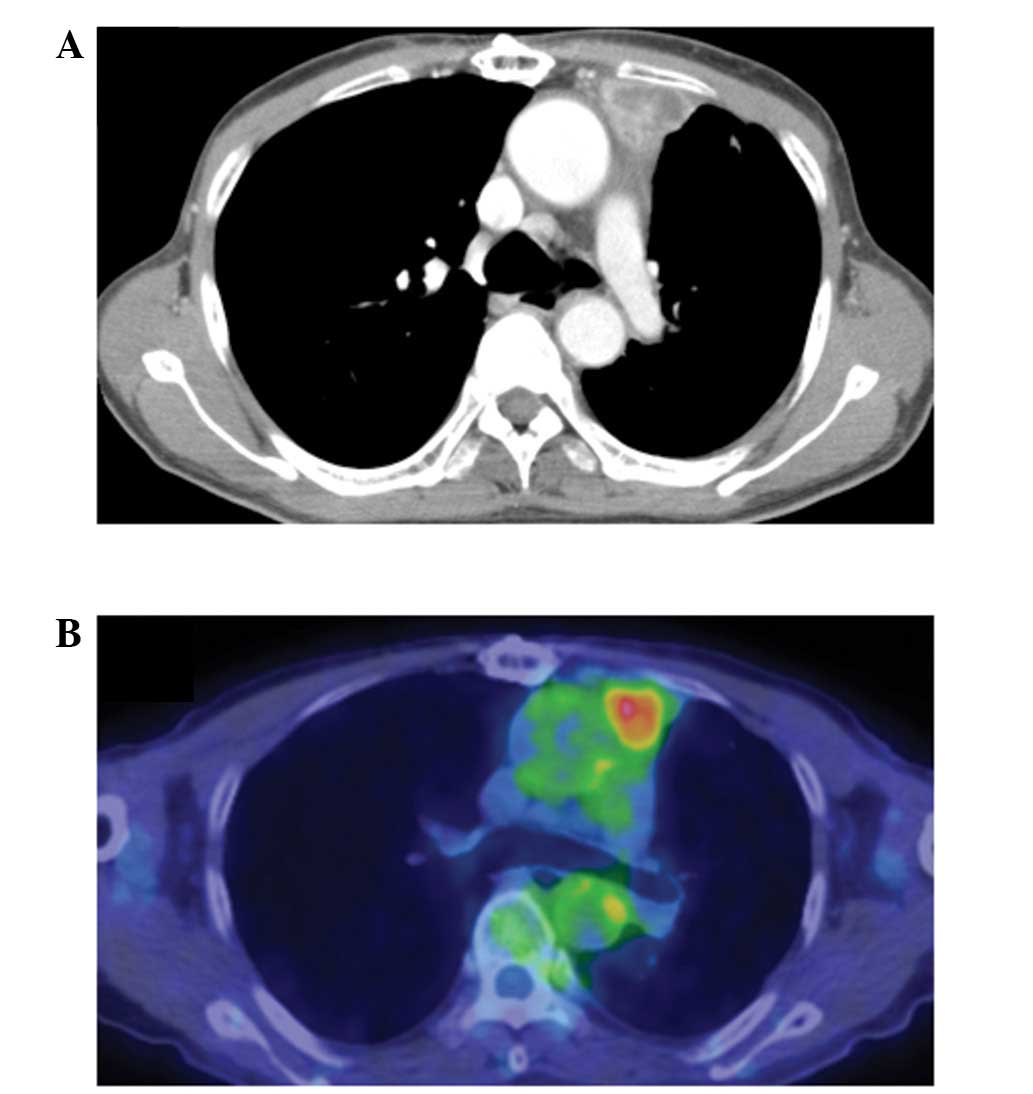
including neuron specific enolase. Computed tomography (CT)
revealed an irregularly enhanced tumor in the anterior mediastinum
with a maximum size of ∼3 cm (Fig.
1A). Positron emission tomography/CT scans revealed increased
18F-fluorodeoxyglucose uptake in the mass (maximum
standard uptake value, 3.35), although no abnormal uptake
indicative of distant metastases was observed (Fig. 1B).
Surgery
Surgery was performed under the diagnosis of a
suspected recurrent thymoma. A posterolateral thoracotomy was
performed under video-assisted thoracoscopy. Severe adhesions were
observed around the tumor, which appeared to have invaded the left
upper lung and pericardium, while no pleural dissemination was
observed. Therefore, the tumor was extirpated in combination with
partial resection of the left upper lung and pericardium, and the
excised pericardium was repaired using a polytetrafluoroethylene
sheet. The tumor was found to be a yellowish-white solid mass
invading the lung (Fig. 2).
