Introduction
Non-small cell lung carcinoma (NSCLC) is one of the
leading causes of cancer-related mortality worldwide, despite
considerable progress in surgery, chemotherapy, radiotherapy and
biological targeted therapy (1).
Recent research in the last decade has shown that these therapies
predominantly improve a patient’s quality of life; the overall
five-year survival rate for patients with such tumors is <15%
(2). As a consequence, research
into novel prognostic biomarkers and therapeutic target structures
in NSCLC remains a focus of attention.
Phosphatidylinositol 3-kinase (PI3K)/protein kinase
B (Akt) (of the PI3K/Akt signaling pathway) have been shown to be
involved in the regulation of cell proliferation and apoptosis, and
are key to the initiation and progression of malignancies,
enhancing cell survival by the stimulation of cell proliferation
and the inhibition of apoptosis (3,4). More
recent studies have identified the activation of the PI3K/Akt
signaling pathway in several types of human cancer, including brain
glioma (5), breast cancer (6) and pancreatic cancer (7). In addition, the high expression of
PI3K and phosphorylated (p)-Akt are often associated with a poor
prognosis. PI3K and p-Akt expression have also been detected in the
early stage of NSCLC (8–13), however, their clinical significance
in operative NSCLC remains controversial (8,9,13).
One study has reported that the antigen expression
of PI3K and p-Akt may be associated with the tumor-node-metastasis
(TNM) stage of NSCLC (8). However,
to the best of our knowledge, there have been no studies on PI3K
and p-Akt expression in advanced NSCLC and the association with
prognosis. In the present retrospective study, the correlations
between the antigen expression of PI3K and p-Akt, and the
clinicopathological data of NSCLC patients and the prognosis in
advanced NSCLC were evaluated.
Patients and methods
Patients
The clinical records of 157 patients (110 males and
47 females; mean age, 57.3 years; range, 46–72 years) with NSCLC
(70 stage I–IIIA and 87 stage IIIB–IV cases), who were admitted to
the Taizhou People’s Hospital (Taizhou, Jiangsu, China) between
June 2008 and June 2010 were retrospectively evaluated. In total,
75 cases of squamous cell carcinoma (SCC), 82 cases of
adenocarcinoma (AdC) and 30 resected lung cancer tumor-adjacent
tissue samples were obtained. Stage I–IIIA patients were confirmed
based on the histopathology report following surgery, while stage
IIIB–IV patients were confirmed using computed tomography-guided
percutaneous or bronchoscopic lung biopsies. The patients were
divided into stages I, II, IIIA, IIIB and IV tumor groups,
according to the TNM system (14).
Patients with advanced NSCLC were excluded from the study if they
had received prior chemotherapy or radiotherapy, or if they had no
definitive histological diagnosis, a poor performance status (PS)
[Eastern Cooperative Oncology Group (ECOG)-PS of ≥3), brain tumor
metastasis or a disease other than lung cancer that may have
affected survival, including cardiac dysfunction, renal
insufficiency, liver cirrhosis or concomitant malignancy. This
study was approved by the Ethics Committee of Taizhou People’s
Hospital and was performed according to the Declaration of
Helsinki. Written informed consent was obtained from the family of
each patient.
Immunohistochemistry
Paraffin-embedded tissue blocks were cut into 4-μm
sections, and representative sections were analyzed
immunohistochemically (EliVision™ Plus IHC kit; Wuhan Boster
Biological Engineering Co., Ltd. Wuhan, China) for PI3K and p-Akt
(1:200; mouse polyclonal antibody; Miltenyi Biotec, San Diego, CA,
USA). Briefly, the sections were dewaxed in xylene and rehydrated
in ethanol through graded concentrations of alcohol. Endogenous
peroxidase activity was blocked by incubating the sections in 5%
hydrogen peroxide in absolute methanol at room temperature for 10
min. Antigen retrieval was performed in a microwave oven for two
cycles of 10 min each. Primary antibodies were applied for 1 h at
room temperature and the sections were washed three times with 0.05
M Tris-buffered saline [TBS (pH 7.2)]. Next, 50 μl immunoglobulin
G/horseradish peroxidase secondary antibody (Wuhan Boster
Biological Engineering Co., Ltd.) was added, followed by incubation
for 30 min at room temperature. The sections were washed three
times with TBS and the reaction products were visualized with
diaminobenzidine (DAB kit; Wuhan Boster Biological Engineering Co.,
Ltd.). The sections were counterstained with hematoxylin and eosin
(Wuhan Boster Biological Engineering Co., Ltd.), dehydrated and
evaluated under a light microscope (DM3000, Leica, Mannheim,
Germany).
