Introduction
Chilaiditi sign refers to the radiological
observation of segmental interposition of the colon between the
liver and the diaphragm, which was first described by Chilaiditi, a
Greek radiologist, in 1910 (1).
Chilaiditi sign has an incidence of 0.025–0.28% worldwide (2) with a marked male predominance (male to
female, 4:1) (3). Chilaiditi sign
may be asymptomatic or may be accompanied by a series of clinical
symptoms, including digestive symptoms, which range from mild
abdominal pain to acute bowel obstruction and is termed Chilaiditi
syndrome (4). The management of
Chilaiditi syndrome includes conservative treatment and surgical
intervention. Chilaiditi syndrome is often misdiagnosed in clinical
practice due to its rarity, particularly in China. The current
study presents a patient with Chilaiditi syndrome who was treated
in January 2012, in addition to a review of seven cases of
Chilaiditi syndrome obtained from the Chinese literature between
1990 and 2013. The pathogenesis, clinical manifestation, diagnosis
and treatment of Chilaiditi syndrome are analyzed and discussed.
The patient provided written informed consent.
Case report
Case report
A 47-year-old male was admitted to the Emergency
Department of the Second Affiliated Hospital, Zhejiang University
(Hangzhou, China) in January 2012, presenting >40 years of
intermittent upper abdominal pain and the absence of flatus for six
days. The symptoms were associated with abdominal distension,
nausea and vomiting, which were relieved by a change of posture or
a sudden movement. The patient had no history of surgery. The
physical examination revealed a soft abdomen with mild upper
abdominal tenderness; no rebound tenderness or muscle guarding was
identified. In addition, auscultation revealed hypoactive bowel
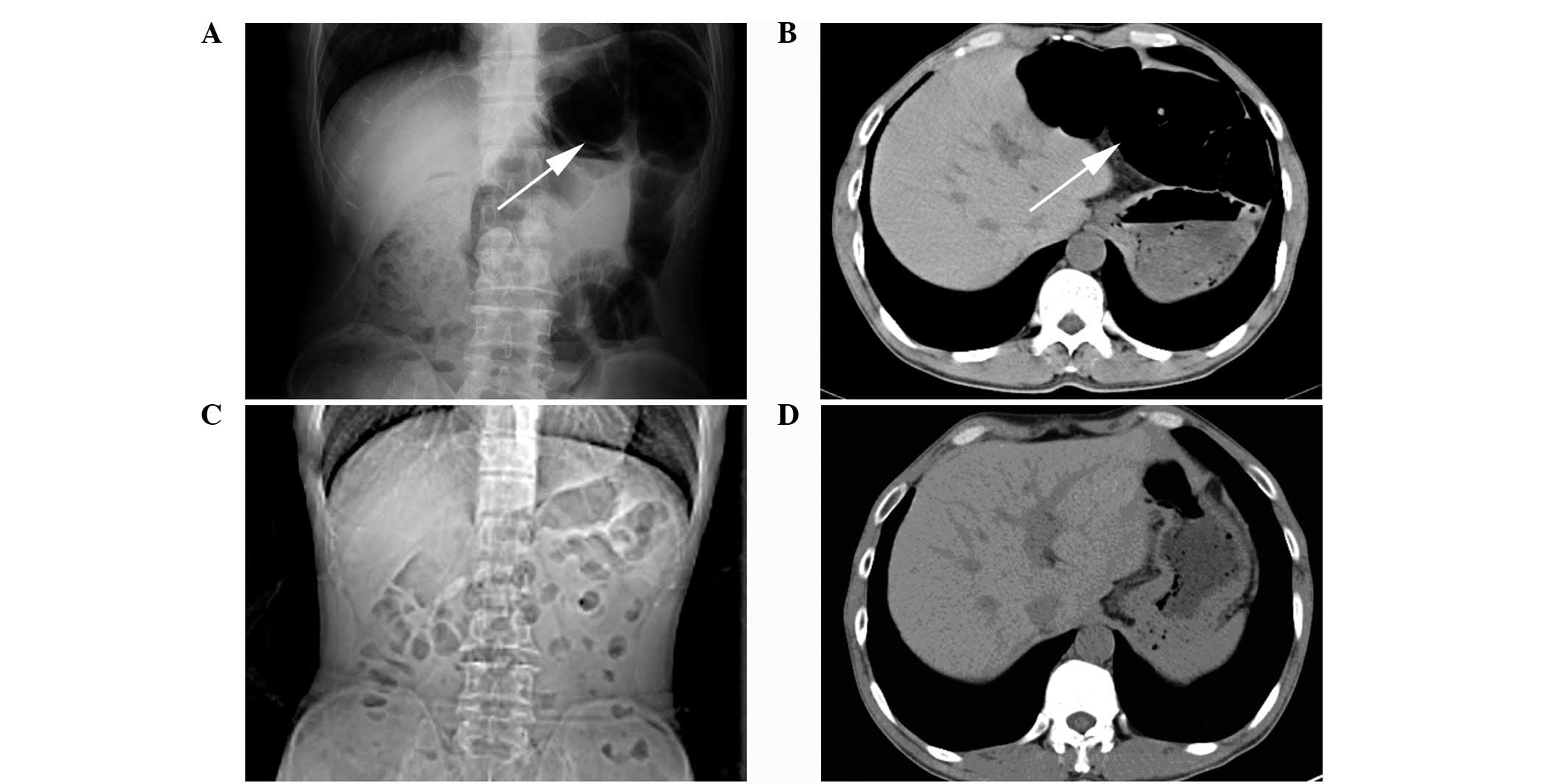
sounds. A plain abdominal X-ray showed an abnormal gas shadow in
the left subphrenic space and a segment of gaseous distended colon,
which was located in the left side of the abdominal cavity; this
was interposed between the liver and the left diaphragm, which
indicated a large bowel obstruction (Fig. 1A). Computed tomography (CT)
confirmed the interposition of the colon (Fig. 1B) accompanied by the small bowel
distention with several air-fluid levels. The patient was treated
conservatively with fasting, nasogastric decompression, fluid
supplementation, parenteral nutrition, enemas and the application
of somatostatin. Six days later, the patient was able to pass
