Introduction
Primary adenocarcinoma of the appendix is a rare
malignancy with ~0.12 cases per 1,000,000 individuals diagnosed
annually (1). The condition was
first described by Berger in 1882 (2). Primary epithelial malignancies of the
appendix are divided into three categories, including mucinous
adenocarcinomas, intestinal-type adenocarcinomas and signet ring
cell carcinomas (3–5). The mucinous adenocarcinoma is the most
frequent histological type among the identified appendiceal
carcinomas (1). As an uncommon
clinical entity, a primary adenocarcinoma of the appendix only
amounts for 0.01–0.2% of all gastrointestinal neoplasms (6) and it is extremely difficult to
diagnose prior to surgical inspection; ≤50% of cases are diagnosed
during intraoperative exploration of the peritoneal cavity
(7–9). The diagnosis of primary appendiceal
mucinous adenocarcinoma usually depends on the pathology following
appendectomy or other explorative surgical procedures (10). The current case report presents a
54-year-old male with primary appendiceal mucinous adenocarcinoma
mimicking urinary bladder carcinoma.
Case report
A 54-year-old previously healthy male presented at
the Shandong Provincial Qianfoshan Hospital Affiliated to Shandong
University (Jinan, China) with the clinical presentation of
continuous frequent micturition, urgent urination and odynuria for
approximately six months. The patient did not have a fever or any
gastrointestinal symptoms. A physical examination was normal and
laboratory tests showed microscopic, but no gross, hematuria. The
level of tumor markers, carcinoembryonic antigen and carbohydrate
antigen 19-9, were normal. A previous ultrasound at the patient’s
local hospital showed a bladder tumor (only described orally by the
