Introduction
A yolk sac tumor (YST) is a malignant germ cell
tumor (MGCT), which typically occurs in the gonads. Extragonadal
YST is rare, particularly in the retroperitoneum (1). Due to the fact that this tumor occurs
principally in girls and women of childbearing age, the
preservation of fertility is particularly important and maintaining
reproductive function to the greatest extent has become the primary
strategy (2). Prior to the advent
of combination chemotherapy, the prognosis for patients with YST
was poor, with an ~80–90% mortality rate within two years of
diagnosis (3,4). At the end of the 1970s, the prognosis
of YST had improved due to the use of novel chemotherapeutic
regimens. In the 1990s, the combination of bleomycin, etoposide and
cisplatin (BEP) was demonstrated to be highly active against MGCT
and became the standard treatment for this type of tumor (5–7).
However, the prognosis for YST remains unsatisfactory. Recent
studies have demonstrated that the FIGO stage and tumor-reductive
surgery strongly affect the prognosis of this disease (8). Other YST prognosis factors remain
unclear.
The YST represents a highly malignant germ cell
neoplasm in adult cases and is generally characterized by a high
serum α-fetoprotein (AFP) level. Serum AFP is one of the hallmarks
of YST and facilitates its diagnosis. The serial measurement serum
AFP is useful for monitoring its clinical course and response to
treatment (9).
Extragonadal germ cell tumors are considered to be a
consequence of the mismigration of germ cells along the urogenital
ridge during embryogenesis and are estimated to represent ~2–5% of
all adult germ-cell malignancies (9). Extragonadal germ cell tumors are
normally located in the mediastinum, retroperitoneum and other
locations such as the pineal gland or sacrococcygeal area (9). Extragonadal YSTs located in the
retroperitoneum are particularly rare (1). Thus, the histogenesis of primary
retroperitoneal YST (PRYST) remains controversial and the
appropriate treatment is currently unclear. This study presents a
case of YST in the retroperitoneum. Patient provided written
informed consent.
Case report
A 19-year-old female presented with abdominal
distension and edema in the lower limbs for six months. The patient