Immunohistochemistry scoring
Positive staining for PI3K and p-Akt was assessed in
10 high-power fields of each tumor by two independent pathologists
using light microscopy in a blinded manner. The mean rate of
positive tumor cells was calculated. PI3K and p-Akt expression was
evaluated for each tissue sample by calculating a total
immunostaining score as the product of the proportion and intensity
scores. The proportion score described the estimated fraction of
positively-stained tumor cells (0, none; 1, ≤10%; 2, 10–50%; 3,
51–80%; and 4, ≥80%), while the intensity score represented the
estimated staining intensity (0, no staining; 1, weak; 2, moderate;
and 3, strong). Thus, the total score ranged between 0 and 12. The
positive and negative expression values of PI3K and p-Akt were
defined as scores of >4 and ≤4, respectively.
Follow-up
The stage IIIB–IV NSCLC patients were followed up
from the date of pathological diagnosis until mortality or the last
follow-up to the outpatient department. At the time of the last
follow-up, 80 patients (92%) had succumbed to the disease, and
seven patients (8%) were lost to follow-up or had succumbed to
other causes.
Statistical analysis
The statistical analysis was performed using the
SPSS 13.0 software (SPSS, Inc., Chicago, IL, USA). Correlations
between PI3K and p-Akt immunostaining and the clinicopathological
parameters, including gender, age, pathological type, histologic
grade, lymph node metastasis, TNM stage and ECOG-PS, were analyzed
using χ2 and Fisher’s exact tests. The overall survival
(OS) of the stage IIIB–IV NSCLC patients was calculated from the
