Introduction
Intraosseous lipoma represents a relatively rare
lesion composed of mature adipose tissue. The true incidence
remains unknown, as the majority of lesions are asymptomatic and do
not require medical attention. A number of authors have
characterized these lesions as benign tumors of the medullary fat
tissue (1,2). However, there have been four published
cases of intracortical lipoma (3–6). To
the best of our knowledge, intracortical lipoma in an adult tibia
has not been previously described. The current case report
describes an adult patient with symptomatic intracortical lipoma in
the tibial diaphysis. The study was approved by the ethics
committee of Chung-Ang University (Seoul, Korea). Written informed
consent was obtained from the patient’s family.
Case report
A 23-year-old male presented to the Department of
Orthopedic Surgery (College of Medicine, Chung-Ang University,
Seoul) with pain and discomfort on the lateral aspect of the tibia.
The patient denied history of trauma and had no past medical
history. On physical examination, no visible or palpable mass,
erythema, or warmth were noted. However, there was mild local
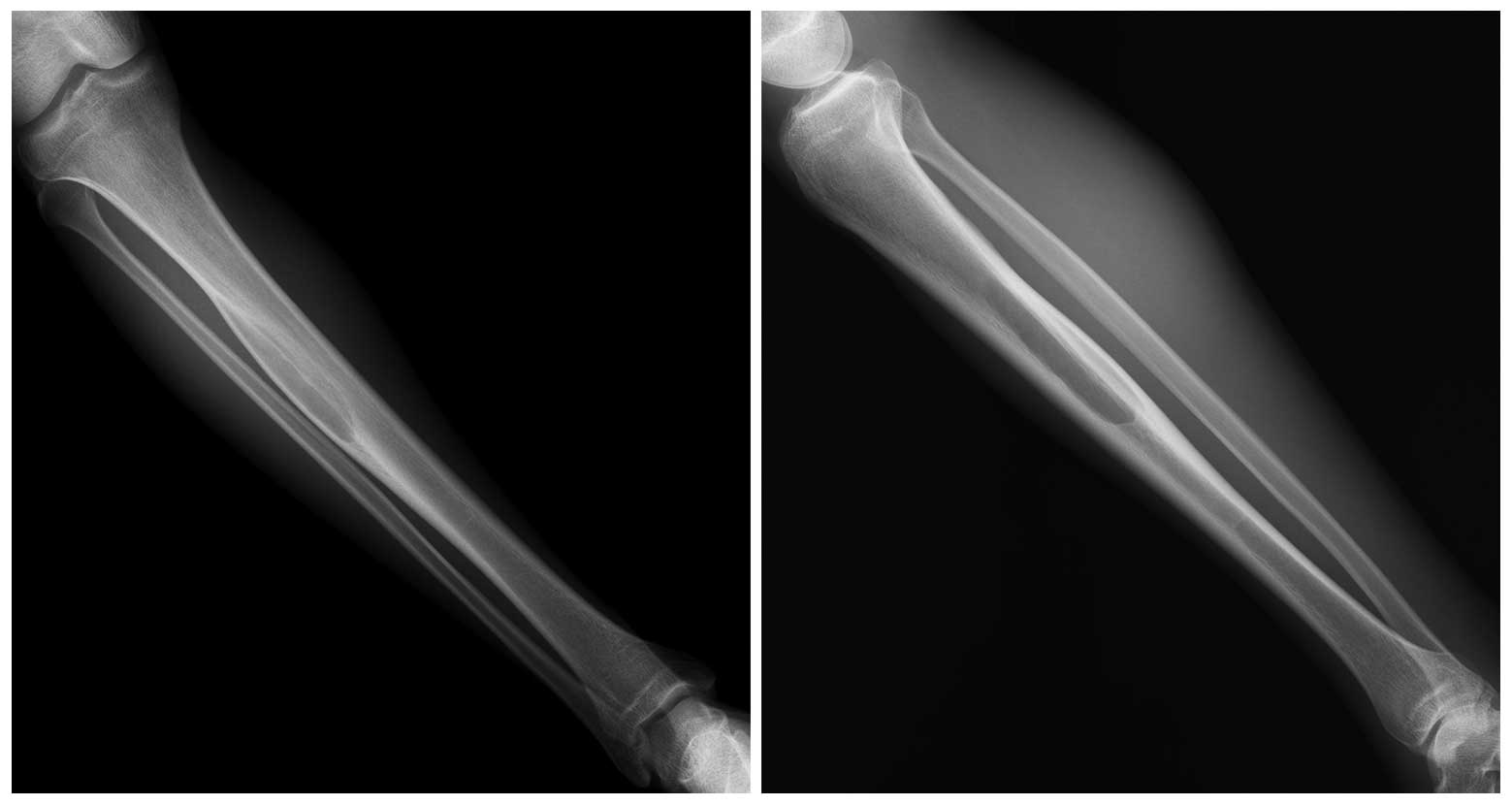
tenderness on the lateral side of the tibia. Radiographs showed a
well-defined osteolytic lesion in the tibial diaphysis with bulging
on the posterolateral side. Plain radiographs did not show any
evidence of periosteal reaction or cortical destruction (Fig. 1), however, confinement of the lesion
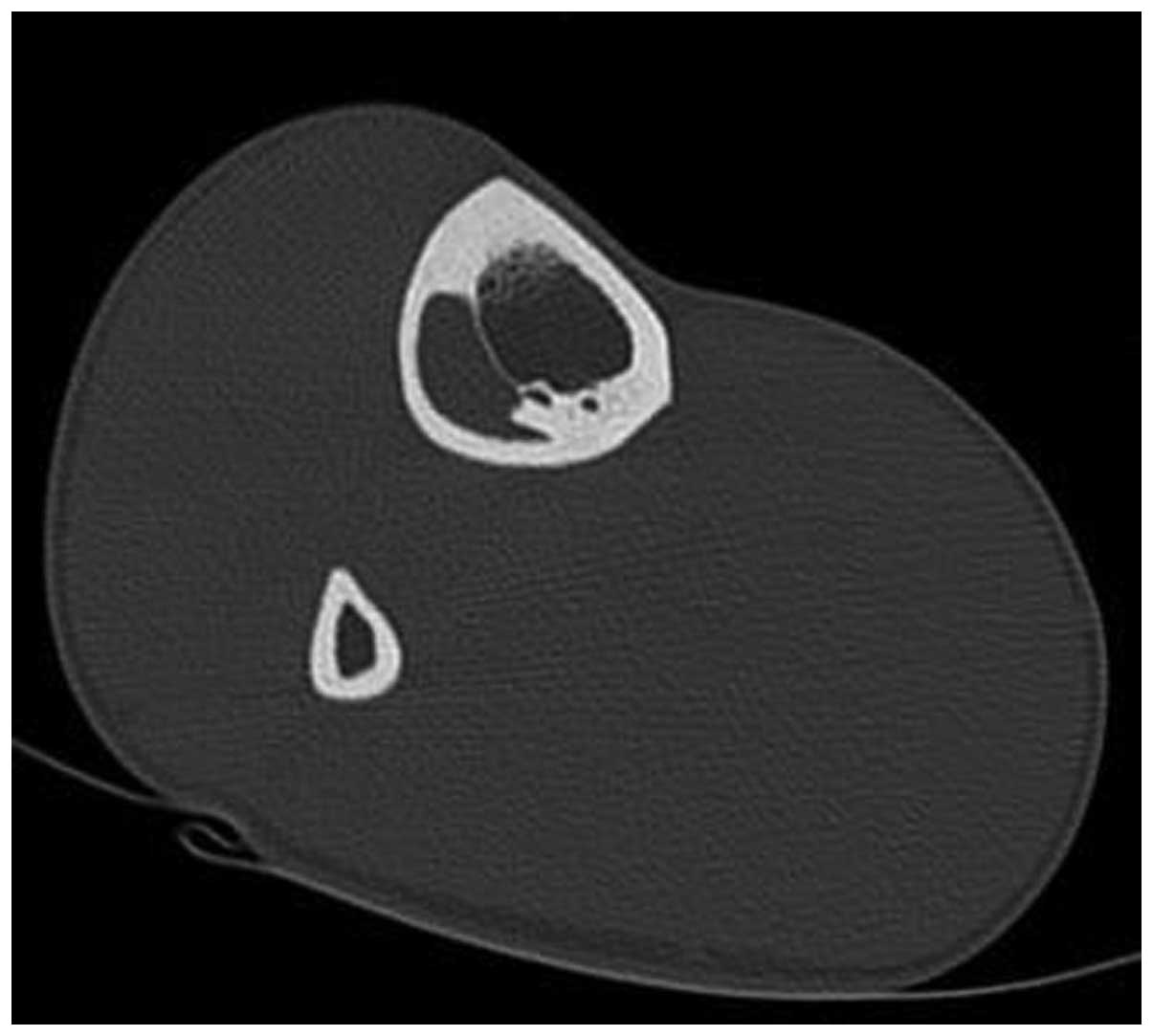
to the cortex could not be confirmed. Computed-tomography (CT)
scanning revealed a lucent lesion with regular margins, which did
not involve the medullary cavity. The lesion was well-circumscribed
and surrounded by sclerotic bone. The measurements were 90 mm in
length and 20×10 mm in maximum diameter (Fig. 2). Magnetic resonance imaging (MRI)
revealed that the lesion consisted of two different components, a
central portion with low-signal intensity on T1-weighted MRI and
high-signal intensity on T2-weighted MRI, and a peripheral portion
with high-signal intensity on T1-weighted and T2-weighted MRI
(Fig. 3). Technetium-99m
scintigraphic scanning revealed increased isotope uptake at the
lesion site. Based on the collective findings, the radiologist
raised the possibility of an intracortical lipoma.