stools and tolerate a liquid diet. After one week, CT was performed
again, which showed normal organ morphology in the left upper
quadrant and identified that the distended colon between the liver
and the diaphragm was restored to its normal position. In addition,
the air-fluid levels in the small bowel had also disappeared
(Fig. 1C and D). The patient
received no further surgical treatment and no evidence of
recurrence was found during the one year of follow-up.
Literature review
The Chinese Biology and Medicine Database
(http://sinomed.imicams.ac.cn/zh/), the
Chinese Periodical Database of Science and Technology (http://lib.cqvip.com/), and the China Hospital
Knowledge Database (http://www.chkd.cnki.net) were searched for cases of
Chilaiditi syndrome between January 1990 and January 2013.
Duplicate reports were excluded to avoid over-representation and
seven cases of Chilaiditi syndrome, as reported in the Chinese
literature (5–9) were identified (Table I).
 | Table IClinical data of seven cases. |
Table I
Clinical data of seven cases.
| First author (year)
[ref] | Age (years) | Gender | Clinical
manifestation | Auxiliary
examination | Complication | Treatment |
|---|
| Wang et al
(2012) [5] | 48 | Female | Abdo pain and
constipation | Chest X-ray and
CT | Atrophy of right
liver lobe | Right
hemicolectomy |
| Hu (2007) [6] | 70 | Male | Abdo pain and bloody
stools | Abdo X-ray and
CT | Rectal cancer | Exploratory
laparotomy |
| Hu (2007) [6] | 60 | Male | Mass in left lower
quadrant | Abdo CT | Mesenteric
lymphosarcoma | Exploratory
laparotomy |
| Cui et al
(2012) [7] | 65 | Male | Abdo pain | Abdo CT | None | Conservative |
| Su et al
(2005) [8] | 62 | Female | Abdo pain and
constipation | Abdo X-ray and
CT | None | Conservative |
| Su et al
(2005) [8] | 75 | Female | Abdo pain and
constipation | Chest and abdo X-ray
and CT | None | Conservative |
| Shen (2000) [9] | 39 | Male | Abdo pain | Abdo CT | Congenital liver
split | Conservative |
The median age of the seven patients at presentation
was 60 years (range, 39–75 years) and the male to female ratio was
4:3. The shortest duration of the symptoms was ~5 h of acute bowel
obstruction in a 39-year-old male, and the longest was >40 years
in a patient who presented with repeated abdominal pain and
constipation. The most frequent symptom of Chilaiditi syndrome was
abdominal pain (n=6/7) with abdominal tenderness (n=3/7). All of
the cases were diagnosed by CT, in which the distension of the
colon interposed between the liver and the diaphragm was revealed.