patient without providing the formal diagnostic report). The
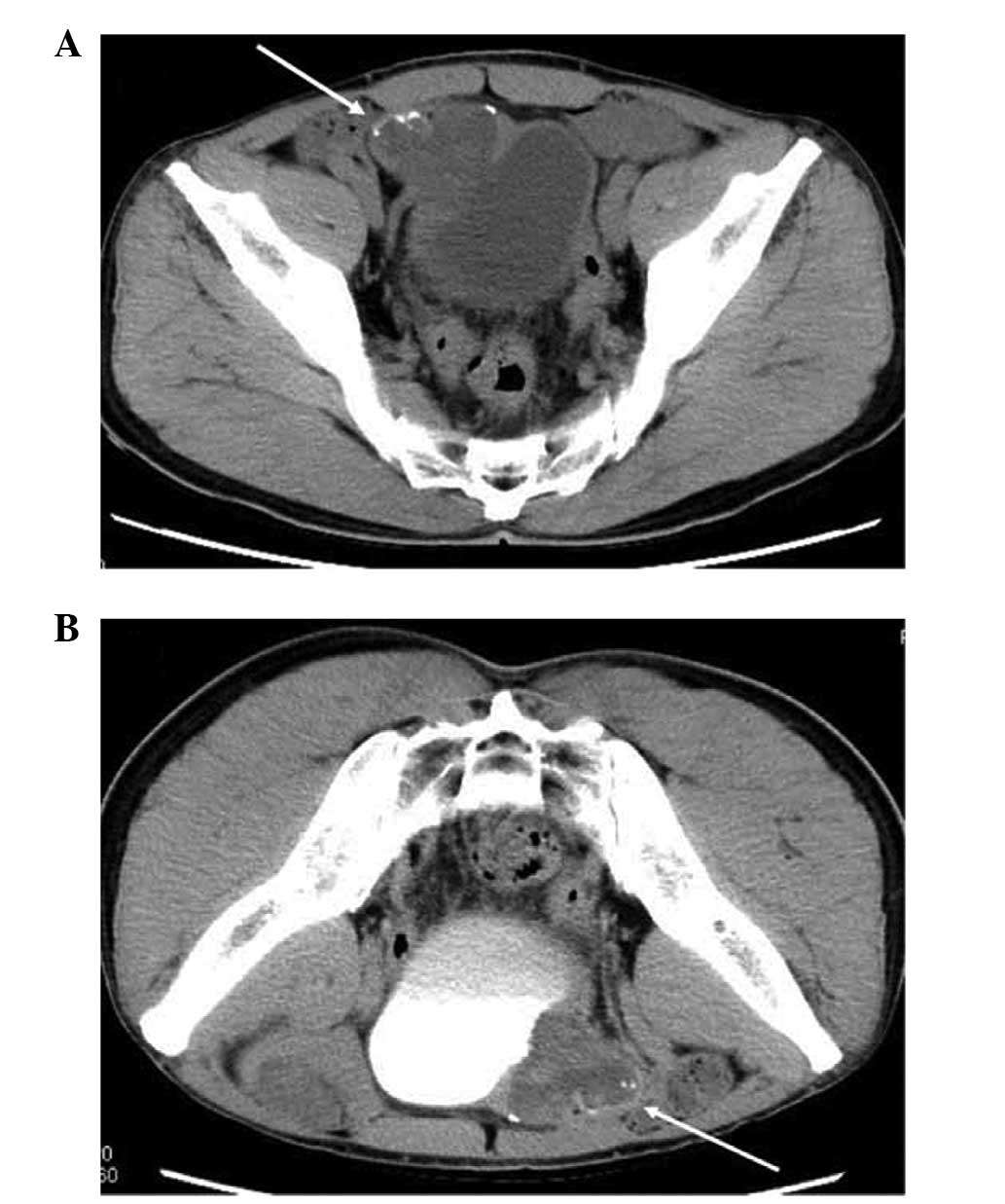
enhanced abdomen computed tomography (CT) scan revealed a hypodense
mass (5.4×4.6 cm at the maximum section) at the level of the right
anterior bladder wall, with sporadic calcifications in the
peripheral area. The mass was moderately and heterogeneously
enhanced in postcontrast images (Fig.
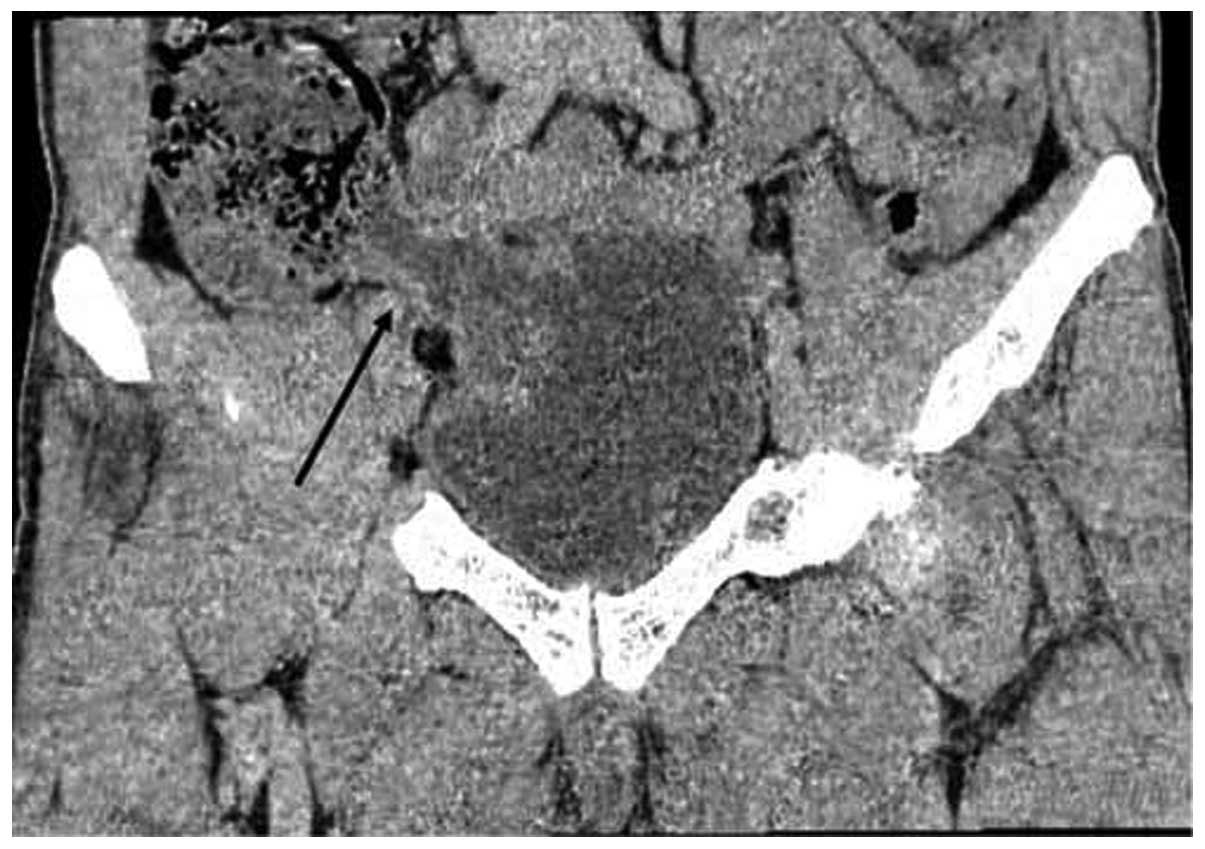
1). From the coronal multiplanar reconstruction (MPR) imaging,
the mass was shown to connect with the ileocecal junction along the
area of the appendix, and the density of the liquid content was low
(Fig. 2). This sign indicated that
the mass may be closely associated with the intestinal tract,
although it appeared to be a urinary bladder carcinoma. The patient
provided written informed consent.
During the surgery, a mass with a maximum diameter
of 5 cm was identified at the level of the right anterior bladder
wall, markedly adhesive to the surrounding tissues. Following
dissection of the peritoneum, the mass was detected to connect and
adhere to the ileocecal junction, and normal appendix tissues were
not found. Following consultation, gastrointestinal surgery experts
considered that the tumor was of appendiceal origin, invading the
urinary bladder. The frozen section revealed a mucinous
adenocarcinoma of the appendix, and the patient immediately
underwent a subsequent hemicolectomy. The final histological
examination confirmed the presence of a primary appendiceal
mucinous adenocarcinoma infiltrating the appendix and urinary
bladder wall. The pathological staging was as follows: TNM
classification, pT4N0M0; and Dukes’, Astler-Coller classification,
stage B.
Discussion
Histologically, adenocarcinomas of the appendix are
classified into three distinct types: Mucinous, intestinal and