date of diagnosis to the date of the last follow-up or mortality.
The cases lost to follow-up or mortality due to any other causes
were defined as censored data for the analysis of the survival
rates. The survival curves were plotted using the Kaplan-Meier
method, and P-values were calculated using the log-rank test. A
multivariate analysis was performed using Cox-proportional hazards
model to identify independent prognostic factors. P≤0.05 was
considered to indicate a statistically significant difference.
Results
PI3K and p-Akt expression in stage I–IIIA
NSCLC and tumor-adjacent tissues
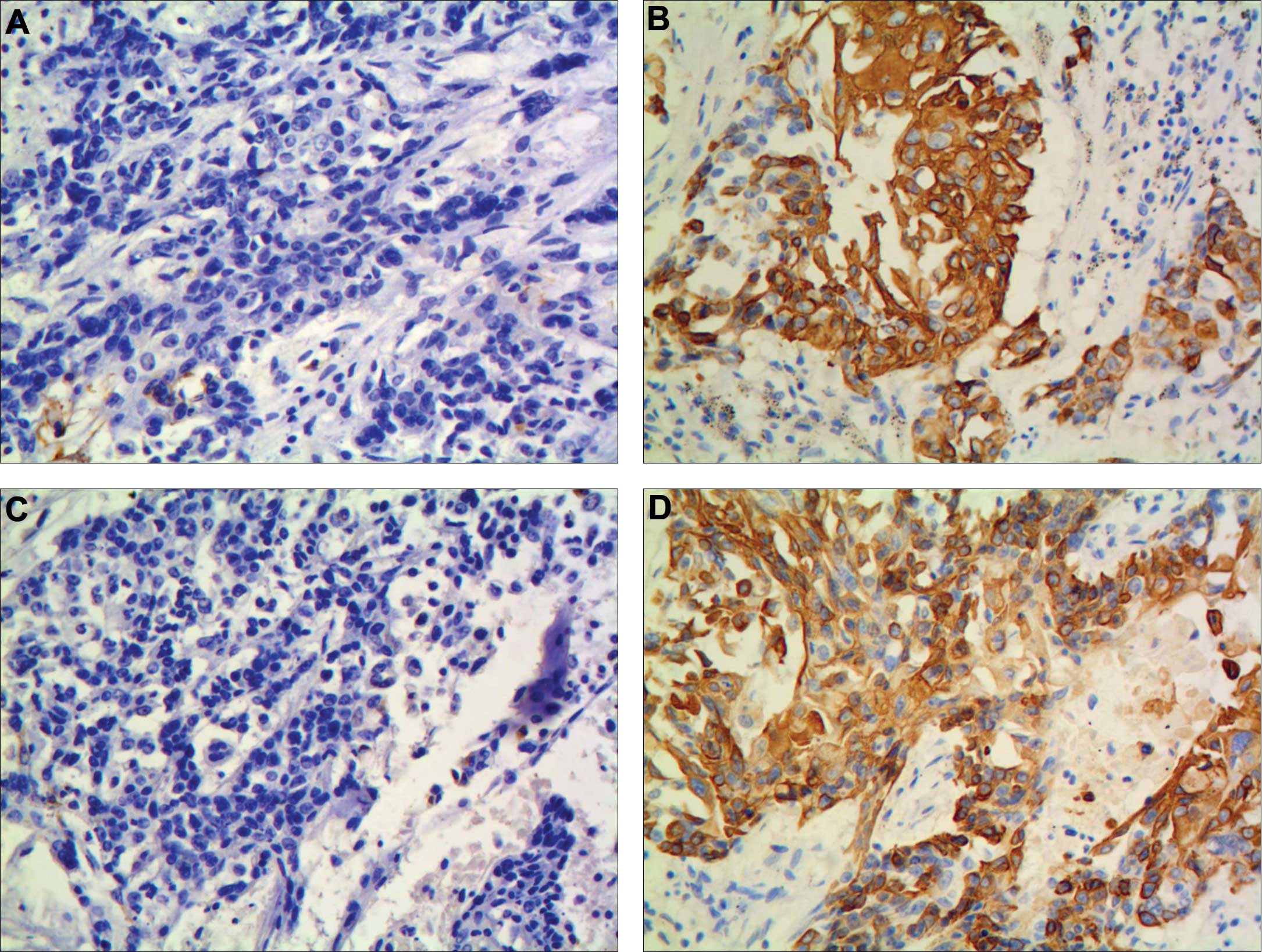
Staining for PI3K and p-Akt demonstrated diffuse
brown particles of varying thickness patterns localized
predominantly in the membrane and cytoplasm of the cancer cells,
however, staining was also occasionally identified in the nucleus.
PI3K and p-Akt expression was absent or infrequent in the
tumor-adjacent tissues. Furthermore, PI3K and p-Akt overexpression
was detected in 58.6 (41/70) and 50.0% (35/70) of the tumors, which
was higher than in the tumor-adjacent tissues for PI3K [16.7%
(5/30); χ2=14.8455; P<0.001] and p-Akt [10.0% (3/30);
χ2=14.2615; P=0.001] (Fig.
1).
PI3K and p-Akt expression in stage
IIIB–IV NSCLC tissues
No significant difference was observed between the
staining location of PI3K and p-Akt in the stage IIIB–IV and I–IIIA
NSCLC tissues. In the stage IIIB–IV tissues, the positive
expression rate of PI3K and p-Akt was 58.6 (51/87) and 45.9%
(40/87), respectively, which did not differ significantly with
regard to the expression in the stage I–IIIA NSCLC tissues
(Figs. 2 and 3).
