Introduction
According to previous studies, spindle cell
carcinoma (SpCC) is an unusual form of divergent differentiated
squamous cell carcinoma (SCC), which consists of elongated
(spindle) epithelial cells and resembles a sarcoma (1). SCC, with the spindle cell component,
is an uncommon phenomenon and a rare type of malignant tumor. It is
also termed as a sarcomatoid carcinoma, pseudosarcoma, pleomorphic
carcinoma and sarcomatous carcinoma (2,3). There
are numerous reports describing the clinical and pathological
findings of SpCC in the head and neck (4–7), with
the majority described as being located in the oral cavity, larynx,
tonsils and pharynx. However, SpCC occurs elsewhere in the body,
such as the skin, lungs and breasts, and the symptoms vary
according to the site.
The histogenesis of SpCC has been the subject of
debate for many decades. It is generally accepted that SpCC is a
monoclonal epithelial neoplasm (8–11) and
the spindle cell element is derived from squamous epithelium with
divergent mesenchymal differentiation (5). However, this type of tumor poses a
significant diagnostic challenge to the pathologist due to the
remarkable morphological and immunohistochemical overlap with other
benign and malignant spindle cell tumors (2,12).
Therefore the importance of an accurate diagnosis is emphasized in
view of the different therapeutic approaches that are required.
In the present report, three cases of SpCC of the
larynx or hypopharynx were investigated, with the aim of presenting
further data on the clinicopathology and immunohistochemistry of
this rare type of tumor. Patients provided written informed
consent.
Case report
Case one
A 55-year-old male was admitted to the Department of
Otolaryngology and Head and Neck Surgery, Sir Run Run Shaw
Hospital, Medical College of Zhejiang University (Hangzhou, China)
