Introduction
Although small cell lung cancer (SCLC) is one of the
most common histological types of primary lung cancer,
endobronchial extension is extremely rare (1,2). A
clinical differential diagnosis of endobronchial lesions may
include a variety of conditions, such as non-malignant tumors,
primary lung carcinoma other than adenocarcinoma and endobronchial
metastasis of carcinoma from extrapulmonary organs (3–8). The
current study presents the case of a patient with SCLC and
endobronchial growth. Written informed consent was obtained from
the patient.
Case report
Patient presentation
A 68-year-old male was referred to the Mito Medical
Center (University of Tsukuba, Mito, Japan) following a three-month
history of hoarseness. Upon admission, laboratory tests revealed
that the patient had hemoglobin levels of 12.5 g/dl, a hematocrit
of 37.2% and a C-reactive protein count of 0.64 mg/dl. The serum
levels of neuron-specific enolase were elevated to 156.7 ng/ml.
X-ray and computed tomography (CT) scans of the chest revealed an
ill-defined mass in the upper lobe of the right lung, with
ipsilateral mediastinal lymph node swelling (Fig. 1). A bronchoscopy revealed a
well-circumscribed movable tumor located at the right B3 bronchus.
The tumor obstructed ∼90% of the lumen and the scope was not able
to pass through this region (Fig.
2). Using the bronchoscopy, the whole of the mobile section of
the endobronchial tumor was removed easily. Following the removal
of the endobronchial tumor, the distal bronchus demonstrated
narrowing by a sub-mucosal tumor.
Pathological analysis
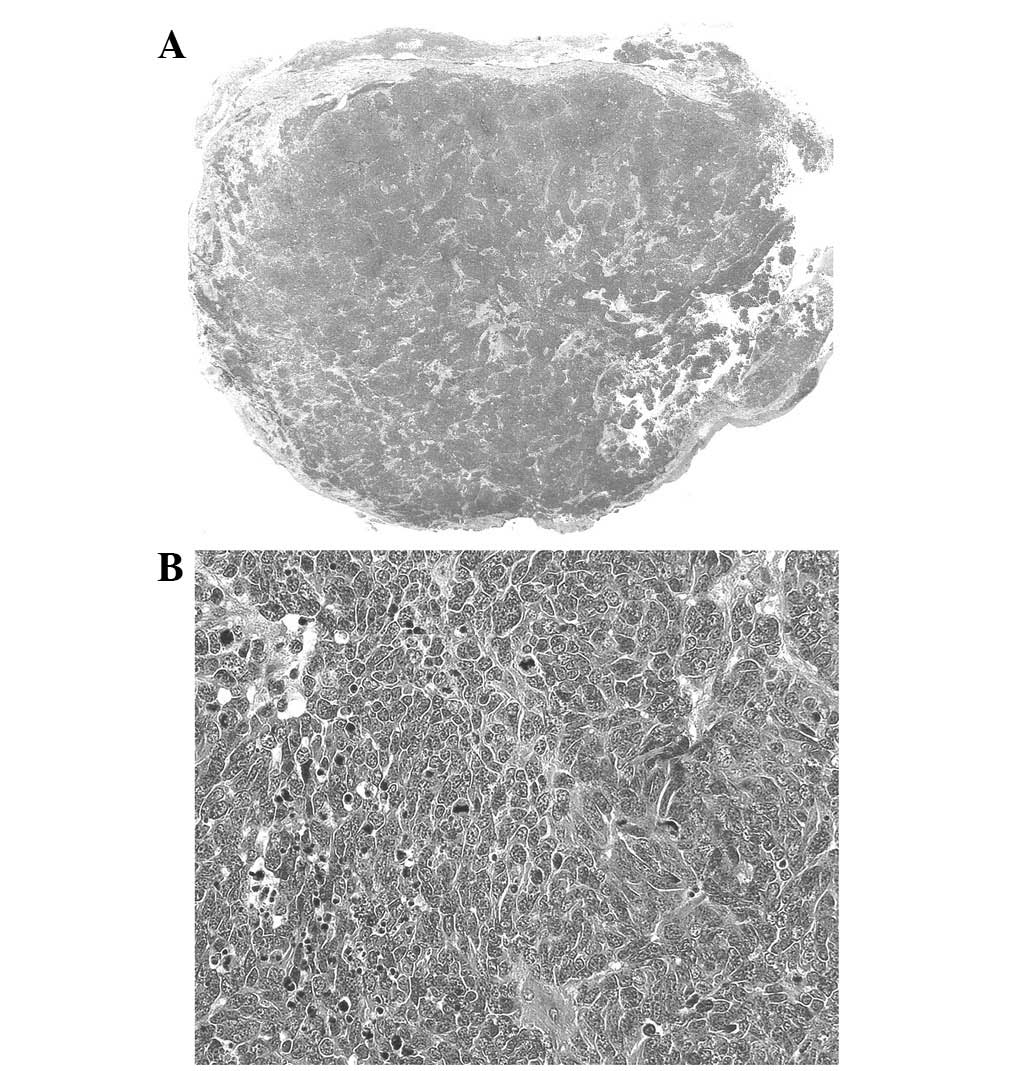
The pathological examination of the tumor was
consistent with a diagnosis of SCLC (Fig. 3). An immunohistochemical examination
revealed positive staining for CD-56 (Fig. 4A) and chromogranin (Fig. 4B).