One patient exhibited atrophy of the right lobe of the liver and an
additional patient exhibited the anatomic abnormality of a
congenital liver split. In addition, a plain abdominal or chest
X-ray was performed (n=4/7), which showed a bowel shadow in the
subphrenic space. The treatment included conservative treatment
(n=4/7) and surgical intervention (n=3/7). The conservative
treatment included fasting, nasogastric decompression, fluid
supplementation, enemas, peristalsis stimulation, traditional
Chinese medicine (auricular acupressure of Vaccaria) and
acupuncture. One patient underwent a right hemicolectomy and during
surgery, an exceptionally elongated and distended right colon was
revealed. Furthermore, a dense adhesion was identified between the
colon and the lower edge of the right hepatic lobe as well as
atrophy of the right hepatic lobe. Hu (6) reported two cases of Chilaiditi
syndrome that were identified with malignancies (rectal cancer and
mesenteric lymphosarcoma) during an exploratory laparotomy, in
which extensive peritoneal metastasis, adhesions, laxity of the
right triangular ligament, and the insertion of a distended
transverse colon between the liver and the diaphragm were revealed.
The seven patients recovered well with the exception of the cases
that were accompanied by a malignancy. The follow-up data were only
available for one case that demonstrated no evidence of recurrence
for one month.
Discussion
Intestinal interposition is a medical condition
where a segment of the bowel is temporarily or permanently
interposed between two organs, for example the liver and the
diaphragm, the spleen and the diaphragm, the spleen and the left
kidney or the stomach and the pancreas. Among these, the
hepatodiaphragmatic interposition is termed Chilaiditi sign and the
others are termed non-Chilaiditi sign (10). The interposed bowel is usually the
hepatic flexure of the colon and much less frequently the small
bowels, which occurs in 3–5% of Chilaiditi sign cases (11). Chilaiditi sign is usually revealed
incidentally by chest or abdominal radiographs, with an incidence
of 0.025–0.28%. In addition, Chilaiditi sign is usually
asymptomatic and when accompanied with clinical symptoms is termed
Chilaiditi syndrome. The incidence of Chilaiditi syndrome rises
with increasing age (12) and has a
marked male predominance (male to female ratio, 4:1) (3).
Normally, suspensory ligaments and fixation of the
colon impede the interposition of the colon between the liver and
the diaphragm. However, various factors have been implicated that
result in the pathological interposition of the colon, these
include hepatic, intestinal, diaphragmatic and other miscellaneous
causes. A large space between the liver and the diaphragm may
potentially lead to colonic interposition (13). Additional factors include those
relating to the intestines, such as megacolon, an
elongated/hypermobile colon with constipation (5), absence/laxity/elongation of the
ligament suspending the transverse colon, abnormal gas accumulation
due to aerophagia. The diaphragmatic factors include the rise of
the right hemidiaphragm, such as eventration or phrenic nerve
injury, and the hepatic factors include atrophy of the liver due to
cirrhosis or congenital etiology (for example a congenital liver
split or relaxation/elongation of suspensory ligaments). Other
factors include enlargement of the lower thoracic cavity (chronic
obstructive pulmonary disease), increased intra-abdominal pressure
(obesity, multiple pregnancies and ascites), mental retardation and
schizophrenia, which are also associated with anatomic
abnormalities that result in Chilaiditi sign (14). Intraperitoneal adhesion, which is
caused by widespread tumor metastasis or previous surgery is also
one of the factors (6). In
addition, psychotropic medication (15) and iatrogenic factors (16), such as endoscopic procedures, have
been reported as causative factors. In the present case, the
patient exhibited a childhood-onset symptom, therefore,
interposition of the colon was more likely due to a congenital
anatomical anomaly. In addition, the patient had emphysema and
chronic obstructive pulmonary disease, therefore, enlargement of
the lower thoracic cavity may also have been a possible cause.
