Introduction
Leiomyosarcoma is a rare, malignant connective
tissue tumor that originates from smooth muscle cells and accounts
for ~7% of all soft-tissue sarcomas (1). Leiomyosarcoma has a poor prognosis due
to its high metastatic recurrence rate and is relatively resistant
to radiation and chemotherapy. In the majority of cases, the tumor
most frequently arises in the uterus, gastrointestinal tract,
retroperitoneum and the subcutaneous tissue of the extremities
(2,3). The most commonly reported sites of
metastasis from leiomyosarcoma are the lungs, liver, kidney, brain
and skin. Spinal metastases of leiomyosarcoma have rarely been
reported, and all cases have been located in the thoracic and
lumbar spinal regions (4). The
surgical treatment for spinal metastases of leiomyosarcoma may be a
considered in situations involving mechanical instability and
neural compression, and is regarded as palliative, with the aim of
improving the patient’s quality of life.
The present study describes a case of leiomyosarcoma
metastasizing to the cervical spine in a 45-year-old male with
neurological deficits. The surgical technique that was used is also
described. To the best of our knowledge, this is the first case of
leiomyosarcoma recurrence presenting in the cervical spine. Patient
provided written informed consent.
Case report
A 45-year-old male was admitted to the First
Affiliated Hospital of Soochow University (Suzhou, China)
presenting with neck pain radiating into the left arm and numbness
that had persisted for five months. The pain was slowly increasing
in strength and was unresponsive to analgesics. The patient’s
medical history included the surgical resection of a mass in the
left thigh eight months prior to admittance, from which
leiomyosarcoma was histologically diagnosed. Upon physical
examination, palpation over the spinous process of C6 elicited