Excisional biopsy was performed to clarify the
diagnosis. Following an incision on the anterolateral skin,
periosteal dissection of the anterior compartment muscles was
completed. The lesion was then identified to be bulging laterally
and the surrounding cortical bone was removed. Macroscopically, the
lesion showed cystic changes and was composed of fat tissue.
Curettage was performed and the true cortex was located beneath the
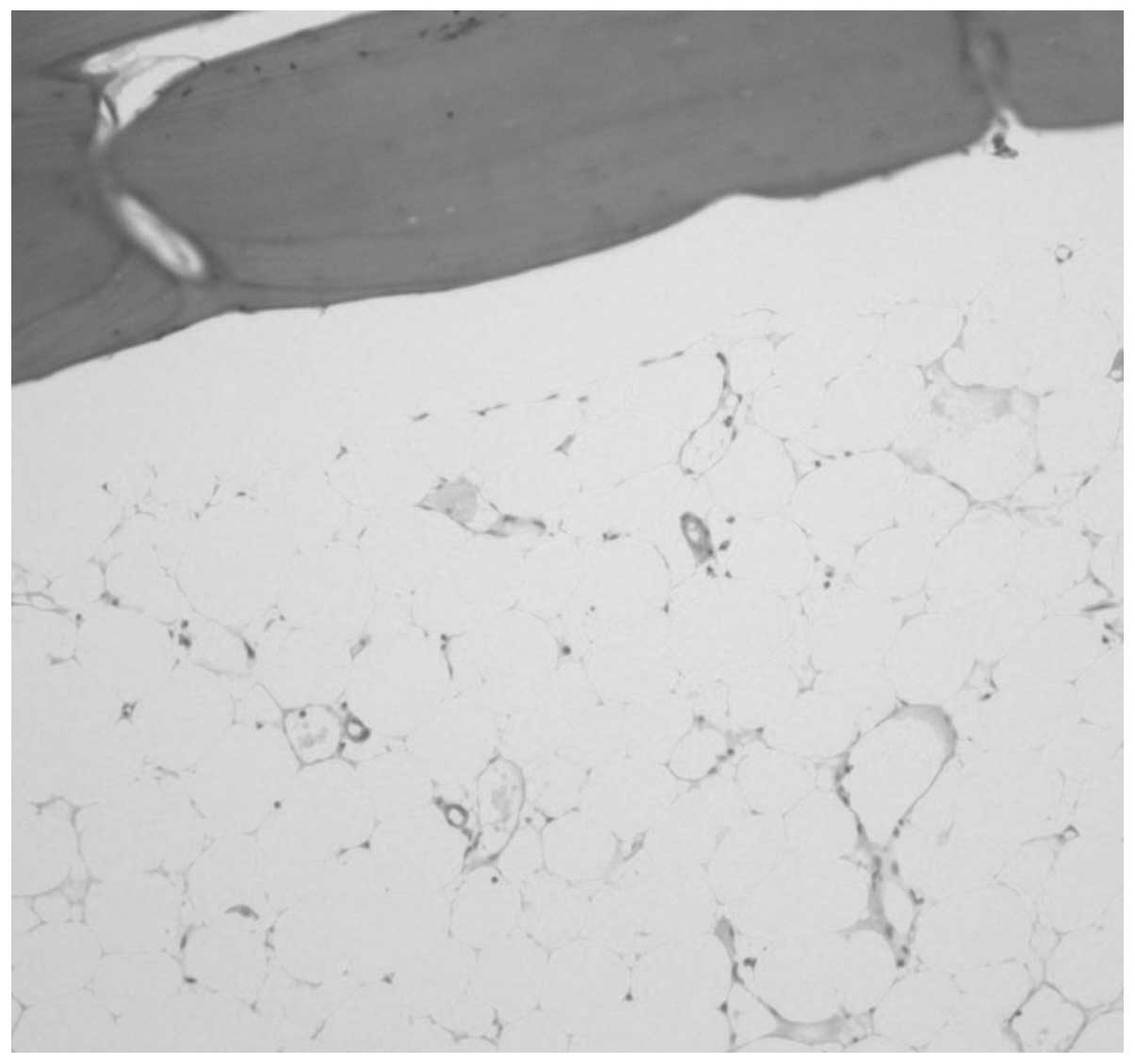
lesion (Fig. 4). Histopathological
examination of the resected and curettage samples showed mature
adipocytes with trabecular bone. No cellular atypia, fat necrosis
or calcifications were observed (Fig.
