Introduction
Fluorodeoxyglucose positron emission
tomography/computed tomography (FDG PET/CT) is used in the imaging
workup of various malignancies for staging and surveillance
(1). Incidental gastrointestinal
observations are found in ~3% of patients undergoing evaluation for
non-gastrointestinal diseases (2).
These incidental observations in asymptomatic patients may be of
clinical significance (2–4). The value of FDG PET or FDG PET/CT for
identifying incidental pre-malignant and malignant colonic lesions
has previously been reported (4–8). The
early detection and treatment of colonic pre-malignant and
malignant lesions may significantly improve survival, whereas
further unnecessary studies may delay treatment of the primary
disease. Studies that document the follow-up of these incidental
observations to the point of histological confirmation are of great
importance since they are the only means to evaluate the true
positive rates of pre-malignant and malignant lesions identified by
FDG PET/CT (8,9).
The aim of the present study was to evaluate
endoscopic and histopathological observations in patients who were
referred for colonoscopy due to incidental FDG colonic uptake on a
PET/CT study.
Patients and methods
The FDG-PET/CT database was retrospectively searched
for patients in whom colonic FDG uptake was incidentally found and
who then underwent colonoscopy between January 2007 and June 2009.
Following identification of the specific patient population, the
following data were retrieved from their medical records:
Demographics, medical history, indications for performing FDG
PET/CT, results of PET/CT and endoscopic and histopathological
observations. Patients with known colon cancer or previous colonic
surgery were excluded from further evaluation. The Institutional
Review Board of Rambam Health Care Campus (Technion, Israel)
approved this retrospective study and the requirement to obtain
informed consent was waived.
Results
The present study consisted of 56 patients (25 males
and 31 females) with a mean age of 72 years old (range, 43–89 years
old). The patient characteristics and indications for FDG PET/CT
are listed in Table I. Overall, 60
foci of FDG uptake were found in the 56 patients. Of the
occurrences indicative of focal FDG uptake in the colon, 13 were in
the ascending colon, 6 in the transverse colon, 14 in the
descending colon, 25 in the rectosigmoid and 2 in the ileum. The
colonoscopy was normal in 35 patients (63%), and endoscopic
observations were found in 21 patients (37%). In these 21 patients,
30 lesions were found; 20/30 (67%) were benign adenomatous polyps,
6/30 (20%) were advanced histological lesions (with features of
high-grade dysplasia or carcinoma in situ), a malignancy was
detected in 3/30 lesions (10%) and 1/30 (3%) was a benign
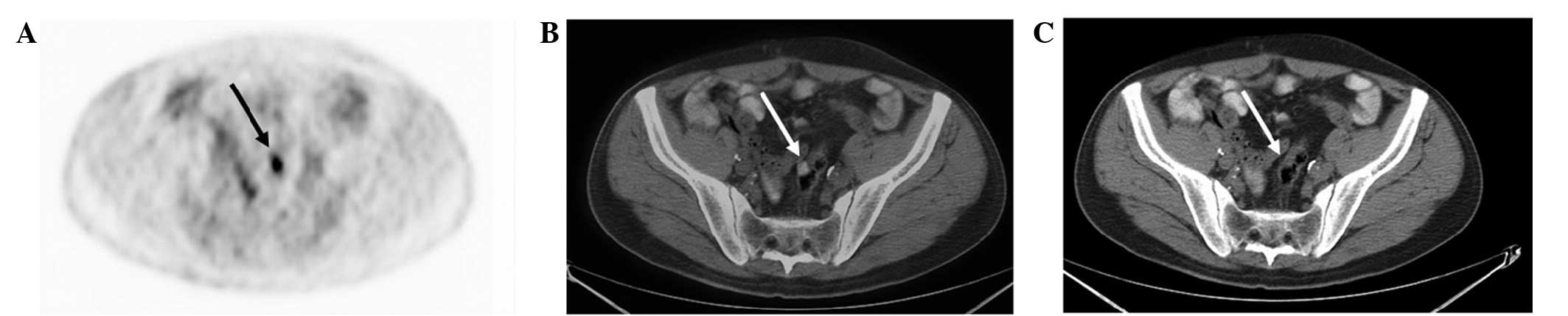
hyperplastic polyp (Table II;
Figs 1 and 2). Diverticular disease, with no
endoscopic signs of inflammation, was found in 7/56 patients
(12.5%) with positive FDG PET/CT results.
 | Table IIndication for FDG PET/CT (n=56). |
Table I
Indication for FDG PET/CT (n=56).