Chilaiditi syndrome has various clinical
manifestations, such as decreased appetite, abdominal pain,
flatulence, nausea, vomiting and constipation. The seven cases
reviewed in the current study all presented with gastrointestinal
symptoms with the exception of one patient. However, in rare cases,
other symptoms besides those associated with the gastrointestinal
tract, such as respiratory distress and angina-like chest pain, may
also be observed (17) Thus,
Chilaiditi syndrome must be considered in chest pain patients with
electrocardiogram results, cardiac function and cardiac enzymes
within the normal ranges. In addition, Chilaiditi syndrome may also
be an indirect manifestation of certain abdominal malignancies,
with or without peritoneal metastasis. In the present study, two of
the previously reported cases were accompanied with malignancies,
one with rectal cancer and the other with mesenteric lymphosarcoma
(6). The complications of
Chilaiditi syndrome may include intestinal obstruction, volvulus
and perforation. In rare cases perforated subdiaphragmatic
appendicitis may occur as a complication of Chilaiditi syndrome
(18).
A characteristic marker of Chilaiditi sign is the
observation of air below the diaphragm, with visible haustral folds
or valvulae conniventes between the liver and the diaphragmatic
surface. In addition, the location of the air is not changed by
altering the posture of the patient. Chilaiditi sign must be
differentiated from pneumoperitoneum by X-ray. Pneumoperitoneum
normally shows a crescent-shaped gas shadow under the diaphragm
without haustral folds or valvulae conniventes, and altering the
posture of the patient changes the position of the gas. Patients
with pneumoperitoneum always exhibit injury to the hollow viscus
and simultaneously possess signs of peritonitis. Ultrasonography is
also useful in the differentiation of Chilaiditi syndrome from
pneumoperitoneum, which usually requires an immediate surgical
intervention (19).
It is important to identify colonic interposition in
patients that are predisposed to developing Chilaiditi sign, such
as cirrhotic patients, in order to prevent complications during a
percutaneous transhepatic procedure or liver biopsy (14). In addition, colonoscopies must be
performed carefully in patients with Chilaiditi sign to prevent
intestinal perforation.
Interventions are not required for asymptomatic
patients with Chilaiditi sign and the treatment is usually
conservative. The present case and four of the reviewed cases were
all cured by conservative treatment, which included bed rest,
nasogastric decompression, fluid supplementation, enema, laxatives
and the discontinuation of offending medications (for example
psychotropic medications) (20). In
addition, traditional Chinese medicine may be used as an
alternative; the two cases reported by Su et al (8) were cured by acupuncture and auricular
acupressure of Vaccaria. When conservative treatment fails,
the intestinal obstruction, such as volvulus, intestinal ischemia
or intestinal perforation, can not be alleviated and thus, surgical
intervention is required. Saber and Boros (21) previously reported that 26% of
patients require operative management and that the number of
surgical interventions for long-term intermittent abdominal pain
continues to increase. Surgical interventions include segmental
colon resection, colopexy and hepatopexy (15).
In conclusion, Chilaiditi syndrome is rare in China
and may be asymptomatic or present with acute abdominal pain.
Occasionally, Chilaiditi syndrome is associated with malignancies
and may, therefore, be misdiagnosed. The present study allows
clinicians to become familiarized with this syndrome and its
management, in order to avoid a misdiagnosis during clinical
treatment.
References
|
1
|
Chilaiditi D: On the question of
hepatoptosis ptosis and generally in the exclusion of three cases
of temporary partial liver displacement. Fortschr Geb Röntgenstr
Nuklearmed. 11:173–208. 1910.(In German).
|
|
2
|
Alva S, Shetty-Alva N and Longo WE: Image
of the month. Chilaiditi sign or syndrome. Arch Surg. 143:93–94.
2008.
|
|
3
|
Yin AX, Park GH, Garnett GM and Balfour
JF: Chilaiditi syndrome precipitated by colonoscopy: a case report
and review of the literature. Hawaii J Med Public Health.