Histopathology
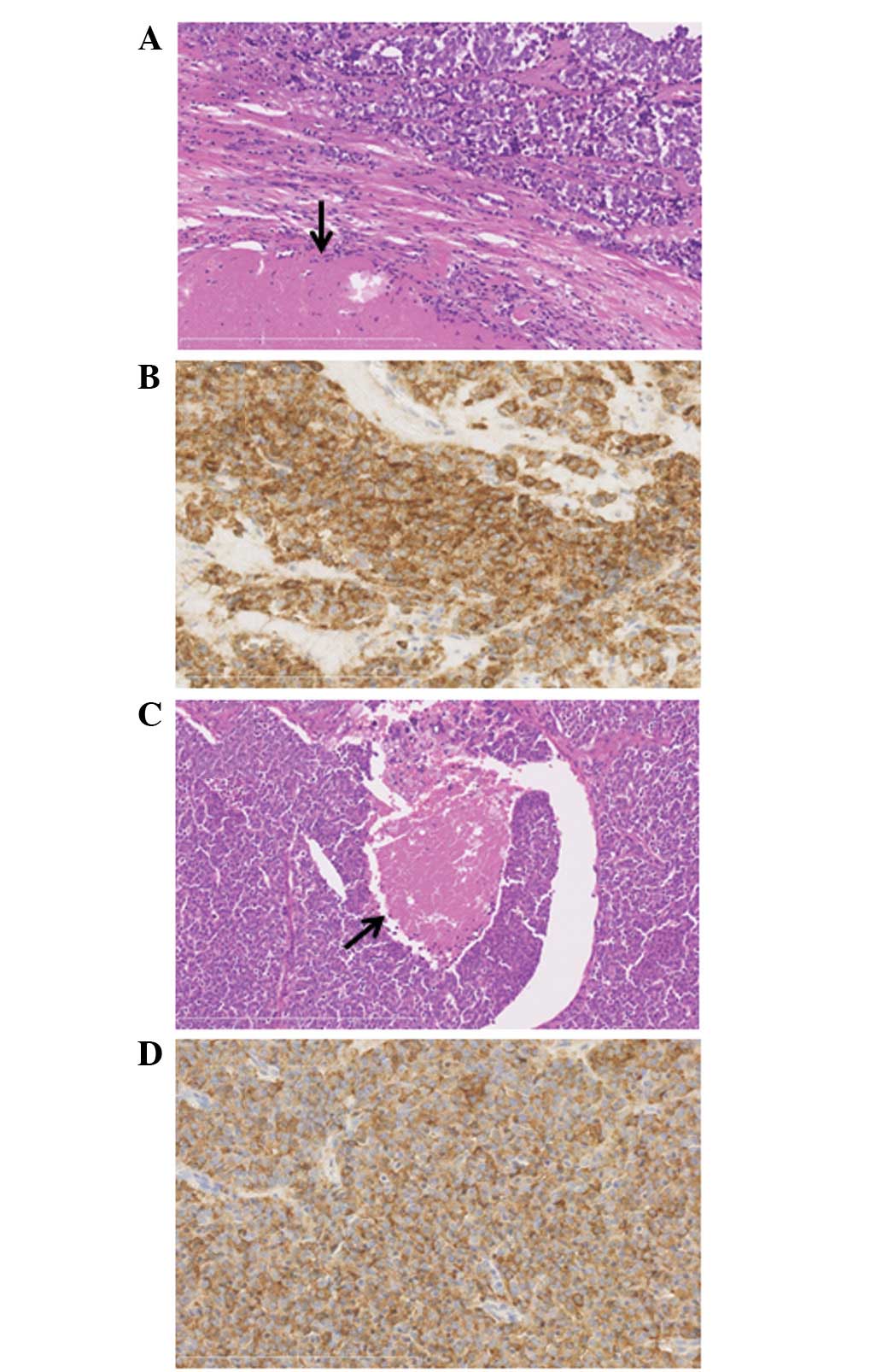
Histopathologically, atypical carcinoid cells were
observed to be arranged in sheets or small nested patterns
accompanied by necrosis and lymphoid infiltration invading the
surrounding adipose tissue and lungs, while extremely few mitotic
cells were observed (Fig. 3A). An
immunohistochemical analysis revealed that the tumor exhibited
immunoreactivity to neuroendocrine markers, including chromogranin
A (Fig. 3B). Based on these
observations, the tumor was diagnosed as a well-differentiated NEC
(atypical carcinoid, due to the presence of necrosis). The surgical
margin of the lung was affected by the cancer cells.
Retrospectively, the specimen that had been excised 24 years
previously was re-examined and was reported to exhibit the same
histology, HE results and immunoreactivity to the neuroendocrine
markers as the present tumor (Figs. 3C
and D).