signet ring cell. Various controversies in the field of appendiceal
mucinous neoplasms have arisen over the past several decades,
focusing on the classification of appendiceal mucinous tumors and
the nature, classification and clinical significance of
pseudomyxoma peritonei (11).
Invasive adenocarcinomas of the appendix are rare, accounting for
only 4–6% of primary malignant appendiceal neoplasms, according to
a study by Hananel et al (12). The pre-operative diagnosis of
primary appendiceal carcinoma is invariably difficult since the
clinical presentation is usually non-specific. Therefore,
appendiceal carcinoma is always neglected or misdiagnosed. The
majority of cases are diagnosed during intraoperative exploration
(13,14). The identification of a previously
reported series of appendiceal neoplasms is difficult due to their
rarity and the increased rarity of appendiceal carcinoma cases also
invading the urinary bladder. Taverna et al (9) described the features and rarity of
appendiceal carcinoma invading the urinary bladder. The appendiceal
carcinoma usually involved the posterior bladder wall initially and
subsequently the anterior bladder lesion was a secondary
localization due to the anatomical relationship between the
appendix and the bladder.
In the present case, the patient did not exhibit any
gastrointestinal symptoms, with signs of bladder irritation,
existing since morbidity, the only clinical presentation.
Ultrasound and abdomen enhanced CT scans revealed a urinary bladder
mass. Combined with the laboratory test results and symptoms, an
initial diagnosis of urinary bladder carcinoma was made. However,
from the CT MPR images, the mass was found to connect with the
ileocecal junction, and the density of the liquid content was low.