Correlation between PI3K and p-Akt
expression and the clinicopathological variables
No significant difference was identified in p-Akt
overexpression in stage I–IIIA NSCLC patients with regard to
patient gender, age, pathological type or degree of
differentiation. However, p-Akt overexpression in stage I–IIIA
NSCLC was found to significantly correlate with lymph node
metastasis (χ2=6.1189; P=0.013) and TNM stage
(χ2=8.9752; P=0.011). Furthermore, no significant
difference was identified in p-Akt overexpression in stage IIIB–IV
NSCLC with regard to patient gender, age, pathological type, degree
of differentiation or ECOG-PS. However, p-Akt overexpression in
stage IIIB–IV NSCLC was found to significantly correlate with TNM
stage (χ2=5.7501; P=0.016). The overexpression of PI3K
was not correlated with the aforementioned clinicopathological
variables in all patients (Tables I
and II).
 | Table ICorrelation between PI3K and p-Akt
expression and clinicopathological factors in stage I–IIIA
NSCLC. |
Table I
Correlation between PI3K and p-Akt
expression and clinicopathological factors in stage I–IIIA
NSCLC.
| Characteristics | n | PI3K
overexpression | Positive rate, % | χ2 | P-value | p-Akt
overexpression | Positive rate, % | χ2 | P-value |
|---|
|
|
|---|
| No, n | Yes, n | No, n | Yes, n |
|---|
| Gender |
| Male | 49 | 18 | 31 | 63.3 | 1.4830 | 0.223 | 27 | 22 | 44.9 | 1.7007 | 0.192 |
| Female | 21 | 11 | 10 | 47.6 | | | 8 | 13 | 61.9 | | |
| Age, years |
| ≥60 | 50 | 22 | 28 | 56.0 | 0.4769 | 0.490 | 23 | 27 | 54.0 | 1.1200 | 0.290 |
| <60 | 20 | 7 | 13 | 65.0 | | | 12 | 8 | 40.0 | | |
| Degree of
differentiation |
| Low-middle | 37 | 14 | 23 | 62.2 | 0.4170 | 0.518 | 18 | 19 | 51.4 | 0.0573 | 0.811 |
| High | 33 | 15 | 18 | 54.5 | | | 17 | 16 | 48.5 | | |
| Pathological
type |
| SCC | 38 | 15 | 23 | 60.5 | 0.1309 | 0.717 | 17 | 21 | 55.3 | 0.9211 | 0.337 |
| AdC | 32 | 14 | 18 | 56.3 | | | 18 | 14 | 43.8 | | |
| TNM stage |
| I | 12 | 6 | 6 | 50.0 | 0.8814 | 0.667 | 9 | 3 | 25.0 | 8.9752 | 0.011 |
| II | 35 | 15 | 20 | 57.1 | | | 20 | 15 | 42.9 | | |
| IIIA | 23 | 8 | 15 | 65.2 | | | 6 | 17 | 73.9 | | |
| Lymph node
metastasis |
| Yes | 26 | 9 | 17 | 65.4 | 0.7913 | 0.374 | 8 | 18 | 69.2 | 6.1189 | 0.013 |
| No | 44 | 20 | 24 | 54.6 | | | 27 | 17 | 38.6 | | |
| PS score |
| 0–1 | 52 | 23 | 29 | 55.8 | 0.6544 | 0.419 | 24 | 28 | 53.9 | 1.1966 | 0.274 |
| 2 | 18 | 6 | 12 | 66.7 | | | 11 | 7 | 38.9 | | |
 | Table IICorrelation between PI3K and p-Akt
expression and clinicopathological factors in stage IIIB–IV
NSCLC. |
Table II
Correlation between PI3K and p-Akt
expression and clinicopathological factors in stage IIIB–IV
NSCLC.