There were no post-operative complications. Although
the surgical margins were positive for cancer cells, no medical
intervention was administered due to the patient’s age and the
invasiveness of radiation and chemotherapy.
Discussion
Thymic NEC is a rare type of neoplasm arising in the
thymus, accounting for 2–4% of all anterior mediastinal tumors
(1). This form of neoplasm has long
been confused with thymoma, although Rosai and Higa described
thymic NEC as a separate entity from thymoma in 1972 (7). Thymic NECs are predominantly or
exclusively composed of neuroendocrine cells and must be
distinguished from other typical thymic carcinomas with small
numbers of neuroendocrine cells (8). Thymic NECs are divided into two
groups, well- and poorly-differentiated, depending on the degree of
tumor differentiation. The former group contains typical and
atypical carcinoids classified according to the presence of
necrosis and/or the number of mitotic cells, while the latter group
includes large cell NEC and small cell carcinoma. This
categorization is significant in that the prognosis of a
well-differentiated NEC is improved compared with that of a
poorly-differentiated NEC (8). In
the present case, well-differentiated neuroendocrine cells were
accompanied by necrotic components.
Local recurrence and distant metastasis develops
frequently following surgical excision of thymic NECs (2–4). Wang
et al previously reported that local recurrence or distant
metastasis developed 15–60 months after surgery in 4/5 (80%)
patients. In these cases, the sites of relapse included the chest
wall, regional lymph nodes, bones and lungs (2). In addition, Fukai et al
reported that distant metastases developed in 10/13 (76.9%) of
patients who underwent total tumor resection, despite the absence
of local recurrence (3). The study
also reported intervals of 4–99 months between surgery and
recurrence, comparable to that reported by Tiffet et al
(22–83 months) (4). A study by
Economopoulos et al identified recurrence in one case 9
years after surgery (5). However,
to the best of our knowledge, there are no reports of any cases of
recurrent thymic NEC relapsing 10–20 years after surgery.
Therefore, the present case involves the longest period of time
between the recurrence of thymic NEC and surgery. The optimal
therapeutic modality for the treatment of recurrent disease has not
been determined. However, due to the aggressive nature of tumors
prone to recur or metastasize even following total excision, more
aggressive treatments, including routine adjuvant chemotherapy and
re-excision of recurrent tumors, as performed in the present case,
may be required to reduce the incidence of local recurrence and
distant metastasis, and therefore improve survival.
In conclusion, this study presents a case of a
surgically-excised thymic NEC recurring >20 years after the
initial excision. Thoracic oncologists must be aware that thymic
NECs may recur ≥20 years after surgical treatment.
Acknowledgements
The authors would like to thank Brian
Quinn for his critical comments on the manuscript. This manuscript
has been presented as a poster at the Third International Thymic
Malignancy Interest Group (ITMIG) Annual Meeting held in 2012.
References
|
1.
|
Duh QY, Hybarger CP, Geist R, Gamsu G,
Goodman PC, Gooding GA and Clark OH: Carcinoids associated with
multiple endocrine neoplasia syndromes. Am J Surg. 154:142–148.
1987. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Wang DY, Chang DB, Kuo SH, Yang PC, Lee
YC, Hsu HC and Luh KT: Carcinoid tumours of the thymus. Thorax.
49:357–360. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Fukai I, Masaoka A, Fujii Y, Yamakawa Y,
Yokoyama T, Murase T and Eimoto T: Thymic neuroendocrine tumor
(thymic carcinoid): a clinicopathologic study in 15 patients. Ann
Thorac Surg. 67:208–211. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Tiffet O, Nicholson AG, Ladas G, Sheppard
MN and Goldstraw P: A clinicopathologic study of 12 neuroendocrine
tumors arising in the thymus. Chest. 124:141–146. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Economopoulos GC, Lewis JW Jr, Lee MW and
Silverman NA: Carcinoid tumors of the thymus. Ann Thorac Surg.
50:58–61. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
de Montpréville VT, Macchiarini P and
Dulmet E: Thymic neuroendocrine carcinoma (carcinoid): a
clinicopathologic study of fourteen cases. J Thorac Cardiovasc
Surg. 111:134–141. 1996.PubMed/NCBI
|
|
7.
|
Rosai J and Higa E: Mediastinal endocrine
neoplasm, of probable thymic origin, related to carcinoid tumor.
Clinicopathologic study of 8 cases. Cancer. 29:1061–1074. 1972.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Rosai J and Sobin LH: Definitions and
explanatory notes. World Health Organization International
Histological Classification of Tumors: Histological Typing of
Tumours of the Thymus. 2nd edition. Springer Verlag;
Berlin-Heildelberg: pp. 15–18. 1999
|