Clinical course
Brain magnetic resonance imaging, abdominal
ultrasonography and bone scintigraphy scans did not identify a
malignancy. The tumor was diagnosed as limited-disease SCLC. The
patient received chemoradiotherapy containing four courses of
cisplatin (80 mg/m2, day 1) and etoposide (100
mg/m2, days 1–3), which resulted in a partial response.
At six months after the initial therapy, the patient exhibited
local recurrence. Despite the second to fourth lines of
chemotherapy being less effective, tumor growth at the primary site
was not as rapid as previously observed and no distant metastasis
was identified. However, 22 months after the initiation of the
first course of chemotherapy, the patient succumbed to SCLC.
Discussion
Radiographical manifestations of endobronchial
lesions are considerably variable. Lobar or segmental atelectasis
and pneumonic infiltration are commonly observed. The radiological
differential diagnosis of an endobronchial mass lesion includes
non-malignant tumors, endobronchial metastasis of carcinoma from
extrapulmonary organs and primary lung carcinoma (3–8). In
addition, the mass-like pulmonary opacity, commonly caused by
endobronchial infections, including mucus plugs distal to a
centrally obstructing lesion due to a fungus or tuberculosis, also
simulate an endobronchial mass on CT scans (9–11). In
the current patient, an ill-defined mass in the upper lobe of the
right lung was identified, with ipsilateral mediastinal lymph node
swelling. Therefore, an endobronchial lesion was not diagnosed in
this patient until the bronchoscopy examination.
It is generally accepted that the bronchoscopic
findings of endobronchial lesions of primary lung carcinoma are
difficult to distinguish from those of metastatic lung carcinoma
and non-malignant tumors (12,13).
Bronchoscopic examinations are used for the diagnosis of
endobronchial lesions as the majority of lesions are within the
view and range of the bronchoscopic field. In specific cases, the
value of bronchoscopic examinations may be limited as the admixture
of necrotic material may prevent the collection of a sufficient
specimen for diagnosis (9–11), however, the formation of a
pathological diagnosis using specimens obtained by a bronchoscopic
biopsy is mandatory for the generation of a correct diagnosis.
Non-malignant endobronchial tumors generally have a smooth surface
with uniform color (14). The most
common sites associated with endobronchial metastasis are the
breast, kidney and colon (5–7).
Metastatic endobronchial tumors often presents as polypoid or
nodular lesions covered with necrotic material (15). Squamous cell carcinoma is the most
common histological type of primary lung carcinoma in a central
location and with endobronchial extensions (4). In this cell type, polypoid lesions
with a rough surface covered with necrotic material are the most
predominant lesions (16,17). Although SCLC with endobronchial
growth is extremely rare, specific cases have been reported
(18,19). Ramaraju et al reported an
unusual case of centrally-located combined SCLC with a squamous
cell component, which was diagnosed by an endo-bronchial lung
biopsy (18). In addition, Lee
et al presented the case of a 51-year-old male with SCLC and
an endobronchial mass in the left main bronchus (19). In these cases, the tumors contained
elements of SCLC mixed with a component of squamous cell carcinoma
(18,19). Patients with combined SCLC have a
higher incidence of peripheral lesions, and as a consequence, the
central location of the tumor in the present case was unusual. The
low incidence rate and often small and inadequate specimens
obtained by bronchoscopic biopsy make it difficult to diagnose
combined SCLC without surgical resection (20).