|
Characteristicsa | n | PI3K
overexpression | Positive rate,
% | χ2 | P-value | p-Akt
overexpression | Positive rate
% | χ2 | P-value |
|---|
|
|
|---|
| No, n | Yes, n | No, n | Yes, n |
|---|
| Gender |
| Male | 61 | 28 | 33 | 54.1 | 1.7209 | 0.190 | 31 | 30 | 49.2 | 0.8432 | 0.358 |
| Female | 26 | 8 | 18 | 69.2 | | | 16 | 10 | 38.5 | | |
| Age, years |
| ≥60 | 52 | 25 | 27 | 51.9 | 2.3903 | 0.122 | 28 | 24 | 46.2 | 0.0016 | 0.968 |
| <60 | 35 | 11 | 24 | 68.6 | | | 19 | 16 | 45.7 | | |
| Degree of
differentiation |
| Low-middle | 49 | 18 | 31 | 63.3 | 0.9977 | 0.318 | 29 | 20 | 40.8 | 1.2029 | 0.273 |
| High | 38 | 18 | 20 | 52.6 | | | 18 | 20 | 52.6 | | |
| Pathological
type |
| SCC | 37 | 18 | 19 | 51.4 | 1.4025 | 0.236 | 21 | 16 | 43.2 | 0.1937 | 0.660 |
| AdC | 50 | 18 | 32 | 64.0 | | | 26 | 24 | 48.0 | | |
| TNM stage |
| IIIB | 49 | 23 | 26 | 53.1 | 1.4294 | 0.232 | 32 | 17 | 34.7 | 5.7501 | 0.016 |
| IV | 38 | 13 | 25 | 65.8 | | | 15 | 23 | 60.5 | | |
| PS score |
| 0–1 | 41 | 20 | 21 | 51.2 | 1.7511 | 0.186 | 19 | 22 | 53.7 | 1.8421 | 0.175 |
| 2 | 46 | 16 | 30 | 65.2 | | | 28 | 18 | 39.1 | | |
Correlation between PI3K and p-Akt
expression and prognosis in stage IIIB–IV NSCLC
The median OS time of all the patients was 15.33
months (95% CI, 13.81–16.85), and survival time was significantly
improved in the advanced NSCLC patients with PI3K- and
p-Akt-negative expression compared with the patients with positive
expression [P13K: 17.70 months (95% CI, 15.11–20.28 months) vs.
13.43 months (95% CI, 11.83–15.02 months); P=0.004; and p-Akt:
17.13 months (95% CI, 14.93–19.34 months) vs. 13.07 months (95% CI,
11.32–14.82 months); P=0.007]. Multivariate analysis showed that
PI3K (HR=2.143; 95% CI, 1.211–3.790; P=0.009), p-Akt (HR=1.991; 95%
CI, 1.009–3.927; P=0.047), TNM stage (HR=4.788; 95% CI,
2.591–8.848; P=0.001) and ECOG-PS (HR=3.272; 95% CI, 1.701–6.296;
P=0.001) were independent predictors for survival in stage IIIB–IV
NSCLC patients (Figs. 4 and
5; Table III).
 | Table IIIMultivariate analysis of survival in
stage IIIB–IV NSCLC. |
Table III
Multivariate analysis of survival in
stage IIIB–IV NSCLC.
| Parametera | Regression
co-efficient | Standard error | Wald | HR (95% CI) | P-value |
|---|
| PI3K
overexpression | 0.762 | 0.291 | 6.860 | 2.143
(1.211–3.790) | 0.009 |
| p-Akt
overexpression | 0.689 | 0.347 | 3.948 | 1.991
(1.009–3.927) | 0.047 |
| Age, years (≥60 vs.
<60) | −0.156 | 0.233 | 0.446 | 0.856
(0.542–1.351) | 0.504 |
| Gender (male vs.
female) | −0.008 | 0.258 | 0.001 | 0.992
(0.598–1.646) | 0.976 |
| TNM stage (IIIb vs.
IV) | 1.566 | 0.313 | 24.982 | 4.788
(2.591–8.848) | 0.001 |
| Degree of
differentiation (low-middle vs. high) | −0.013 | 0.241 | 0.003 | 0.987
(0.616–1.583) | 0.963 |
| PS score (0–1 vs.