was admitted to Chunan Chinese Traditional Medical Hospital
(Hangzhou, China) and an abdominal computed tomography (CT) scan
revealed a solid mass located in the retroperitoneum (tumor size,
20×25×30 cm). A palliative tumor resection was performed during the
first exploratory laparotomy on October 28, 2009; the large pelvic
mass was not completely removed and widespread metastasis was
found. The histopathology report revealed a malignant
retroperitoneal tumor (although a YST was initially considered) and
two cycles of single-agent mitomycin (10 mg) chemotherapy were
performed by intraoperative intraperitoneal and intravenous
administration.
The patient was transferred to the Zheijiang Cancer
Hospital (Hangzhou, China) on November 17, 2009. The α-fetoprotein
(AFP) serum levels were elevated to 9,859.76 ng/ml (normal level,
<10 ng/ml); cancer antigen 125 (CA-125) levels were elevated to
51.90 U/ml (normal level, <35 U/ml); the serum β-human chorionic
gonadotropin (β-hCG; normal level, <10 mIU/ml), carcinoembryonic
antigen (CEA; normal level, <5.0 ng/ml), carbohydrate antigen
19-9 (CA 19-9; normal level, <37 U/ml) and squamous cell
carcinoma (SCC) antigen (normal level, <1.5 ng/ml) were within
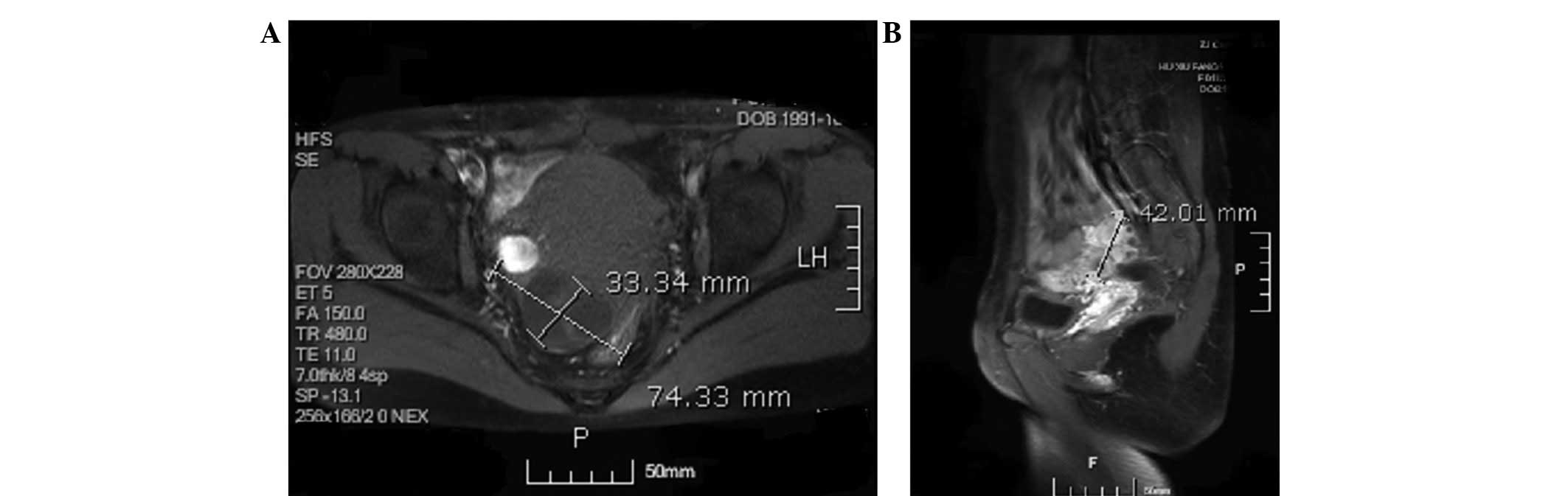
the normal ranges. A pelvic CT scan revealed a pelvic mass (tumor
size, 7.4×9.3 cm; Fig. 1) and an
upper abdomen CT showed multiple enlargements of the
retroperitoneal lymph nodes.
Following two cycles of chemotherapy consisting of
bleomycin (15 mg for three consecutive days), etoposide (150 mg for
four consecutive days) and cisplatin (40 mg for three consecutive
days; termed a BEP regimen), the serum AFP levels decreased to
1,251.27 ng/ml on January 7, 2010 and the CT scan revealed that the
tumor size had significantly reduced (Fig. 2). The interval debulking and
fertility-sparing surgeries (unilateral left side
salpingo-oophorectomy, omentectomy and intumescent lymph node
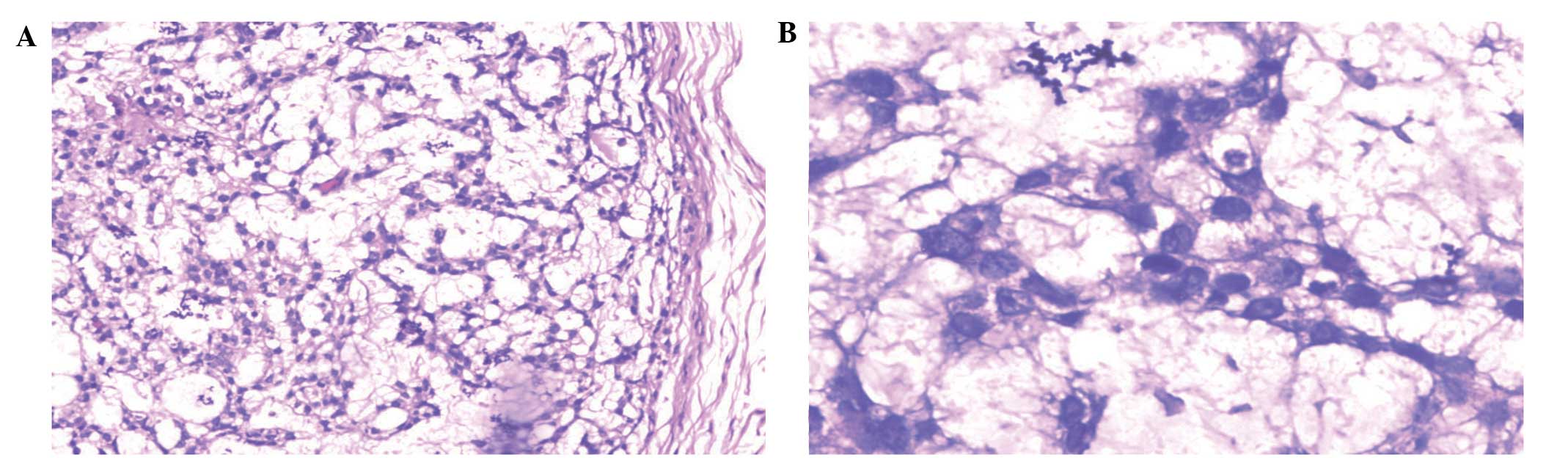
resection) were performed on January 12, 2010. No residual tumor
was found and the histopathology report showed a marginal quantity
of tumor tissue in the pelvic floor and no positive lymph nodes
(Fig. 3). Following surgery, an
additional two cycles of chemotherapy, consisting of the
aforementioned BEP regimen, were administered continuously.