| Primary disease | Patients, n | Indication for FDG
PET/CT |
|---|
| Colorectal
cancer | 16 | In 15 patients,
imaging was performed as part of surveillance or due to increased
levels of CEA. One patient had a known metastatic disease without
bowel sites of disease |
| Non-Hodgkin
lymphoma | 14 | Staging
Assessment of new suspicious lesions |
| Breast cancer | 5 | Suspected metastatic
disease |
| Lung cancer | 7 | Staging |
| Melanoma | 3 | Staging
Response to systemic treatment |
| Hodgkin lymphoma | 2 | Surveillance |
| Bladder cancer | 2 | Assessment of new
lung lesion
Assessment of response to systemic treatment |
| Malignant
hystiocytoma | 1 | Suspected
recurrence |
| Gastric cancer | 1 | Suspected lesions in
the lung and liver |
| Cervix cancer | 1 | Surveillance |
| Pancreatic
cancer | 1 | Staging |
| Tongue cancer | 1 | Staging |
| Skin squamous cell
cancer | 1 | Staging |
| Fever of unknown
origin | 1 | To determine to
source of prolonged fever |
 | Table IIAnatomical site of FDG foci and
histological observations. |
Table II
Anatomical site of FDG foci and
histological observations.
| Parameter | Malignant, n | Advanced adenoma,
n | Benign, n |
|---|
| Foci | 3 | 6 | 21 |
| Anatomical site |
| Ascending colon | | 1 | 5 |
| Descending
colon | 1 | 2 | 7 |
| Rectosigmoid | 2 | 3 | 9 |
| Normal colonoscopy
(including diverticular disease) | | | 35 |
Discussion
The potential of FDG PET or FDG PET/CT in colorectal
screening has been studied in numerous trials (4–9). Focal
colonic FDG uptake has up to a 70–80% probability of showing
corresponding abnormal histopathological observations (4,6).
Gutman et al(6) evaluated
the positive predictive value of FDG PET/CT for the detection of
colonic abnormalities. The study focused on the ability of FDG
PET/CT to detect advanced adenomas (adenomas of >10 mm in
diameter, adenomas with a villous component or moderate to severe
dysplasia) and carcinomas. Among the 20 patients who underwent a
colonoscopy, 5 had a normal colonoscopy (25%) and 15 (75%) patients
had pathological lesions. In these 15 patients, a total of 18
lesions were found, including 2 benign hyperplastic polyps in the
rectosigmoid and 16 advanced neoplasms. The advanced neoplasms
consisted of 13 villous adenomas and 3 adenocarcinomas.
In an additional series of 3,210 PET scans performed
for screening in asymptomatic patients, focal FDG avid uptakes were
found in 20 patients, corresponding to 12 villous adenomas, 6
carcinomas and 2 tubular adenomas in the colonoscopy (4). These results are consistent with other
studies showing that FDG PET ± CT is a sensitive tool to detect
colonic premalignant lesions (4,6,7,9,10).
However, caution must be applied, as the true negative rates are
rarely evaluated in studies (9). It
should be noted that FDG PET/CT is not a screening test for colon
lesions; however, these were incidental observations detected
during the evaluation of other diseases.
The majority of studies evaluating incidental
colonic observations did not include patients with colorectal
cancer. In the present study, the primary disease was colorectal
cancer in 16 patients; however, all the patients had undergone
surgical resection of their primary lesions and had no evidence of
disease located in the bowel. Moreover, the medical files of
patients who underwent a colonoscopy due to colonic observations on
FDG PET/CT were reviewed, therefore, the rates of incidental
colonic observations or the false negative rates were not
evaluated. The true positive rates (36%) in the current study were
lower than reported by others. Despite possible false-positive
results, colonoscopy is recommended as the next diagnostic step for
further evaluation of such observations. Since there are numerous
confounding factors when evaluating the colorectal region,
including fecal impaction, muscular peristaltic activity and
inflammation, re-evaluation of the scan is advised. Gutman et
al(6) indicated that in 3
patients, re-evaluation led to a different conclusion from that of
the scan report regarding the nature of the FDG focal colonic
uptake. The re-evaluation indicated that the colonic lesion was
consistent with physiological activity, as the FDG uptake was
located in the colonic lumen without bowel-wall involvement in an
area of fecal stasis.
Although the present study found a lower incidence
of lesions in the colon following colonoscopy, in 20 patients,
colonic FDG observations matched the colonoscopic abnormalities,
the majority of which required further surveillance and treatment.