2) | 1.186 | 0.334 | 12.609 | 3.272
(1.701–6.296) | 0.001 |
Discussion
The PI3K/Akt signaling pathway is pivotal in the
initiation and progression of malignancies, enhancing cell survival
by stimulating cell proliferation, inhibiting apoptosis, promoting
tumor angiogenesis and enhancing resistance to chemotherapy and
radiotherapy (15,16). Signaling is predominantly activated
by growth factor receptor tyrosine kinases (17), which in turn converts membrane-bound
phosphatidylinositol 4,5-bisphosphonate to phosphatidylinositol
3,4,5-trisphosphate, which subsequently activates Akt by
phosphorylation. p-Akt acts to promote cell proliferation and
survival by antagonizing and inactivating various components of the
apoptotic cascade, including Bcl-2 (18), caspase-9 (19), glycogen synthase kinase 3 (20) and Forkhead transcription factor
family members (21). p-Akt has
also been shown to promote cell proliferation by regulating the
stability of cyclin D1 (22) or
activating mTOR (23). Furthermore,
a previous study revealed that p-Akt is extremely important in the
regulation of angiogenesis and metastasis in various types of human
malignancy (24).
More recent studies have identified the activation
of the PI3K/Akt signaling pathway in several types of human cancer,
including brain glioma (5), breast
cancer (6) and pancreatic cancer
(7). In addition, the high
expression of PI3K and p-Akt are often associated with a poor
prognosis. PI3K and p-Akt expression have also been detected in the
early stage of NSCLC, however, their clinical significance in
operative NSCLC remains controversial. Tsurutani et al
(12) reported that p-Akt was
positive in the majority NSCLC specimens, but rarely detected in
the surrounding normal tissues, indicating that p-Akt activation is
a factor for a poor prognosis for all stages of NSCLC. These
results indicated that the activation of the PI3K/Akt signaling
pathway is important in the transition from precancerous lesion to
malignancy. Balsara et al (25) also reported that the overexpression
of mTOR, a downstream target of the PI3K/Akt signaling pathway, was
significantly higher than the expression in normal lung tissue, and
its expression was found to closely correlate with the TNM stage.
These findings suggested that the activation of the PI3K/Akt
pathway is closely correlated with tumor progression. David et
al (9) investigated the tumors
obtained from 61 patients with NSCLC in three tissue microarrays
and found that the positive expression rate of p-Akt was 23%
(14/61), indicating that p-Akt is an independent adverse prognostic
factor for NSCLC. The expression and clinical significance of p-Akt
in operative NSCLC was also confirmed by Al-Saad et al
(8). Notably, the study also found
that the high expression of PI3K in tumor stromal cells is an
independent factor for a favorable prognosis for NSCLC. Shah et
al (13) examined 82 surgically
resected stage I–IIIA NSCLC samples for p-Akt by
immunohistochemistry and found that high p-Akt levels correlate
with high tumor grade, whereby p-Akt is an independent factor for a
favorable prognosis for stage I–IIIA NSCLC. Al-Saad et al
(8) considered that these
inconsistent results may be the result of tissue specificity,
technical differences, immunohistochemical antibodies obtained from
different providers, varying scoring methods, study size and the
number of statistical variables entered in the multivariate
analysis (8).
In the present study, the clinical records of 70
patients with stage I–IIIA NSCLC were retrospectively evaluated,
and it was detected that PI3K and p-Akt expression occurred in the
membrane of lung cancer cells, as well as the cytoplasm and
occasionally the nucleus. PI3K and p-Akt overexpression were
detected in 58.6 and 50.0% of the tumors, which was higher than
that observed in the tumor-adjacent tissues. These results revealed
that the PI3K/Akt signaling pathway is overactivated in NSCLC and
may closely correlate with the initiation and progression of the
condition, as observed in previous studies (9,12). The
present study also detected that p-Akt overexpression in stage
I–IIIA NSCLC was significantly correlated with lymph node
metastasis and TNM stage, which revealed that the activation of the
PI3K/Akt signaling pathway may be involved in the promotion of cell
proliferation, invasion and metastasis in NSCLC.
To the best of our knowledge, no studies have been
reported with regard to the correlation between PI3K and p-Akt
expression and advanced NSCLC in the English-language literature.