The region of the lesion was in line with the appendix. Therefore,
the primary diagnosis was changed. It was considered that the
lesion had originated from the intestinal tract, then invaded the
bladder, and that the appendix was the most likely organ of this
origin. This was confirmed by explorative surgery, followed by a
subsequent hemicolectomy due to the frozen section analysis.
In the present case, the patient’s clinical
presentation was confusing and the rarity of an appendiceal
carcinoma invading the urinary bladder led us to initially ignore
the possibility of its presence. The signs and symptoms of an
appendiceal adenocarcinoma were not specifically apparent, but the
CT MPR technique was useful to identify a correlation with the
appendix. Therefore, a diagnosis of a primary appendiceal mucinous
carcinoma must be considered by radiologists and clinicians for
patients who do not exhibit gastrointestinal symptoms, but show
involvement of the nearest organs and the bladder wall. It is
possible that CT MPR images may provide more information.
References
|
1
|
McCusker ME, Coté TR, Clegg LX and Sobin
LH: Primary malignant neoplasms of the appendix: a population-based
study from the surveillance, epidemiology and end-results program,
1973–1998. Cancer. 94:3307–3312. 2002.
|
|
2
|
Berger A: Ein Fall von Krebs des
Wurmfortsatzes. Ber Klin Wochenschr. 19:6101882.(In German).
|
|
3
|
Ko YH, Park SH, Jung CK, et al: Clinical
characteristics and prognostic factors for primary appendiceal
carcinoma. Asia Pac J Clin Oncol. 6:19–27. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pai RK and Longacre TA: Appendiceal
mucinous tumors and pseudomyxoma peritonei: histologic features,
diagnostic problems, and proposed classification. Adv Anat Pathol.
12:291–311. 2005. View Article : Google Scholar
|
|
5
|
Misdraji J and Young RH: Primary
epithelial neoplasms and other epithelial lesions of the appendix
(excluding carcinoid tumors). Semin Diagn Pathol. 21:120–133. 2004.
View Article : Google Scholar
|
|
6
|
Rassu PC, Cassinelli G, Ronzitti F,
Bronzino P, Stanizzi T and Casaccia M: Primary adenocarcinoma of
the appendix. Case report and review of the literature. Minerva
Chir. 57:695–698. 2002.(In Italian).
|
|
7
|
Butler JA, Houshiar A, Lin F and Wilson
SE: Goblet cell carcinoid of the appendix. Am J Surg. 168:685–687.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Petrou A, Papalambros A, Katsoulas N,
Bramis K, Evangelou K and Felekouras E: Primary appendiceal
mucinous adenocarcinoma alongside with situs inversus totalis: a
unique clinical case. World J Surg Oncol. 8:492010. View Article : Google Scholar
|
|
9
|
Taverna G, Corinti M, Colombo P, et al:
Bladder metastases of appendiceal mucinous adenocarcinoma: a case
presentation. BMC Cancer. 10:622010. View Article : Google Scholar
|
|
10
|
Ito H, Osteen RT, Bleday R, Zinner MJ,
Ashley SW and Whang EE: Appendiceal adenocarcinoma: long-term
outcomes after surgical therapy. Dis Colon Rectum. 47:474–480.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Misdraji J: Appendiceal mucinous neoplasm:
controversial issues. Arch Pathol Lab Med. 134:864–870.
2010.PubMed/NCBI
|
|
12
|
Hananel N, Powsner E and Wolloch Y:
Adenocarcinoma of the appendix: an unusual disease. Eur J Surg.
164:859–862. 1998. View Article : Google Scholar
|
|
13
|
Baykal C, Türkmen IC, Hizli F, Doğusoy GB,
Sertep I and Dünder I: Primary mucinous borderline tumor of the
vermiform appendix mimicking ovarian carcinoma: case report. Eur J
Gynaecol Oncol. 33:528–529. 2012.PubMed/NCBI
|
|
14
|
Andreopoulou E, Yee H, Warycha MA, et al:
Mucinous cancer of the appendix: challenges in diagnosis and
treatment. J Chemother. 19:451–454. 2007. View Article : Google Scholar : PubMed/NCBI
|