complaining of a mass on the left side of the neck, which had been
present for six months. The patient reported that the mass had
increased rapidly over the two preceding months. The patient stated
there was no tenderness or paresthesia, however, the mass had been
punctured and pus had been extracted at the Jiangshan Beilin
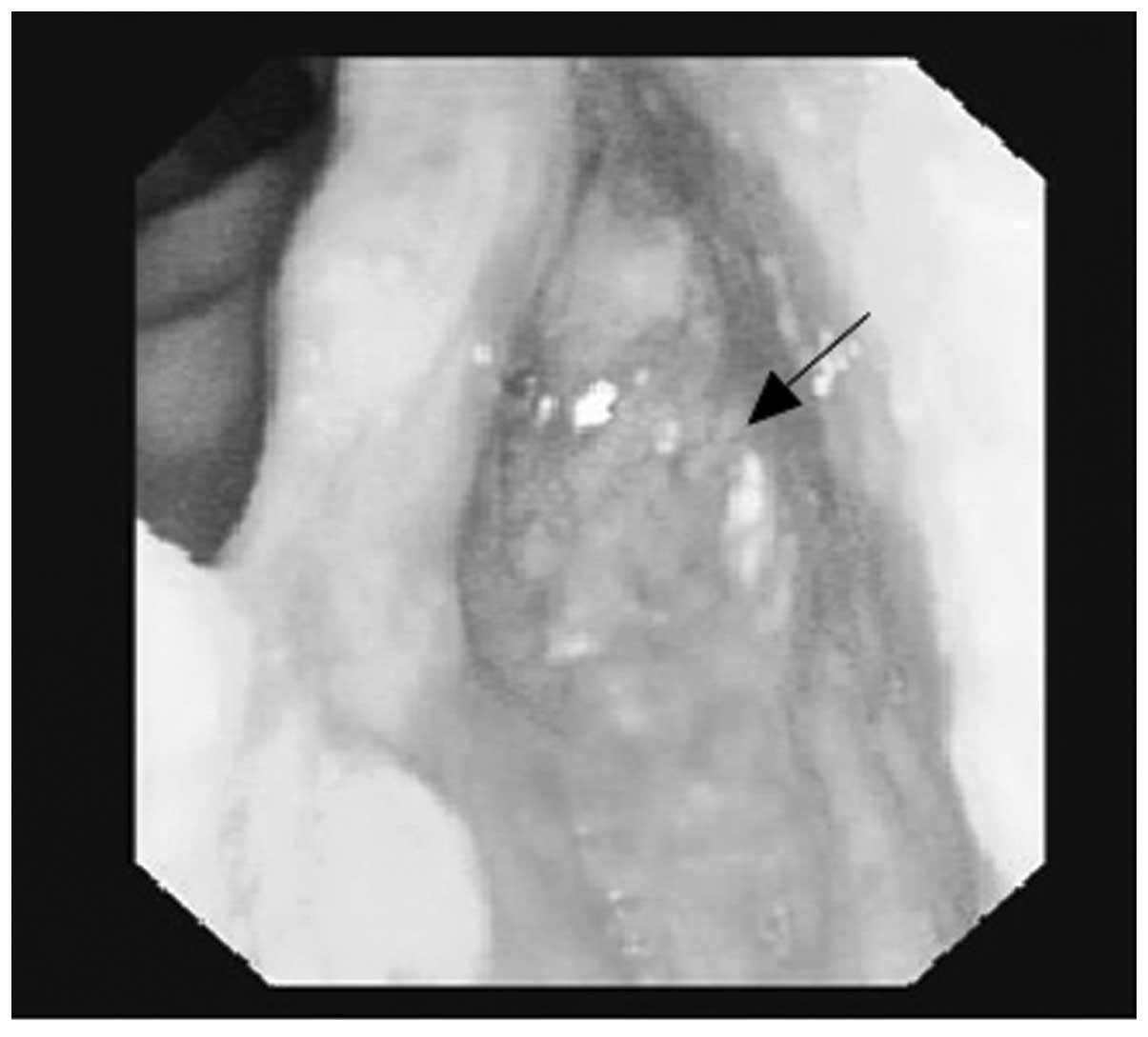
Hospital (Jiangshan, China). An endoscopy revealed a 1.5-cm
submucosal mass in the left pyriform sinus, which extended to the
lateral wall (Fig. 1). The
posterior pharyngeal wall, vocal cords, subglottic region and the
base of the tongue appeared to be healthy. Computed tomographic
(CT) examinations demonstrated a soft tissue mass in the left
pyriform sinus and a 4.4×4.1-cm lesion, which was not well defined
from the surrounding healthy soft tissue on the left side of the
neck (Fig. 2).
The patient underwent surgical removal of the mass
in the left pyriform sinus, without involvement of the larynx,
followed by radial forearm free flap (RFFF) reconstruction of the
hypopharynx under general anesthesia. A neck dissection was
performed to treat the neck lymph node metastasis.
Following surgery, the patient underwent
chemoradiation therapy; this consisted of radiotherapy (6 MV
single-wavelength anomalous diffraction X-ray; absorbed dose to the
tumor was 3,600 cGy; 18 fractions for 26 days) plus concurrent
chemotherapy of 170 mg oxaliplatin for one day and 140 mg
nedaplatin for one day. No acute side-effects were noted, however,
mucositis and odynophagia were observed. Following discharge from
hospital the patient was administered with Chinese traditional
medicine, including Angelica, Astragalus,
Prunella and toad skin. During the follow-up examination 8
months following the patient’s surgery no evidence of recurrence or
metastasis was identified.