severe pain, and mild hypoesthesia on the ulnar side of the left
upper extremity was detected.
Laboratory examinations did not reveal any abnormal
findings. The plain radiographs, however, revealed a compression
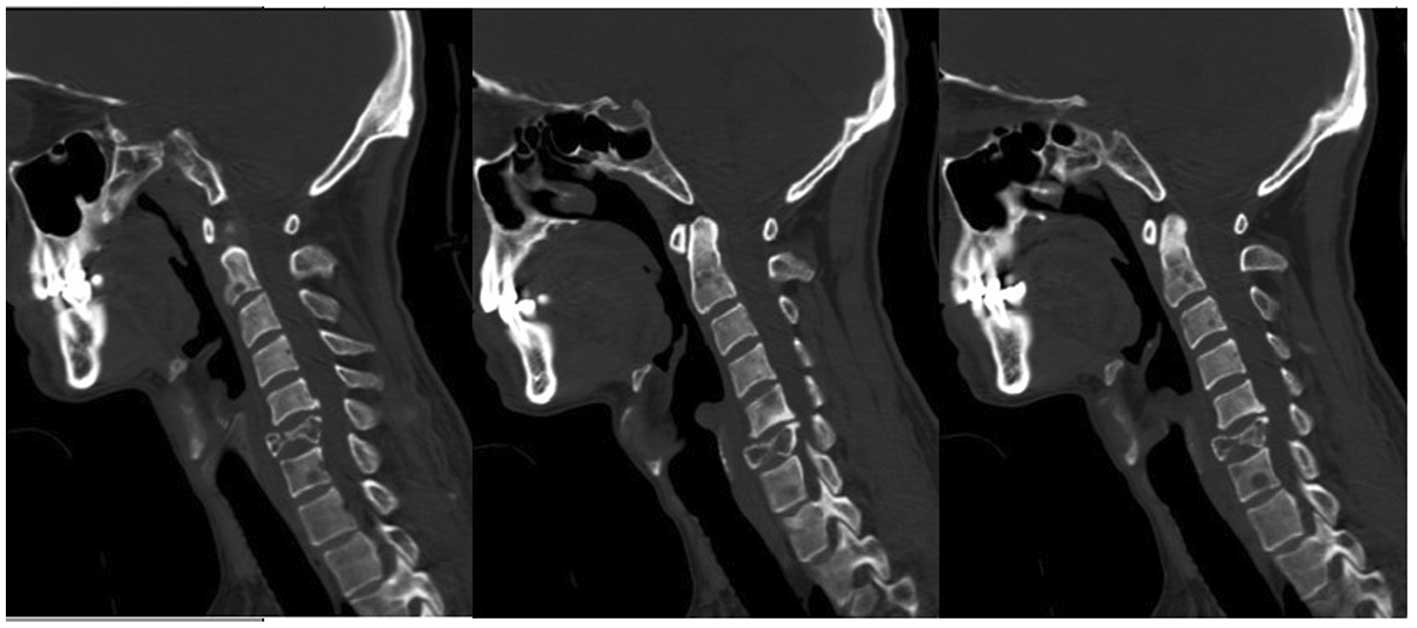
fracture of the C6 vertebral body. Computed tomography (CT) scans
of the cervical spine (Fig. 1)
revealed osteolytic lesions of numerous vertebrae (C2, C3, C4, C5,
C6, C7, T1 and T2). In the case of the C6 vertebra, total
destruction of the vertebral body resulted in vertebral collapse
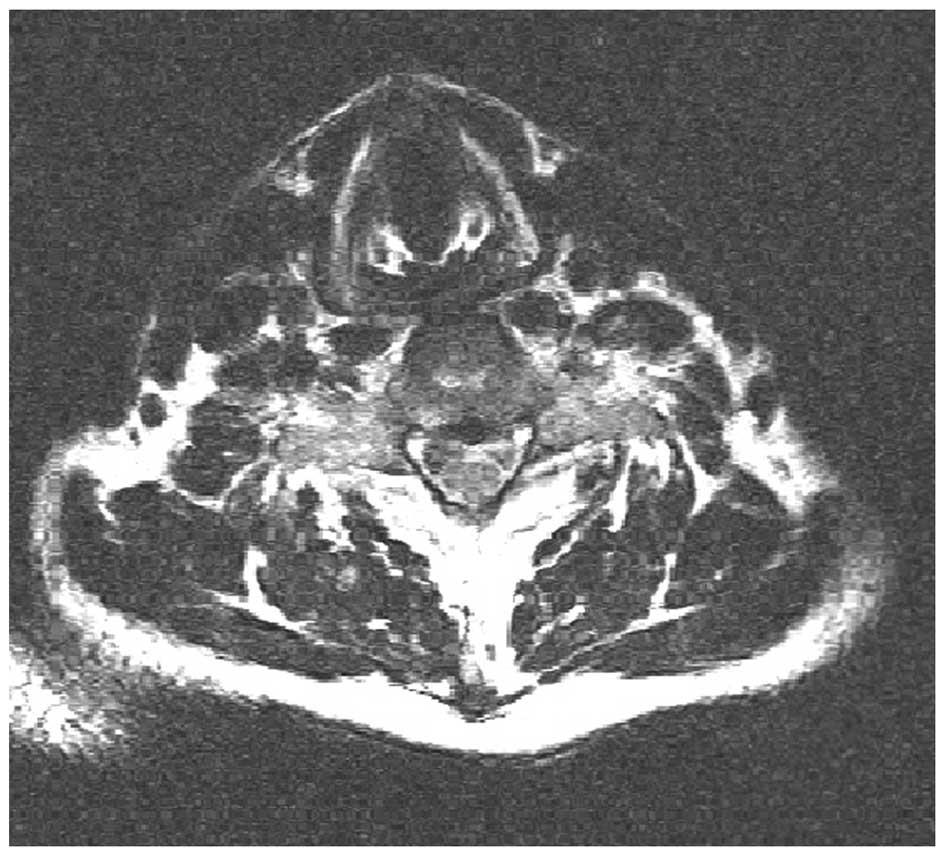
and subsequent spinal cord compression. Magnetic resonance imaging
showed that the lesions were of low signal intensity on T1-weighted
images and high signal intensity on T2-weighted images, and that
the spinal cord at the level of the C6 spine was compressed
(Fig. 2). Further CT scans of the
chest also detected metastatic lesions in the lungs. Therefore,
spinal metastases of leiomyosarcoma were diagnosed and
decompressive surgery was selected as the therapeutic strategy.
Under general anesthesia, the patient was placed in
the supine position, where the neck was slightly extended. The
cervical spine was approached through a right-sided transverse skin
incision. Following discectomies of C5/C6 and C6/C7, a C6
corpectomy was performed. The surgical specimen presented a
grayish-white and infiltrative tumor occupying the C6 vertebral
body. A frozen section was obtained intraoperatively and a
subsequent diagnosis of leiomyosarcoma was formed. Following the
placement of a titanium mesh cage filled with polymethyl
methacrylate (PMMA) cement, the C5 and C7 vertebrae were injected
with cement through a screw tract using a 5-ml syringe when the
cement was at the ‘toothpaste-like’ phase. The selected screw was
then inserted into the tract immediately following the cement
injection.