5). Pain and discomfort disappeared during the postoperative
period, and no tumor recurrence was observed at the 12-month
postoperative follow-up.
Discussion
Intraosseous lipoma is a rare, benign bone tumor
that accounts for <0.1% of primary bone tumors (7). Differential diagnosis includes
non-ossifying fibroma, simple bone cyst, fibrous dysplasia,
enchondroma, aneurismal bone cyst, bone infarct and osteomyelitis
(1,8–10).
This particular tumor occurs most frequently in the lower limb,
particularly in the calcaneus. Other common sites include long bone
metaphyses (11). The majority of
lesions are located intramedullary, and cortical bone involvement
is rare. According to published reports, four cases of
intracortical lipoma have been previously described. Of these
cases, three patients were adults and all tumors were located in
the femoral diaphysis (3,4,6). The
remaining case report was of a seven-year-old pediatric patient
with a tumor located in the tibial metaphysis (5). All four patients were female, two
patients presented with pain and two lesions were found
incidentally. The present case study appears to be the first report
of an adult patient with an intracortical lipoma in the tibial
diaphysis (Table I).
 | Table ISummary of case reports of
intracortical lipomas. |
Table I
Summary of case reports of
intracortical lipomas.
| Study (year)
[ref] | Age, years | Gender | Location | Radiological
observations | Symptoms | Treatment |
|---|
| Downey et
al(1983) [3] | 34 | Female | Diaphysis of
femur | Incidental
finding | Dense, separated
lesion expanding the cortical outline of the diaphysis. | Surgical
excision |
| Yamamoto et
al(2002) [6] | 74 | Female | Diaphysis of
femur | Thigh pain | Small osteolytic
lesion in the lateral diaphyseal cortex. | Surgical
excision |
| Lee et
al(2007) [4] | 31 | Female | Diaphysis of
femur | Incidental
finding | Well-defined,
expansile, radiolucent lesion with multiple septa in the diaphyseal
cortex. | Surgical
excision |
| Madhuri et
al(2007) [5] | 7 | Female | Metaphysis of
tibia | Proximal tibia
pain | Sclerosis of the
upper-anteromedial tibial cortex that contained a linear lytic
lesion. | Surgical
excision |
| Current study
(2013) | 23 | Male | Diaphysis of
tibia | Lateral tibia
pain | Well-defined
osteolytic lesion in the diaphysis of the tibia with mild bulging
on the posterolateral side. | Surgical
excision |
Radiographic appearance of intraosseus lipomas
varies but can include well-defined osteolytic lesions with
marginal sclerosis. Radionuclide bone scanning can be positive or
negative and, therefore, has limited diagnostic utility (12). Although diagnosis of intracortical
lipoma on plain radiographs remains challenging, CT and MRI are
useful for detecting fat within the lesion and for helping to
confirm a purely intracortical location (7). Lipoma fat can be easily recognized on
MRI by high-signal intensity on T1- and T2-weighted images. Cyst
signal intensity is low on T1-weighted MRI but high on T2-weighted
MRI due to the fluid component. In the present patient, peripheral
high-signal density on T1- and T2-weighted MRI scans was captured
due to fat tissue. The central portion of the cystic change showed
low-signal intensity on T1-weighted MRI and high-signal intensity
on T2-weighted MRI. In operation filed, we could confirm that the
radiological finding corresponded to the pathologic specimen.
Previously, Milgram (8) subdivided intraosseous lipomas into
three stages. Stage 1 lesions are purely radiolucent and consist
almost entirely of fat tissue. In stage 2 lesions, central
calcifications with adjacent minor cystic degeneration in viable
adipocytes are observed. Stage 3 lesions represent late cases in
which fat has been devitalized with varying degrees of cyst
formation, calcification and reactive bone formation. Although
there were no calcific changes, we hypothesize that the
histological observations of the current case are consistent with
stage 3 lesions, due to the appearance of cystic changes.