Case two
A 62-year-old male was admitted to the Department of
Otolaryngology and Head and Neck Surgery, Sir Run Run Shaw Hospital
(Hangzhou, China), to evaluate the presence of persistent
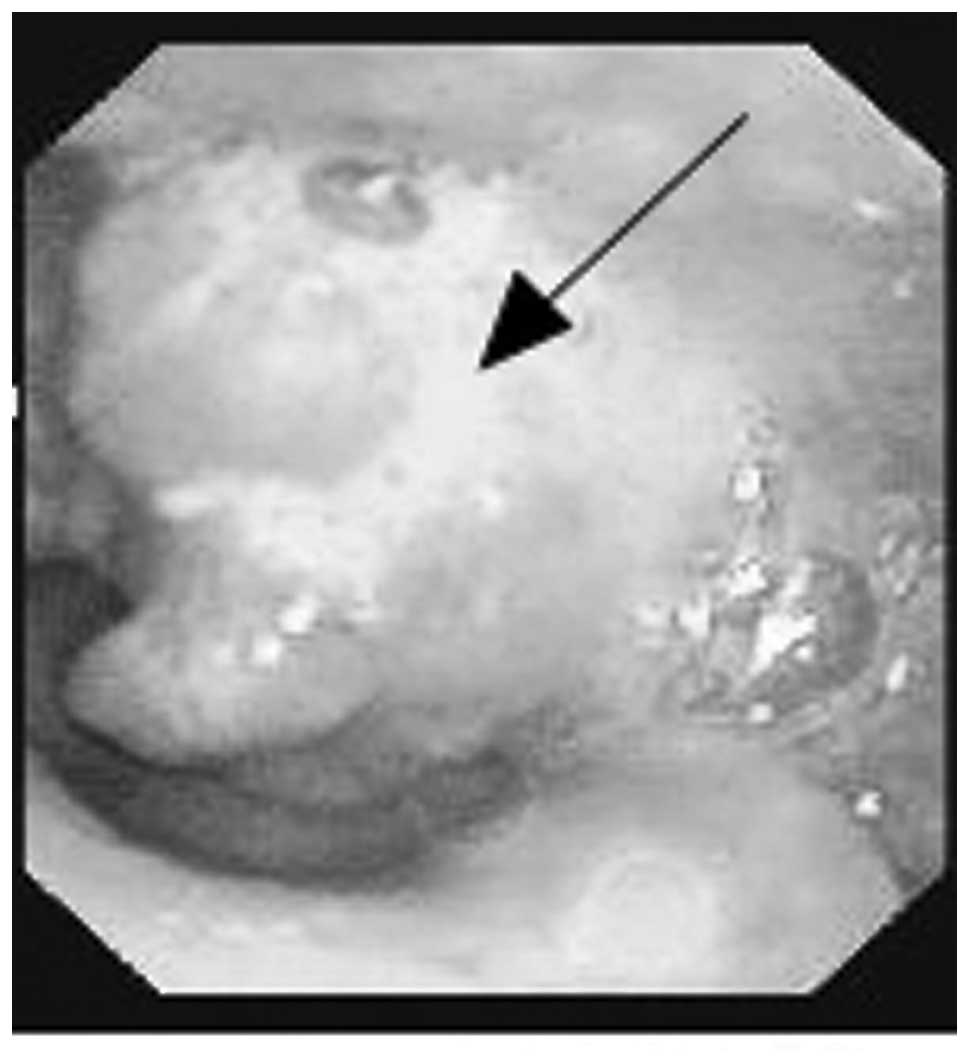
hoarseness (six-month duration). An endoscopy demonstrated a mass
on the left vocal cord, which markedly extended to the anterior
commissure (Fig. 3). CT showed a
1.5×1.0-cm mass on the left vocal cord, at high resolution
(Fig. 4). A total laryngectomy with
neck dissection was performed. The surgically-removed tumor of the
left vocal cord appeared cauliflower-like and was 1.5×1.3 cm in
size. Follow-up of the patient 6 months postoperatively revealed
pulmonary metastases.
Case three
A 57-year-old male presented at the Department of
Otolaryngology and Head and Neck Surgery, Sir Run Run Shaw Hospital
(Hangzhou, China) with a one-year history of pharyngeal foreign
body sensation. An endoscopy and CT revealed a large mass on the
posterior wall of the hypopharynx (Figs. 5 and 6). The patient was treated with a near
total hypopharyngectomy followed by RFFF reconstruction. In
addition, external radiotherapy was administered at the Taizhou
Hospital (Taizhou, China). Metastases and recurrence were not
clinically apparent at the 5.5-month follow-up. A summary of all
three cases is presented in Table
I.