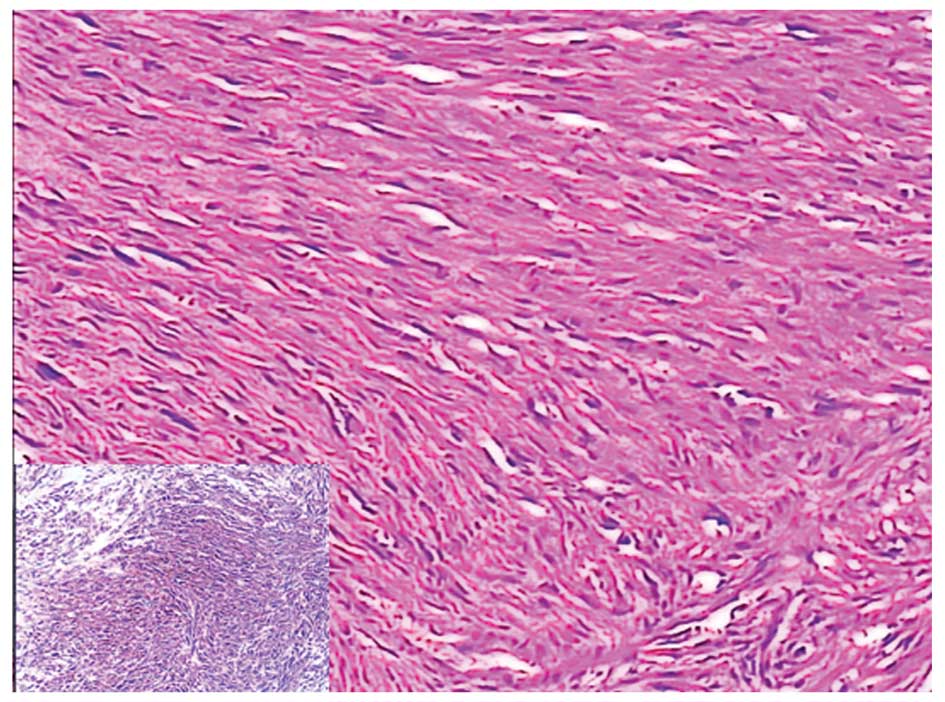
Pathological examination of the specimen revealed a
proliferation of atypical spindle cells surrounded by
fibrocollagenous tissue (Fig. 3).
Immunohistochemical staining was positive for desmin and smooth
muscle actin (Fig. 3 inset), and
negative for S-100 protein, cluster of differentiation (CD)34 and
CD56. Based on the microscopic and immunochemical findings, a
diagnosis of leiomyosarcoma was indicated.
Post-operatively, the pain and numbness
significantly decreased. The patient was transferred to the
Department of Oncology for chemotherapy and radiotherapy. The
chemotherapy consisted of six courses of adriamycin (25
mg/m2, days 1 to 3), every 28 days. Radiotherapy
delivered a total radiation dose of 50 Gy in 25 fractions over five
weeks. A 13-month clinical follow-up examination found that the
patient had experienced only mild numbness of the left hand since
the surgery. In addition, follow-up radiographs revealed that
during this period, no fixation failure or bone cement leakage had
occurred (Fig. 4).
Discussion
Due to their aggressive nature and propensity for
hematogenous spread, leiomyosarcomas have a strong potential for
metastasis to distant sites. Osseous metastases from leiomyosarcoma
are rare; the majority of cases are primary uterine leiomyosarcoma,
while tumors of the stomach, vein and soft tissues have far fewer
recorded incidences of metastasis to the bone (3). Despite the spine being the more common
site of osseous metastasis, the involvement of the cervical spine
in metastatic leiomyosarcoma has, to the best of our knowledge,
never been reported previously. This may be as the cervical spine
is only involved in 8–20% of metastatic spine disease cases
(5), and as leiomyosarcoma
metastasizing to the cervical spine may be a delayed effect and
therefore of lesser clinical significance at the time of
occurrence.
Destructive lesions in numerous vertebrae usually
represent metastases in adult humans. In the present case, multiple
cervical and thoracic vertebrae were involved by osteolytic
lesions. Given the rarity of primary spinal leiomyosarcoma
(6,7) and the patient’s previous history, the
lesions were considered to be of a metastatic type, which was then
confirmed by the pathological examination.
Microscopic examination is a reliable and important
method for the confirmation that a spindle-cell sarcoma in the bone
is in fact a leiomyosarcoma (3).
However, distinguishing leiomyosarcomas from other aggressive
spindle cell malignancies, particularly fibrosarcoma, malignant
fibrous histiocytoma, malignant peripheral nerve sheath tumor and
metastatic spindle cell carcinoma, is not always easy (2–4).