Following surgery and an additional two cycles of the BEP regimen,
the serum AFP levels decreased to 8.17 ng/ml following the final
administration of the BEP regimen on February 28, 2010.
However, tumor recurrence occurred three months
after the final BEP regimen. The serum AFP levels elevated to
193.99 ng/ml on June 4, 2010 and magnetic resonance imaging (MRI)
revealed a cystic and solid mass in the right parametrium (Fig. 4). A salpingostomy and secondary
cytoreductive surgery were performed on June 11, 2010. No residual
tumor was found and the histology report showed metastatic or
invasive malignant tumors (although a YST was initially considered)
on the surface of the sigmoid colon and the rectum (Fig. 5). The patient underwent three cycles
of chemotherapy consisting of bleomycin (15 mg for three
consecutive days), vincristine (1.5 mg on day one) and cisplatin
(40 mg for three consecutive days; termed a BVP regimen) and three
cycles of chemotherapy consisting of vincristine (1.5 mg one day
one) and cisplatin (40 mg for three consecutive days; termed a VP
regimen). Following the final VP regimen on October 11, 2010, the
AFP level decreased to 2.59 ng/ml and the CA-125, β-hCG, CEA, CA
19-9 and SCC were within the normal ranges.
However, tumor recurrence occurred just three months
following the final BVP regimen. The serum AFP level elevated to
72.80 ng/ml on January 10, 2011 and the CT scan revealed that the
cystic and solid mass in the right parametrium had markedly
increased (compared with the prior MRI) (Fig. 6). Radical surgery (hysterectomy,
unilateral right side salpingo-oophorectomy and right pelvic
lymphadenectomy) was performed on January 18, 2011. No residual
tumor was found and the histopathology report showed spindle cells
(although a YST was initially considered) on the surface of the
small intestine (Fig. 7).
Following surgery, the patient received two cycles
of chemotherapy consisting of vincristine (1 mg on day one),
actinomycin D (400 μg for five consecutive days) and
cyclophosphamide (200 mg for three consecutive days; termed a VAC
regimen). However, the serum AFP level increased to 465.27 ng/ml
following the final VAC regimen on March 14, 2011 and the positron
emission tomography/CT revealed tumor metastases to the liver and
the spleen. Therefore, the patient was administered three cycles of
chemotherapy consisting of taxol® (210 mg on day one),
ifosfamide (2 g on day one and 1 g on days two and three) and
cisplatin (70 mg on day one; termed a TIP regimen), while the serum
AFP level continuously increased to 3,500.01 ng/ml following the
final TIP regimen on May 23, 2011. The patient presented with liver
and spleen metastases and succumbed to cachexia 21 months after
diagnosis.