 | Table IBrief summary of the three cases. |
Table I
Brief summary of the three cases.
| No. | Gender | Age, years | Symptom | Site of tumor | Size, cm | Neck lymph node
metastasis | Follow-up |
|---|
| 1 | Male | 55 | Neck mass | Left pyriform
sinus | 1.5×1.2 | 1 | No recurrence at 8
months |
| 2 | Male | 62 | Hoarseness | Left vocal cord | 1.5×1.3 | 0 | Pulmonary metastases
at 6 months |
| 3 | Male | 57 | Foreign body
sensation | Posterior wall of the
hypopharynx | 6.5×6.0 | 0 | No recurrence at 5.5
months |
Histopathological and immunohistochemical
findings
The immunohistochemical results of SpCC are
demonstrated in Table II. In case
one, macroscopically, the largest mass of the neck was 6×5.5 cm,
smooth and solid with partly cystic degeneration, while the tumor
of the left pyriform sinus was 1.5×1.2×1.7 cm and exhibited surface
ulcers. The tissue sample from case two was the total larynx, with
a 1.5×1.3-cm cauliflower-like mass obscuring the entire left vocal
cord. In case three, the mass of the posterior wall of the
hypopharynx was also cauliflower-like, ~6.5×6 cm in size and
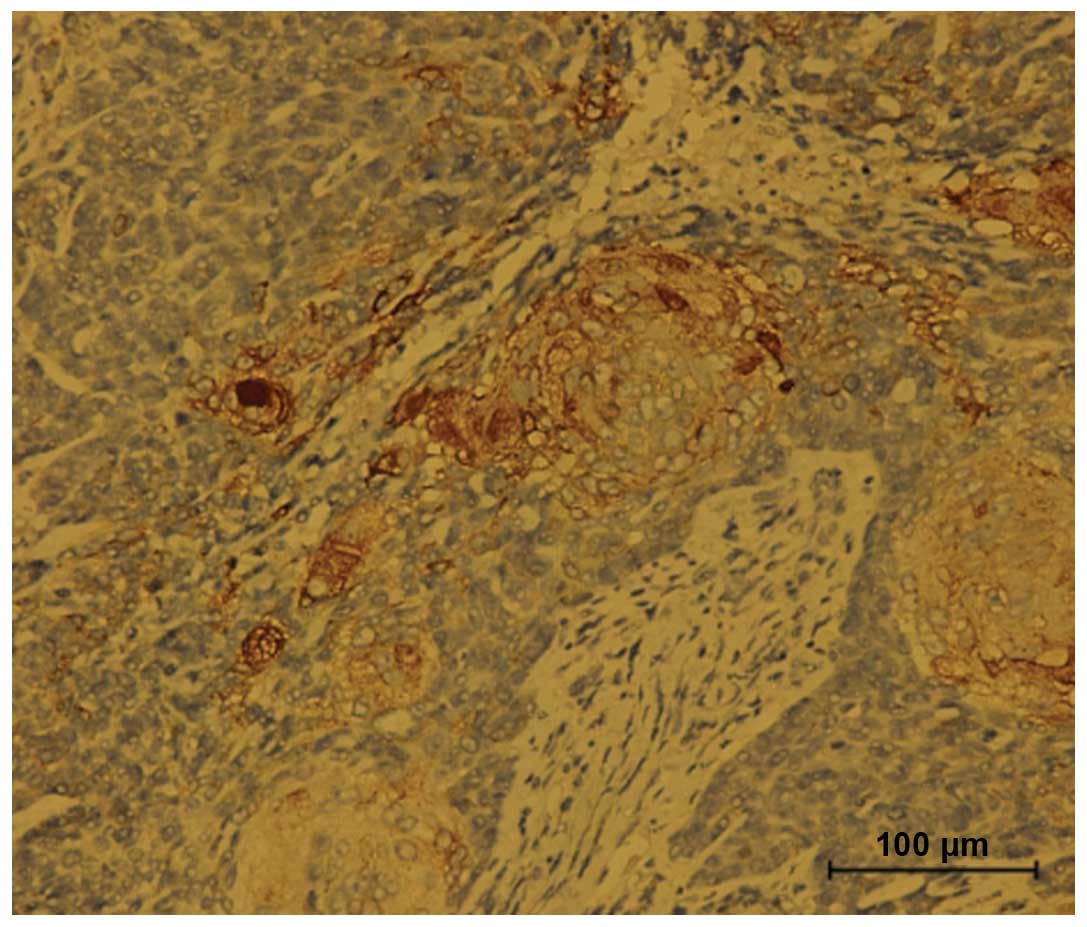
extended to the left pyriform sinus. Histologically, the tumors all
demonstrated a biphasic appearance. The tumors were composed of
bundles of spindle cells with an unusual, basophilic,
hyperchromatic, pleomorphic appearance accompanying small areas of
SCC (Fig. 7). In addition, various
quantities of collagen were identified in the sarcomatoid
zones.