In the present case study, the SCLC originated
endobronchially from the upper lobe of the lung. Chest CT scans
revealed that its location was central. A bronchoscopic examination
identified an irregularly covered partly-whitish tissue,
representative of the necrotic material coverage.
Bronchoscopically, squamous cell lung cancer was considered as a
differential diagnosis, although no such component was observed
pathologically in the present study. The tumor was not found to
exhibit necrotic material or other cell types of lung cancer and an
admixture of fibrin in the outer stratum was found, indicative of
necrotic material.
Despite SCLC with endobronchial growth being an
extremely rare tumor presentation, the clinical evaluation of this
diagnosis in patients presenting with a pulmonary tumor adjacent to
the bronchus and an endobronchial polypoid lesion must not
overlooked.
References
|
1.
|
Travis WD, Travis LB and Devesa SS: Lung
Cancer. Cancer. 75:191–202. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Brambilla E, Travis WD, Colby TV, et al:
The new World Health Organization Classification of lung tumours.
Eur Respir J. 18:1059–1068. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Unger M: Endobronchial therapy of
neoplasms. Chest Surg Clin N Am. 13:129–147. 2003. View Article : Google Scholar
|
|
4.
|
Koss MN, Hochholzer L and Frommelt RA:
Carcinosarcomas of the lung: a clinicopathologic study of 66
patients. Am J Surg Pathol. 23:1514–1526. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Katsimbri PP, Bamias AT, Froudarakis ME,
et al: Endobronchial metastases secondary to solid tumors: report
cases and review of the literature. Lung Cancer. 28:163–170. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Braman SS and Whitcomb ME: Endobronchial
metastasis. Arch Intern Med. 135:543–547. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Seo JB, Im JG, Goo JM, et al: Atypical
pulmonary metastases: spectrum of radiologic findings.
Radiographics. 21:403–417. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Shah H, Garbe L, Nussbaum E, et al: Benign
tumors of the tracheobronchial tree. Endoscopic characteristics and
role of laser resection Chest. 107:1744–1751. 1995.PubMed/NCBI
|
|
9.
|
Lau KY: Endobronchial actinomycosis
mimicking pulmonary neoplasm. Thorax. 47:664–665. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Kim JS, Rhee Y, Kang SM, et al: A case of
endobronchial aspergilloma. Yonsei Med J. 41:422–425. 2000.
View Article : Google Scholar
|
|
11.
|
Van den Brande P, Lambrechts M, Tack J, et
al: Endobronchial tuberculosis mimicking lung cancer in elderly
patients. Respir Med. 85:107–109. 1991.PubMed/NCBI
|
|
12.
|
Murakami S, Watanabe Y, Saitoh H, et al:
Treatment of multiple primary squamous cell carcinomas of the lung.
Ann Thorac Surg. 60:964–969. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Saida Y, Kujiraoka Y, Akaogi E, et al:
Early squamous cell carcinoma of the lung: CT and pathologic
correlation. Radiology. 201:61–65. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Oshikawa K, Ohno S, Ishii Y, et al:
Evaluation of bronchoscopic findings in patients with metastatic
pulmonary tumor. Intern Med. 37:349–353. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Wilson RW and Kirejczyk W: Pathological
and radiological correlation of endobronchial neoplasms: Part I,
Benign tumors. Ann Diagn Pathol. 1:31–46. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Lam B, Wong MP, Fung SL, et al: The
clinical value of autofluorescence bronchoscopy for the diagnosis
of lung cancer. Eur Respir J. 28:915–919. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Shulman L and Ost D: Advances in
bronchoscopic diagnosis of lung cancer. Curr Opin Pulm Med.
13:271–277. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Ramaraju K, Aggarwal B, Kulsrestha R, et
al: Unusual presentation of an uncommon lung malignancy. Lung
India. 25:132–134. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Lee JE, Park HS, Jung SS, et al: A case of
small cell lung cancer treated with chemoradiotherapy followed by
photodynamic therapy. Thorax. 64:637–679. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Roggli VL, Vollmer RT, Greenberg SD, et
al: Lung cancer heterogeneity: a blinded and randomized study of
100 consecutive cases. Hum Pathol. 16:569–579. 1985. View Article : Google Scholar : PubMed/NCBI
|