Discussion
PRYST is an extremely rare tumor that, to the best
of our knowledge, has only previously been described in case
reports. There are no specific clinical symptoms and signs of
PRYST; thus, the tumor is commonly identified when it has grown to
a considerable size. In the majority of cases, the tumor has
invaded the crucial nerves and blood vessels, such as the abdominal
aorta, inferior vena cava and may have formed tumor thrombus in the
vena cava. It is particularly difficult to manage these cases;
however, complete resection of retroperitoneal tumors is crucial
for successful treatment. DiPerna et al (10) indicated that the resection of
tumors, which are invading major vascular structures, may provide
an acceptable morbidity and mortality among patients. Maintaining
the female reproductive function to the greatest extent has become
the primary strategy, during the treatment of gynecological cancer,
for prolonging survival and improving patient quality of life. The
reproductive function may be retained provided that the uterus and
the contralateral ovary remain intact, regardless of the tumor
stage (3). Cicin et al
(2) considered that
fertility-sparing surgery was as effective as radical surgery in
patients with an ovarian YST. Peccatori et al (11) retrospectively analyzed 129 patients
with malignant ovarian germ cell tumors and found that
fertility-sparing surgery did not affect recurrence or survival
rate in patients with ovarian germ cell tumors. Ayhan et al
(12) analyzed 45 patients with all
stages of dysgerminomas and found no significant difference between
conservative and non-conservative surgery in recurrence or survival
rate of patients. Furthermore, Zanagnolo et al (13) reported that fertility-sparing
surgery was safe for patients with malignant ovarian germ cell
tumors. In the present case, four different surgical procedures,
including palliative, interval debulking, fertility-sparing,
secondary cytoreductive and radical surgeries, and a salpingostomy,
were performed. The serum AFP level markedly decreased following
all the procedures except radical surgery. Although the PRYST
relapsed, the present study indicated that surgical resection is
the optimal treatment modality for PRYSTs, particularly when
performed prior to PRYST recurrence.
AFP is an important tumor marker of YST; an
increased serum AFP level is typically observed in patients
presenting with a YST and exhibits a good correlation with the
severity of the lesion. Serum AFP levels decrease rapidly following
tumor resection, however, the levels increase during tumor
recurrence or metastasis. Talerman et al (14) reported that serial serum AFP may be
used for diagnostic purposes, and the detection of metastases and
recurrence. In the present case, the serum AFP level decreased from
9,859.76 ng/ml to 8.17 ng/ml following interval debulking surgery,
fertility-sparing surgery and the BEP chemotherapy regimen; and
decreased from 193.99 ng/ml to 2.59 ng/ml following salpingostomy,
secondary cytoreductive surgery, and the BVP and VP chemotherapy
regimens. By contrast, the serum AFP level increased from 8.17
ng/ml to 193.99 ng/ml following the first tumor recurrence, and
from 2.59 ng/ml to 72.80 ng/ml following the second tumor
recurrence. Therefore, AFP is an important tumor marker for
monitoring tumor recurrence and may be used to assess preoperative
or postoperative residual tumors, monitor the response to
chemotherapy treatment and contribute to long-term follow-up.
Since the 1980s, various platinum-based chemotherapy
regimens (such as BEP and BVP) have been widely used and have
markedly improved the prognosis of patients with MGCTs. The
administration of cisplatin-based combination chemotherapy regimens
has improved the curative effect on MGCT patients. Cicin et
al (2) reported that the most
decisive prognostic factors in patients with ovarian YST were
optimal cytoreductive surgery and the standard BEP regimen. In
addition, cisplatin-containing chemotherapy has markedly improved
the outlook for patients with MGCT and overall cure rates are
>80% (15). The BEP regimen
became the most effective treatment for MGCTs after the 1990s and
is considered to be the first-line chemotherapy regimen for MGCTs
(1,15). In the present study, the BEP regimen
appeared to be an effective treatment strategy for the PRYST even
when the tumor was not completely resected. The serum AFP level
markedly decreased (from 9,859.76 ng/ml to 8.17 ng/ml) following
four courses of BEP chemotherapy. In addition, the BVP and VP
regimens also proved effective following tumor recurrence. The
serum AFP level markedly decreased (from 193.99 ng/ml to 2.59
ng/ml) following three cycles of BVP and VP regimens (the BVP
regimen was replaced by the VP regimen as the patient had received
the life-time dose of bleomycin).