 | Table IIImmunohistochemical results of the
spindle cell carcinoma. |
Table II
Immunohistochemical results of the
spindle cell carcinoma.
| No. | CK (high) | CK (low) | p63 | CK | EMA | Desmin | VM | Ki-67 | CD34 | SMA | Actin | CK7 |
|---|
| 1 | + | − | + | + | − | − | + | + | − | − | − | / |
| 2 | + | / | / | + | − | − | + | + | − | + | + | − |
| 3 | + | + | + | + | + | / | + | − | / | + | / | − |
Immunohistochemistry revealed that the SCC component
was strongly positive for cytokeratin (CK) and the spindle cell
component was strongly positive for vimentin (VM; Fig. 9). Reactivity for epithelial membrane
antigen (Fig. 8), Ki-67, smooth
muscle actin and actin were detected at various levels. No immune
activity was observed for desmin, CD34 or CK7. Additional
immunohistochemical data is demonstrated in Table II. Case one (with lymph node
metastasis) exhibited well-differentiated SCC on the left side of
the neck, however, there was no evidence of metastases in the other
two cases.
Discussion
SpCC is a rare and unusual biphasic malignant
neoplasm of the head and neck. It consists of sarcomatoid
proliferation of pleomorphic spindle shape cells and SCC (13). The mean age of diagnosis of SpCC is
57 years (14). Four factors were
considered that may predispose individuals to this disease: i)
Tobacco use; ii) alcohol use; iii) poor oral health; and iv)
previous irradiation at the site of the tumor (8). The patients included in the present
study were aged 55–62 years and had significant histories of
smoking and alcohol consumption.
SpCC develops due to a variety of reasons, including
genetic predisposition, however, it may also be caused by a
combination of other factors, including injury and inflammation in
patients that are thought to be predisposed to this type of tumor.
It has been hypothesized that the development of the spindle cell
phenotype involves a functional loss of genes, which control
epithelial differentiation, and that the conversion to the spindle
morphology is a recessive entry (15). Lane (16) and Battifora (17) regarded the spindle cells as varying
between mesenchymal metaplasia of epithelial cells to an atypical,
although benign, stromal response. Although there is disagreement
with respect to the origin of these elements, there is a consensus
among various individuals that the size, location and presence of
neck disease, and not the history per se, may guide the
selection of the therapeutic options and influence patient
survival. One study has noted that the malignant squamous cell
component may be inconspicuous, and thus a diligent search for
these elements is required in order to obtain an accurate diagnosis
(18).
Histopathologically, the microscopic features of
SpCC include the presence of two distinct epithelial-derived
components; a squamous cell and a sarcomatoid spindle cell
component. The squamous cell component forms a minor portion of the
tumor mass, whereas the spindle cell component constitutes the
greatest portion and presents a wispy and fasciculated pattern,
which was also demonstrated in the present cases. The squamous
component may be represented by dysplasia, carcinoma in situ
or frankly invasive carcinoma (19). The patient in case one exhibited SCC
in situ.