In the majority of cases of complete endoscopic resection, even in
cases of carcinoma in situ or adenoma (tubular,
tubulovillous or villous) with favorable histological features (T1
lesion, grade 1–2, no lymphovascular invasion, negative margins and
no fragmentation of the specimen), no further treatment is required
(11,12). However, appropriate endoscopic
surveillance is mandatory (12).
In the present study, in one patient with a normal
colonoscopy who exhibited a complete response to metastatic colon
carcinoma, the colonic observation disappeared in a subsequent FDG
PET/CT following chemotherapy. However, a later FDG PET/CT scan
indicated diffuse metastatic disease involving the lung, liver and
pelvis. A total of 35 FDG observations did not match any
colonoscopic abnormality in the present study, thus, the PET/CT
scan results were interpreted as false positive (62.5%). Of these
false positive results, 7 revealed diverticular-disease with no
endoscopic signs of inflammation. Peng et al(8) indicated that false-positive FDG uptake
is more commonly observed in the right colon; this observation is
not consistent with the present study. In the current study, the
maximal standardized uptake (SUVmax) was not evaluated
and the clinical significance of the SUVmax from
previous studies was inconclusive (5,8). The
SUVmax value was higher in cancer patients, however, a
high SUVmax value does not necessarily result in the
detection of malignancies (5,8).
A positive FDG uptake that was followed by a normal
endoscopy was considered physiological FDG uptake in the bowel. As
shown in Table I, in specific
patients, the indication for FDG PET/CT was pre-treatment staging,
whereas for others, it was performed to evaluate the response to
treatment of metastatic disease. Therefore, the timing and
relevance of colonoscopic investigation must be dictated by
clinical judgment and the status of the primary tumor.
References
|
1
|
Bar-Shalom R, Valdivia AY and Blaufox D:
PET imaging in oncology. Semin Nucl Med. 30:150–185. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kamel EM, Thumshirn M, Truninger K, et al:
Significance of incidental 18F-FDG accumulations in the
gastrointestinal tract in PET/CT: correlation with endoscopic and
histopathologic results. J Nucl Med. 45:1804–1810. 2004.PubMed/NCBI
|
|
3
|
Agress H Jr and Cooper BZ: Detection of
clinically unexpected malignant and premalignant tumors with
whole-body FDG PET: histopathologic comparison. Radiology.
230:417–422. 2004. View Article : Google Scholar
|
|
4
|
Chen YK, Kao CH, Liao AC, et al:
Colorectal cancer screening in asymptomatic adults: the role of FDG
PET scan. Anticancer Res. 23:4357–4361. 2003.PubMed/NCBI
|
|
5
|
Israel O, Yefremov N, Bar-Shalom R, Kagana
O, Frenkel A, Keidar Z and Fischer D: PET/CT detection of
unexpected gastrointestinal foci of 18F-FDG uptake: incidence,
localization patterns, and clinical significance. J Nucl Med.
46:758–762. 2005.
|
|
6
|
Gutman F, Alberini JL, Wartski M, et al:
Incidental colonic focal lesions detected by FDG PET/CT. AJR Am J
Roentgenol. 185:495–500. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tatlidil R, Jadvar H, Bading JR and Conti
PS: Incidental colonic fluorodeoxyglucose uptake: correlation with
colonoscopic and histopathologic findings. Radiology. 224:783–787.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Peng J, He Y, Xu J, et al: Detection of
incidental colorectal tumours with 18F-labelled
2-fluoro-2-deoxyglucose positron emission tomography/computed
tomography scans: results of a prospective study. Colorectal Dis.
13:e374–e378. 2011. View Article : Google Scholar
|
|
9
|
Weston BR, Iyer RB, Qiao W, Lee JH,
Bresalier RS and Ross WA: Ability of integrated positron emission
and computed tomography to detect significant colonic pathology:
the experience of a tertiary cancer center. Cancer. 116:1454–1461.
2010. View Article : Google Scholar
|
|
10
|
Drenth JP, Nagengast FM and Oyen WJ:
Evaluation of (pre-)malignant colonic abnormalities: endoscopic
validation of FDG-PET findings. Eur J Nucl Med. 28:1766–1769. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Markowitz AJ and Winawer SJ: Management of
colorectal polyps. CA Cancer J Clin. 47:93–112. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Winawer SJ, Zauber AG, Fletcher RH, et al:
Guidelines for colonoscopy surveillance after polypectomy: a
consensus update by the US Multi-Society Task Force on Colorectal
Cancer and the American Cancer Society. CA Cancer J Clin.
56:143–159. 2006. View Article : Google Scholar
|