The pathogenesis of intracortical lipomas remains
controversial. A number of authors have suggested that lesions
represent benign tumors of medullary adipose tissue (1,2).
Others consider these lesions to be products of reactive changes
secondary to infarct, infection or trauma (13). It has also been proposed that cyst
formation results from degeneration of a pre-existing lipoma, or
that a lipoma represents the late-stage of a simple bone cyst
(11). However, none of the
aforementioned theories adequately explain the underlying
pathogenesis of an intracortical lipoma.
The majority of intraosseous lipomas can be managed
conservatively. Surgery is indicated for symptomatic lesions,
malignancy, or risk of pathological fracture. Surgical treatment
usually consists of curettage and bone grafting (11). For the current case, surgical
treatment was performed, as the lesion was large and the patient
complained of mild pain. Furthermore, confirmation that the lesion
was a benign, intracortical lipoma was not obtained.
In conclusion, the current report presents a case of
an adult male with an intracortical lipoma accompanied by cystic
changes in the tibial diaphysis. Intracortical lipoma represents a
rare, benign bone tumor typically discovered incidentally. Although
biopsy is required to confirm diagnosis, CT and MRI are useful
imaging modalities to elucidate lesion characteristics and
location. Intracortical lipomas should be included in the
differential diagnosis of intracortical, osteolytic lesions of long
bones.
Acknowledgements
This study was supported by a grant from the Basic
Science Research Program through the National Research Foundation
of Korea funded by the Ministry of Education, Science and
Technology (2013R1A1A2007989).
References
|
1
|
Barcelo M, Pathria MN and Abdul-Karim FW:
Intraosseous lipoma. A clinicopathologic study of four cases. Arch
Pathol Lab Med. 116:947–950. 1992.PubMed/NCBI
|
|
2
|
Chow LT and Lee KC: Intraosseous lipoma. A
clinicopathologic study of nine cases. Am J Surg Pathol.
16:401–410. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Downey EF Jr, Brower AC and Holt RB: Case
report 243. Cortical ossifying lipoma of femur. Skeletal Radiol.
10:189–191. 1983.PubMed/NCBI
|
|
4
|
Lee SJ, Yoon JH, Bae JI, et al:
Intracortical lipoma of the femur. Skeletal Radiol. 36:S77–S81.
2007. View Article : Google Scholar
|
|
5
|
Madhuri V, Manipadam MT, Walter NM and
Cherian RA: Intracortical lipoma of bone: report of the first case
in a child. J Pediatr Orthop B. 16:327–329. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yamamoto T, Marui T, Akisue T, et al:
Intracortical lipoma of the femur. Am J Surg Pathol. 26:804–808.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Eyzaguirre E, Liqiang W, Karla GM,
Rajendra K, Alberto A and Gatalica Z: Intraosseous lipoma. A
clinical, radiologic, and pathologic study of 5 cases. Ann Diagn
Pathol. 11:320–325. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Milgram JW: Intraosseous lipomas. A
clinicopathologic study of 66 cases. Clin Orthop Relat Res.
277–302. 1988.PubMed/NCBI
|
|
9
|
Lauf E, Mullen BR, Ragsdale BD and Kanat
IO: Intraosseous lipoma of distal fibula. Biomechanical
considerations for successful treatment. J Am Podiatry Assoc.
74:434–440. 1984. View Article : Google Scholar
|
|
10
|
Appenzeller J and Weitzner S: Intraosseous
lipoma of os calcis. Case report and review of literature of
intraosseous lipoma of extremities. Clin Orthop Relat Res. 171–175.
1974.PubMed/NCBI
|
|
11
|
Campbell RS, Grainger AJ, Mangham DC,
Beggs I, Teh J and Davies AM: Intraosseous lipoma: report of 35 new
cases and a review of the literature. Skeletal Radiol. 32:209–222.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Murphey MD, Carroll JF, Flemming DJ, Pope
TL, Gannon FH and Kransdorf MJ: From the archives of the AFIP:
benign musculoskeletal lipomatous lesions. Radiographics.
24:1433–1466. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Barker GR and Sloan P: Intraosseous
lipomas: clinical features of a mandibular case with possible
aetiology. Br J Oral Maxillofac Surg. 24:459–463. 1986. View Article : Google Scholar
|