Immunohistochemical studies are often useful in establishing the
diagnosis by demonstrating the smooth muscle cell origin (3,8).
Usually, leiomyosarcoma cells are positive for smooth muscle actin,
weakly positive for desmin and negative for S100 protein.
The prognosis of patients with leiomyosarcoma is
variable depending on the resectability and existence of
metastasis. According to a previous study, patient survival times
range from weeks to 13 years when leiomyosarcoma metastasizes to
the spine (4). Despite numerous
surgeons emphasizing that total resection of the tumor should be
performed to achieve an improved prognosis (4,8,9), this
was considered to be impossible in the patient in the present
study. Therefore, decompressive surgery was selected as the
therapeutic strategy. The surgical technique involved a C6
corpectomy with insertion of an interbody cage and anterior
instrumentation. Given the poor quality of bone in the C5 and C7
vertebrae, resulting from the existence of osteolytic foci, PMMA
was injected into the adjacent vertebral bodies to increase
vertebral and fixation strength. It has previously been
hypothesized that PMMA may have an antitumoral effect (10) and that its space occupying effect
may inhibit tumor cell growth (11). It should be noted that cement
augmentation of the adjacent vertebrae is not a traditional
technique in the treatment of the cervical spine. However, we
believe that it may have been effective in preventing fixation
failure to a certain extent in the present case.
Leiomyosarcoma is known for its relative resistance
to radiotherapy and chemotherapy. However, in cases where total
resection of the lesion has not been established, an additional
therapy, such as radiotherapy and/or chemotherapy, may be required
to improve local control. In the present case, the patient was
referred for radiotherapy and chemotherapy post-operatively, and in
the follow-up examinations the patient exhibited only mild numbness
of the left hand. However, a detailed follow-up evaluation is
required.
Metastases from leiomyosarcoma should be considered
in the differential diagnosis of a patient with multiple vertebrae
destruction, particularly in a patient with a previous history of
leiomyosarcoma. For patients with spinal metastases and
neurological deficits where total resection is impossible,
palliative decompression of the symptom-causing vertebrae is
recommended and stability of the reconstruction should be
guaranteed.
References
|
1
|
Russell WO, Cohen J, Enzinger F, Hajdu SI,
Heise H, Martin RG, Meissner W, Miller WT, Schmitz RL and Suit HD:
A clinical and pathological staging system for soft tissue
sarcomas. Cancer. 40:1562–1570. 1977.
|
|
2
|
Sanerkin NG: Primary leiomyosarcoma of the
bone and its comparison with fibrosarcoma. Cancer. 44:1375–1387.
1979.
|
|
3
|
Shapiro S: Myelopathy secondary to
leiomyosarcoma of the spine. Case report Spine (Phila Pa 1976).
17:249–251. 1992.
|
|
4
|
Elhammady MS, Manzano GR, Lebwohl N and
Levi AD: Leiomyosarcoma metastases to the spine. Case series and
review of the literature. J Neurosurg Spine. 6:178–183. 2007.
|
|
5
|
Fehlings MG, David KS, Vialle L, Vialle E,
Setzer M and Vrionis FD: Decision making in the surgical treatment
of cervical spine metastases. Spine (Phila Pa 1976). 34(Suppl):
S108–S117. 2009.
|
|
6
|
Nanassis K, Alexiadou-Rudolf C and
Tsitsopoulos P: Spinal manifestation of metastasizing
leiomyosarcoma. Spine (Phila Pa 1976). 24:987–989. 1999.
|
|
7
|
Sucu HK, Bezircioğlu H and Rezanko T:
Partial spondylectomy for primary leiomyosarcoma of C2 vertebra.
Spine (Phila Pa 1976). 36:E1422–E1426. 2011.
|
|
8
|
Nishida J, Kato S, Shiraishi H, Ehara S,
Sato T, Okada K and Shimamura T: Leiomyosarcoma of the lumbar
spine: case report. Spine (Phila Pa 1976). 27:E42–E46. 2002.
|
|
9
|
Young CL, Wold LE, McLeod RA and Sim FH:
Primary leiomyosarcoma of bone. Orthopedics. 11:615–618. 1988.
|
|
10
|
Bouza C, López-Cuadrado T, Cediel P,
Saz-Parkinson Z and Amate JM: Balloon kyphoplasty in malignant
spinal fractures: a systematic review and meta-analysis. BMC
Palliat Care. 8:122009.
|
|
11
|
Yang HL, Sun ZY, Wu GZ, Chen KW, Gu Y and
Qian ZL: Do vertebroplasty and kyphoplasty have an antitumoral
effect? Med Hypotheses. 76:145–146. 2011.
|