71:158–162. 2012.
|
|
4
|
Lekkas CN and Lentino W: Symptom-producing
interposition of the colon. Clinical syndrome in mentally deficient
adults. JAMA. 240:747–750. 1978. View Article : Google Scholar
|
|
5
|
Wang DD, Wang ZL and Qiao HQ: One case
report of Chilaiditi syndrome. Zhonghua Wei Chang Wai Ke Za Zhi.
5:4472012.(In Chinese).
|
|
6
|
Hu JL: Diagnosis, differential diagnosis
and clinical significance of hepatodiaphragmatic interposition of
the colon. Hai Nan Yi Xue Bian Ji Bu. 8:1452007.(In Chinese).
|
|
7
|
Cui MJ, Wei LZ and Niu QH: Chilaiditi
syndrome: one case report. Wei Chang Bing Xue He Gan Bing Xue Za
Zhi. 5:486–487. 2012.
|
|
8
|
Su SH, Yang J and Hu YT: Misdiagnosis
analysis of the Chilaiditi syndrome of two old patients. Zhong Guo
Zong He Lin Chuang. 8:7682005.(In Chinese).
|
|
9
|
Shen YQ: One case of congenital liver
split with hepatodiaphragmatic interposition of the colon.
Guangdong Yi Xue. 10:8572000.(In Chinese).
|
|
10
|
Bredolo F, Esposito A, Casiraghi E,
Cornalba G and Biondetti P: Intestinal interposition: the
prevalence and clinical relevance of non-hepatodiaphragmatic
conditions (non-Chilaiditi forms) documented by CT and review of
the literature. Radiol med. 116:607–619. 2011. View Article : Google Scholar
|
|
11
|
Vessal K and Borhanmanesh F:
Hepatodiaphragmatic interposition of the intestine (Chilaiditi’s
syndrome). Clin Radiol. 27:113–116. 1976.
|
|
12
|
Schubert SR: Chilaiditi’s syndrome: an
unusual cause of chest or abdominal pain. Geriatrics. 53:85–88.
1998.
|
|
13
|
Oh SN, Rha SE, Byun JY, Kim JY, Song KY
and Park CH: Chilaiditi syndrome caused by Fitz-Hugh-Curtis
syndrome: multidetector CT findings. Abdom Imaging. 31:45–47. 2006.
View Article : Google Scholar
|
|
14
|
Moaven O and Hodin RA: Chilaiditi
syndrome: a rare entity with important differential diagnoses.
Gastroenterol Hepatol (NY). 8:276–278. 2012.
|
|
15
|
Blevins WA, Cafasso DE, Fernandez M and
Edwards MJ: Minimally invasive colopexy for pediatric Chilaiditi
syndrome. J Pediatr Surg. 46:e33–e35. 2011. View Article : Google Scholar
|
|
16
|
Aldoss IT, Abuzetun JY, Nusair M, Suker M
and Porter J: Chilaiditi syndrome complicated by cecal cerforation.
South Med J. 102:841–843. 2009. View Article : Google Scholar
|
|
17
|
Sorrentino D, Bazzocchi M, Badano L, Toso
F and Giagu P: Heart-touching Chilaiditi’s syndrome. World J
Gastroenterol. 11:4607–4609. 2005.
|
|
18
|
Lenz M, Kindler M, Schilling M, Pollack T,
Schwab W and Becker M: Chilaiditi’s syndrome complicated by
subdiaphragmatic perforated appendicitis: unusual manifestation of
a rare condition. Chirurg. 82:830–833. 2011.(In German).
|
|
19
|
Lin CH, Yu JC, Ou JJ, Lee YT, Huang M and
Wu HS: Chilaiditi syndrome: the pitfalls of diagnosis. Surg Sci.
3:141e42012.
|
|
20
|
Lohr CE, Nuss MA, McFadden DW and Hogg JP:
Laparoscopic management of Chilaiditi’s syndrome. Surg Endosc.
18:3482004.
|
|
21
|
Saber AA and Boros MJ: Chilaiditi’s
syndrome: what should every surgeon know? Am Surg. 71:261–263.
2005.
|