Histological studies alone cannot explain the
spindle cell components. Recent immunohistochemical studies have
demonstrated the histogenesis of the spindle cells within these
tumors. The concept that spindle cell elements are epithelial in
origin is currently verified by positive keratin immunostaining; in
addition, the demonstration of desmosomes and tonofilaments in the
cells provides further support (7,20). CK
is considered to be the most sensitive and reliable epithelial
marker used for demonstrating the epithelial phenotype. In the
present study, the spindle cells were positive for VM and negative
for CK. The VM positivity indicated that these bundles of cells are
carcinoma cells with true mesenchymal metaplasia. By employing
staining for ras oncogene p21, CK and VM, Toda et al
(21) proposed that the spindle
cell component is epithelial in origin and is malignant. As a
result of the present study, it is hypothesized that SpCC are of
epithelial origin, however, undergo an alteration that results in a
loss of CK.
Review of the literature, diagnostic imaging,
specific staining and electron microscopy facilitates with the
categorization of this type of tumor and therefore, in the design
of individualized surgical approaches. Batsakis (14) advises that these lesions be viewed
as aggressive and that therapy should be based on clinical staging
rather than microscopy. Diagnostic imaging may aid with delineating
the extent of this type of lesion. In the present study, CT was
required to perform the surgical procedures on the patients.
Surgical removal is the preferred method, with radiation providing
an effective adjunctive therapy. Certain authors are of the opinion
that surgery alone is not sufficient and that radiotherapy should
be a mandatory adjunct to surgery. Radiotherapy is also significant
in cases where the surgical margin is positive or where there is
extensive nodal disease. In a previous study, the overall
recurrence rate of SpCC of the head and neck was identified as
71.4% with a metastasis rate of 21.4% (22). These metastasis locations may be
nearby tissues or system-wide locations, which include the lungs,
kidneys and the liver. Incidentally, the lungs were the most
frequent site for metastasis, as reported by Thompson et al
(2) who did not identify soft
tissue as a site for metastasis in their large population of
patients. In those particular cases, the prognosis was poor and
chemotherapy and radiation were the only methods for controlling
the cancer.
In conclusion, SpCC of the larynx and hypopharynx is
potentially aggressive, appears to readily recur and metastasize,
and patients generally have a poor prognosis. Batsakis (14) identified an overall mortality rate
of 35% within 2.5 years across all anatomical sites of the head and
neck that may be associated with this type of tumor. Distant
metastases and the depth of tumor invasion into underlying
structures were found to be reliable prognostic factors, together
with their polypoid configuration. Therefore, long-term and
frequent follow-up is considered to be essential.
Acknowledgements
The authors would like to thank the Department of
Radiation Oncology, Sir Run Run Shaw Hospital, Medical College of
Zhejiang University (Hangzhou, China) for the assistance with
treatment and their contributive discussion. The authors would also
like to thank the Pathology and Radiology Departments for the
technical assistance.
References
|
1
|
Su HH, Chu ST, Hou YY, et al: Spindle cell
carcinoma of the oral cavity and oropharynx: factors affecting
outcome. J Chin Med Assoc. 69:478–483. 2006.
|
|
2
|
Thompson LD, Wieneke JA, Miettinen M and
Heffner DK: Spindle cell (sarcomatoid) carcinomas of the larynx: a
clinicopathologic study of 187 cases. Am J Surg Pathol. 26:153–170.
2002.
|
|
3
|
Batsakis JG: Tumors of the Head and Neck,
Clinical and Pathological Considerations. 2nd edition. Williams
& Wilkins; Baltimore, MA: pp. 217–219. 1979
|
|
4
|
Viswanathan S, Rahman K, Pallavi S, et al:
Sarcomatoid (spindle cell) carcinoma of the head and neck mucosal
region: a clinicopathologic review of 103 cases from a tertiary
referral cancer centre. Head Neck Pathol. 4:265–275. 2010.
|
|
5
|
Batsakis JG and Suarez P: Sarcomatoid
carcinoma of the aerodigestive tracts. Adv Anat Pathol. 7:282–293.