The present study revealed that PI3K and p-Akt are detected in
advanced NSCLC, however, no significant difference was identified
between the staining location and overexpression of PI3K and p-Akt
in stage IIIB–IV NSCLC tissues compared with that in stage I–IIIA
NSCLC tissues. p-Akt overexpression in advanced NSCLC was found to
significantly correlate with TNM stage, which revealed that the
activation of the PI3K/Akt signaling pathway may be persistently
involved in the progression of NSCLC. Furthermore, the multivariate
analysis showed that p-Akt, TNM stage and ECOG-PS were independent
and adverse prognostic markers in advanced NSCLC, as observed in
the previous studies by David et al (9) and Al-Saad et al (8), but inconsistent with the study by Shah
et al (13). We hypothesize
that the possible reasons for these contradictory results may
include the number of samples and the TNM staging of the selected
patients. The present study also revealed that PI3K is an
independent and unfavorable prognostic marker in advanced NSCLC,
contradictory to the results found in the study by Al-Saad et
al (9), which revealed that the
high expression of PI3K in tumor stromal cells is an independent
favorable prognostic factor in NSCLC. The results of the study by
Al-Saad et al indicate that the stromal overexpression of
PI3K enhances stromal cell function by preventing tumor cell
proliferation in concert with the assumed function of the immune
system.
Due to the limited follow-up time in stage I–IIIA
NSCLC, the correlation between PI3K and p-Akt expression and
prognosis in stage I–IIIA NSCLC was not analyzed in the present
study. With an extension to the follow-up time, this study will be
continued in the next phase of research.
In conclusion, the PI3K/Akt signaling pathway is
overactivated in NSCLC, and is closely correlated with unfavorable
prognostic factors. PI3K and p-Akt are also independent and adverse
prognostic markers in advanced NSCLC. The results of the present
study further indicate that PI3K and p-Akt may be potential
therapeutic targets for NSCLC. However, due to the limitations
inherent in retrospective analyses, the prognostic value of PI3K
and p-Akt overexpression requires further validation in larger
prospective studies.
References
|
1
|
Molina JR, Yang P, Cassivi SD, Schild SE
and Adjei AA: Non-small cell lung cancer: epidemiology, risk
factors, treatment, and survivorship. Mayo Clin Proc. 83:584–594.
2008.
|
|
2
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011.
|
|
3
|
Cantrell DA: Phosphoinositide 3-kinase
signaling pathways. J Cell Sci. 114:1439–1445. 2001.
|
|
4
|
Hennessy BT, Smith DL, Ram PT, Lu Y and
Mills GB: Exploiting the PI3K/AKT pathway for cancer drug
discovery. Nat Rev Drug Discov. 4:988–1004. 2005.
|
|
5
|
Sunayama J, Sato A, Matsuda K, et al: Dual
blocking of mTor and PI3K elicits a prodifferentiation effect on
glioblastoma stem-like cells. Neuro Oncol. 12:1205–1219. 2010.
|
|
6
|
Zhou J, Wulfkuhle J, Zhang H, et al:
Activation of the PTEN/mTOR/STAT3 pathway in breast cancer
stem-like cells is required for viability and maintenance. Proc
Natl Acad Sci USA. 104:16158–16163. 2007.
|
|
7
|
Missiaglia E, Dalai I, Barbi S, et al:
Pancreatic endocrine tumors: expression profiling evidences a role
for AKT-mTOR pathway. J Clin Oncol. 28:245–255. 2010.
|
|
8
|
Al-Saad S, Donnem T, Al-Shibli K, Persson
M, Bremnes RM and Busund LT: Diverse prognostic roles of AKT
isoforms, PTEN and PI3K in tumor epithelial cells and stromal
compartment in non-small cell lung cancer. Anticancer Res.
29:4175–4183. 2009.
|
|
9
|
David O, Jett J, LeBeau H, et al:
Phospho-Akt over expression in non-small cell lung cancer confers
significant stage-independent survival disadvantage. Clin Cancer
Res. 10:6865–6871. 2004.
|
|
10
|
Tang JM, He QY, Guo RX and Chang XJ:
Phosphorylated Akt over expression and loss of PTEN expression in
non-small cell lung cancer confers poor prognosis. Lung Cancer.