The VAC and TIP regimens are classic chemotherapy
regimens for germ cell tumors. Lertkhachonsuk et al
(16) reported that the VAC regimen
was effective for patients with MGCTs. Park et al (17) demonstrated that TIP chemotherapy was
a well-established and active regimen for patients with relapsed
germ cell tumors as a salvage treatment. In the present study, the
patient was considered to be a cisplatin-refractory case as,
following BEP, BVP and VP regimens, the patient experienced
complete remission (defined as no residual tumor and a normal serum
AFP level) for approximately three months after each treatment
(from February 28 to June 4, 2010 and from October 11, 2010 to
January 10, 2011). Thus, as a result of the tumor recurrence, the
chemotherapy regimen was altered to the VAC regimen; however, the
VAC regimen appeared to be ineffective. Consequently, the
chemotherapy regimen was altered again and the TIP regimen was
administered which was also ineffective. Accordingly, the
platinum-based chemotherapy regimens remain effective for PRYST
patients even when there is a tumor relapse following the first
platinum-based chemotherapy. By contrast, platinum-based
chemotherapy regimens and other regimens may not be effective in
the case of a cisplatin-refractory patient where the tumor relapses
more than once.
Approximately 10–20% of patients experience a YST
relapse following the first treatment (13,18)
and their AFP levels may be associated with tumor recurrence and
prognosis. Mitchell et al (4) reported that relapses were principally
observed among patients with an AFP level >1,000 ng/ml. With
regards to the prognosis of YST, Mayordomo et al (19) reported that a serum AFP level of
>1,000 ng/ml was a prognostic factor in patients with ovarian
and extragonadal MGCTs. de La Motte Rouge et al (20) retrospectively analyzed 84 patients
with ovarian YST and found that a decline in the serum AFP level
may be a poor prognostic factor. Moreover, high serum AFP levels
may be associated with a worse prognosis in patients with MGCTs
(4,19); however, these studies that
explicitly evaluated the significance of serum AFP levels in an
ovarian YST series failed to illustrate that this was a prognostic
factor (3,4,8–22). In
the present case, the serum AFP level increased from 72.80 ng/ml to
3,500.01 ng/ml during VAC and TIP chemotherapy, which indicated a
poor prognosis regardless of radical surgery.
In conclusion, the current study presented a rare
case of YST originating in the retroperitoneum. PRYST is an
extremely rare malignant tumor with a poor prognosis. Although
PRYST may relapse promptly after surgical treatment, surgical
resection is considered to be the optimal treatment, particularly
when performed prior to PRYST recurrence, as it markedly decreases
the AFP level. In addition, it was observed that the BEP, BVP and
VP chemotherapy regimens are effective for patients with PRYST even
when the tumor is not completely resected. Thus, AFP is an
important tumor marker for monitoring PRYST recurrence and the
observation of elevated serum AFP levels during chemotherapy
indicate a poor prognosis.
Abbreviations:
|
YST
|
yolk sac tumor
|
|
PRYST
|
primary retroperitoneal yolk sac
tumor
|
|
AFP
|
α-fetoprotein
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
|
MGCT
|
malignant germ-cell tumors
|
|
BEP
|
bleomycin, etoposide and cisplatin
|
|
BVP
|
bleomycin, vincristine and
cisplatin
|
|
VP
|
vincristine and cisplatin
|
|
VAC
|
vincristine, actinomycin D and
cyclophosphamide
|
|
TIP
|
taxol, ifosfamide and cisplatin
|
References
|
1
|
Bokemeyer C, Nichols CR, Droz JP, et al:
Extragonadal germ cell tumors of the mediastinum and
retroperitoneum: results from an international analysis. J Clin
Oncol. 20:1864–1873. 2002.
|
|
2
|
Cicin I, Saip P, Guney N, et al: Yolk sac
tumors of the ovary: evaluation of clinicopathological features and
prognostic factors. Eur J Obstet Gynecol Reprod Biol. 146:210–214.
2009.
|
|
3
|
Kurman RJ and Norris HJ: Malignant germ
cell tumor of the ovary. Hum Pathol. 8:551–564. 1977.
|
|
4
|
Mitchell PL, Al-Nasiri N, A’Hern R, et al:
Treatment of nondysgerminomatous ovarian germ cell tumors: an
analysis of 69 cases. Cancer. 85:2232–2244. 1999.
|
|
5
|
Gershenson DM, Morris M, Cangir A, et al:
Treatment of malignant germ cell tumours of the ovary with
bleomycin, etoposide, and cisplatin. J Clin Oncol. 8:715–720.