2000.
|
|
6
|
Batsakis JG, Rice DH and Howard DR: The
pathology of head and neck tumors: spindle cell lesions
(sarcomatoid carcinomas, nodular fasciitis, and fibrosarcoma) of
the aerodigestive tracts, Part 14. Head Neck Surg. 4:499–513.
1982.
|
|
7
|
Takata T, Ito H, Ogawa I, et al: Spindle
cell squamous carcinoma of the oral region. An immunohistochemical
and ultrastructural study on the histogenesis and differential
diagnosis with a clinicopathological analysis of six cases.
Virchows Arch A Pathol Anat Histopathol. 419:177–182. 1991.
|
|
8
|
Leventon GS and Evans HL: Sarcomatoid
squamous cell carcinoma of the mucous membranes of the head and
neck: a clinicpathologic study of 20 cases. Cancer. 48:994–1003.
1981.
|
|
9
|
Guarino M, Tricomi P, Giordano F and
Christofori E: Sarcomatoid carcinomas: pathological and
histopathogenetic considerations. Pathology. 28:298–305. 1996.
|
|
10
|
Thompson L, Chang B and Barsky SH:
Monoclonal origins of malignant mixed tumors (carcinosarcomas).
Evidence for a divergent histogenesis. Am J Surg Pathol.
20:277–285. 1996.
|
|
11
|
Torenbeek R, Hermsen MA, Meijer GA, et al:
Analysis by comparative genomic hybridization of epithelial and
spindle cell components in sarcomatoid carcinoma and
carcinosarcoma: histogenetic aspects. J Pathol. 189:338–343.
1999.
|
|
12
|
Anderson CE and Al-Nafussi A: Spindle cell
lesions of the head and neck: an overview and diagnostic approach.
Diagn Histopathol. 15:264–272. 2009.
|
|
13
|
Kudo Y, Ogawa I, Kitagawa M, et al:
Establishment and characterization of a spindle cell squamous
carcinoma cell line. J Oral Pathol Med. 35:479–483. 2006.
|
|
14
|
Batsakis JG: ‘Pseudosarcoma’ of the mucous
membranes in the head and neck. J Laryngol Otol. 95:311–316.
1981.
|
|
15
|
Munakata R, Cheng J, Nakajima T and Saku
T: Spindle cell carcinoma of the gingiva: report of an autopsy
case. J Oral Pathol Med. 27:180–184. 1998.
|
|
16
|
Lane N: Pseudosarcoma (polypoid
sarcoma-like masses) associated with squamous-cell carcinoma of the
mouth, fauces, and larynx. Cancer. 10:19–41. 1957.
|
|
17
|
Battifora H: Spindle cell carcinoma.
Cancer. 37:2275–2282. 1976.
|
|
18
|
Viswanathan S, Rahman K, Pallavi S, et al:
Sarcomatoid (spindle cell) carcinoma of the head and neck mucosal
region: a clinicopathologic review of 103 cases from a tertiary
referral cancer centre. Head Neck Pathol. 4:265–275. 2010.
|
|
19
|
Ansari-Lari MA, Hoque MO, Califano J and
Westra WH: Immunohistochemical p53 expression patterns in
sarcomatoid carcinoma of the upper respiratory tract. Am J Surg
Pathol. 26:1024–1031. 2002.
|
|
20
|
Shibuya Y, Umeda M, Yokoo S and Komori T:
Spindle cell squamous carcinoma of the maxilla: report of a case
with immunohistochemical analysis. J Oral Maxillofac Surg.
58:1164–1169. 2000.
|
|
21
|
Toda S, Yonemitsu N, Miyabara S, et al:
Polypoid squamous cell carcinoma of the larynx. An
immunohistochemical study for ras p21 and cytokeratin. Pathol Res
Pract. 185:860–866. 1989.
|
|
22
|
Sarma A, Das R, Sharma JD and Kataki AC:
Spindle cell carcinoma of the head and neck: A clinicopathological
and immunohistochemical study of 40 Cases. J Cancer Ther.
3:1055–1059. 2012.
|