51:181–191. 2006.
|
|
11
|
Tsao AS, McDonnell T, Lam S, et al:
Increased phospho-AKT (Ser (473)) expression in bronchial
dysplasia: implications for lung cancer prevention studies. Cancer
Epidemiol Biomarkers Prev. 12:660–664. 2003.
|
|
12
|
Tsurutani J, Fukuoka J, Tsurutani H, et
al: Evaluation of two phosphorylation sites improves the prognostic
significance of Akt activation in non-small cell lung cancer
tumors. J Clin Oncol. 24:306–314. 2006.
|
|
13
|
Shah A, Swain WA, Richardson D, et al:
Phospho-Akt expression is associated with a favorable outcome in
non-small cell lung cancer. Clin Cancer Res. 11:2930–2936.
2005.
|
|
14
|
Groome PA, Bolejack V, Crowley JJ, et al:
IASLC International Staging Committee; Cancer Research and
Biostatistics; Observers to the Committee; Participating
Institutions: The IASLC Lung Cancer Staging Project: validation of
the proposals for revision of the T, N, and M descriptors and
consequent stage groupings in the forthcoming (seventh) edition of
the TNM classification of malignant tumors. J Thorac Oncol.
2:694–705. 2007.
|
|
15
|
Shaw RJ and Cantley LC: Ras, PI(3)K and
mTOR signalling controls tumor cell growth. Nature. 441:424–430.
2006.
|
|
16
|
Pisick E, Jagadeesh S and Salgia R:
Receptor tyrosine kinases and inhibitors in lung cancer.
ScientificWorldJournal. 4:589–604. 2004.
|
|
17
|
Brunet A, Bonni A, Zigmond MJ, et al: Akt
promotes cell survival by phosphorylating and inhibiting a Forkhead
transcription factor. Cell. 96:857–868. 1999.
|
|
18
|
Henshall DC, Araki T, Schindler CK, et al:
Activation of bcl-2 associated death protein and counter-response
of Akt within cell populations during seizure-induced neuronal
death. J Neurosci. 22:8458–8465. 2002.
|
|
19
|
Duguay D and deBlois D: Differential
regulation of Akt, caspases and MAP kinases underlies smooth muscle
cell apoptosis during aortic remodelling in SHR treated with
amlodipine. Br J Pharmacol. 151:1315–1323. 2007.
|
|
20
|
Diehl JA, Cheng M, Roussel MF and Sherr
CJ: Glycogen synthase kinase-3b regulates cyclin D1 proteolysis and
subcellular localization. Genes Dev. 12:3499–3511. 1998.
|
|
21
|
Sunters A, Madureira PA, Pomeranz KM,
Aubert M, Brosens JJ, Cook SJ, et al: Paclitaxel-induced nuclear
translocation of FOXO3a in breast cancer cells is mediated by c-Jun
NH2-terminal kinase and Akt. Cancer Res. 66:212–220. 2006.
|
|
22
|
Wang L, Cao XX, Chen Q, Zhu TF, Zhu HG and
Zheng L: DIXDC1 targets p21 and cyclin D1 via PI3K pathway
activation to promote colon cancer cell proliferation. Cancer Sci.
100:1801–1808. 2009.
|
|
23
|
Hahn-Windgassen A, Nogueira V, Chen CC,
Skeen JE, Sonenberg N and Hay N: Akt activates mTOR by regulating
cellular ATP and AMPK activity. J Biol Chem. 280:32081–32089.
2005.
|
|
24
|
Zhang R, Xu Y, Ekman N, et al: Etk/Bmx
transactivates vascular endothelial growth factor 2 and recruits
phosphatidylinositol 3-kinase to mediate the tumor necrosis
factor-induced angiogenic pathway. J Biol Chem. 278:51267–51276.
2003.
|
|
25
|
Balsara BR, Pei J, Mitsuuchi Y, et al:
Frequent activation of Akt in non-small cell lung carcinomas and
preneoplastic bronchial lesions. Carcinogenesis. 25:2053–2059.
2004.
|