1990.
|
|
6
|
Williams S, Blessing JA, Liao SY, et al:
Adjuvant therapy of ovarian germ cell tumours with cisplatin,
etoposide, and bleomycin: a trial of the Gynecologic Oncology
Group. J Clin Oncol. 12:701–706. 1994.
|
|
7
|
Willemse PH, Aalders JG, Bouma J, et al:
Long-term survival after vinblastine, bleomycin, and cisplatin
treatment in patients with germ cell tumors in the ovary: an
update. Gynecol Oncol. 28:268–277. 1987.
|
|
8
|
Nawa A, Obata N, Kikkawa F, et al:
Prognostic factors of patients with yolk sac tumors of the ovary.
Am J Obstet Gynecol. 184:1182–1188. 2001.
|
|
9
|
Wada S, Yoshimura R, Nishisaka N, et al:
Primary retroperitoneal pure yolk-sac tumor in an adult male. Scand
J Urol Nephrol. 35:515–517. 2001.
|
|
10
|
DiPerna CA, Bowdish ME, Weaver FA, et al:
Concomitant vascular procedures for malignancies with vascular
invasion. Arch Surg. 137:901–906. 2002.
|
|
11
|
Peccatori F, Bonazzi C, Chiari S, et al:
Surgical management of malignant ovarian germ cell tumors: 10
years’ experience of 129 patients. Obstet Gynecol. 86:367–372.
1995.
|
|
12
|
Ayhan A, Bildirici I, Günalp S and Yuce K:
Pure dygerminoma of the ovary: a review of 45 well staged cases.
Eur J Gynecol Oncol. 21:98–101. 2000.
|
|
13
|
Zanagnolo V, Sartori E, Galleri G,
Pasinetti B and Bianchi U: Clinical review of 55 cases of malignant
ovarian germ cell tumors. Eur J Gynaecol Oncol. 25:315–320.
2004.
|
|
14
|
Talerman A, Haije WG and Baggerman L:
Serum alphafetoprotein (AFP) in patients with germ cell tumors of
the gonads and extragonadal sites: correlation between endodermal
sinus (yolk sac) tumor and raised serum AFP. Cancer. 46:380–385.
1980.
|
|
15
|
No authors listed. International Germ Cell
Consensus Classification: a prognostic factor-based staging system
for metastatic germ cell cancers. International Germ Cell Cancer
Collaborative Group. J Clin Oncol. 15:594–603. 1997.
|
|
16
|
Lertkhachonsuk R, Termrungruanglert W,
Vasuratna A, et al: Malignant ovarian germ cell tumor in King
Chulalongkorn Memorial Hospital. J Med Assoc Thai. 88:124–128.
2005.
|
|
17
|
Park S, Lee S, Lee J, et al: Salvage
chemotherapy with paclitaxel, ifosfamide, and cisplatin (TIP) in
relapsed or cisplatin-refractory germ cell tumors. Onkologie.
34:416–420. 2011.
|
|
18
|
Zanetta G, Bonazzi C, Cantù M, et al:
Survival and reproductive function after treatment of malignant
germ cell ovarian tumors. J C1in Oncol. 19:1015–1020. 2001.
|
|
19
|
Mayordomo JI, Paz-Ares L, Rivera F, et al:
Ovarian and extragonadal malignant germ-cell tumors in females: a
single-institution experience with 43 patients. Ann Oncol.
5:225–231. 1994.
|
|
20
|
de La Motte Rouge T, Pautier P, Rey A, et
al: Prognostic factors in women treated for ovarian yolk sac
tumour: a retrospective analysis of 84 cases. Eur J Cancer.
47:175–182. 2011.
|
|
21
|
Kawai M, Kano T, Furuhashi Y, et al:
Prognostic factors in yolk sac tumors of the ovary. A
clinicopathologic analysis of 29 cases. Cancer. 67:184–192.
1991.
|
|
22
|
Tong X, You Q, Li L, et al: Prognostic
factors of patients with ovarian yolk sac tumors: a study in
Chinese patients. Onkologie. 31:679–684. 2008.
|