Introduction
It is hypothesized that neuroendocrine carcinoma
(NEC) arise from cells that are involved in the diffuse endocrine
system (1). The biological activity
and prognosis of NEC are associated with various factors, including
the tumor site, histological type and degree of differentiation. A
number of studies have confirmed that poorly differentiated NEC is
associated with an aggressive clinical course and poor prognosis
(2,3). Numerous patients with NEC develop
hepatic metastasis (4), which must
be distinguished from primary hepatocellular carcinoma (HCC). HCC
is one of the most common types of tumor worldwide and one of the
most malignant. Furthermore, patients with chronic hepatitis B
viral infection or alcoholic cirrhosis are at increased risk of
developing HCC (5). In the present
case, the patient was diagnosed with primary HCC within a few
months of being diagnosed with a tonsil NEC. Such NEC of the tonsil
tend to be aggressive and are associated with a poor prognosis.
This report describes one case of tonsil neuroendocrine carcinoma
concurrent with hepatocellular carcinoma. Patient provided written
informed consent.
Case report
A 72-year-old male was admitted to the Gaozhou
People’s Hospital (Gaozhou, China) in March 2013 with a four-month
history of a left neck tumor. Fine-needle aspiration of the left
tonsil mass had been performed at two other hospitals and was
identified to be positive for a small-cell malignancy or NEC. The
patient was referred to The Affiliated Tumor Hospital of Guangzhou
Medical University (Guangzhou, China) for further treatment. The
patient’s medical history included hypertension, which had been
present for six years with intermittent use of oral
antihypertensive agents. In addition, the patient was infected with
the hepatitis B virus (HBV) and had suffered with liver cirrhosis
for 15 years. The patient was a non-smoker, however, occasionally
consumed alcohol. The physical examination was notable for a
solitary, left, level II tonsil mass (size, 3.6×2.0 cm), according
to the following chinese antiadoncus clinical classification
system: I, Tonsil enlargement which does not exceed the pharyngeal
arch palate; II, tonsil enlargement exceeds the pharyngeal arch
palate, but does not exceed the midline of the posterior pharyngeal
wall; and III, tonsil enlargement exceeds the midline of the
posterior pharyngeal wall (6).
There were numerous enlarged nodes on each side of the neck; the
largest node was 2.2×1.1 cm. The laboratory tests were abnormal;
the α-fetoprotein (AFP) level had increased to 9.2×104
ng/ml (normal range, 0–25 ng/ml), and carbohydrate antigen 19-9
(normal range, 0–37 U/ml), cancer antigen 125 (normal range, 0–35
kU/l) and neuron specific enolase (NSE; normal range, 0–12.5 U/ml)
were all increasing. In addition, the level of HBV-DNA was
1.62×107 IU/ml (normal range, 0–50 IU/ml). However,
alanine aminotransferase (normal range, 10–40 IU/l), aspartate
aminotransferase (normal range, 10–40 IU/l) and bilirubin (normal
range, 3.4–17.1 μmol/l) were all observed to be within the normal
ranges.
Contrast-enhanced magnetic resonance imaging of the
oropharyngeal airway revealed a 3.6-cm mass of the left palate and
there were numerous enlarged nodes on each side of the neck, with
the largest measuring 2.2×1.1 cm. A computed tomography (CT) scan
of the chest and abdomen demonstrated liver cirrhosis, multiple
liver tumors and portal vein thrombosis, as well as metastasis to
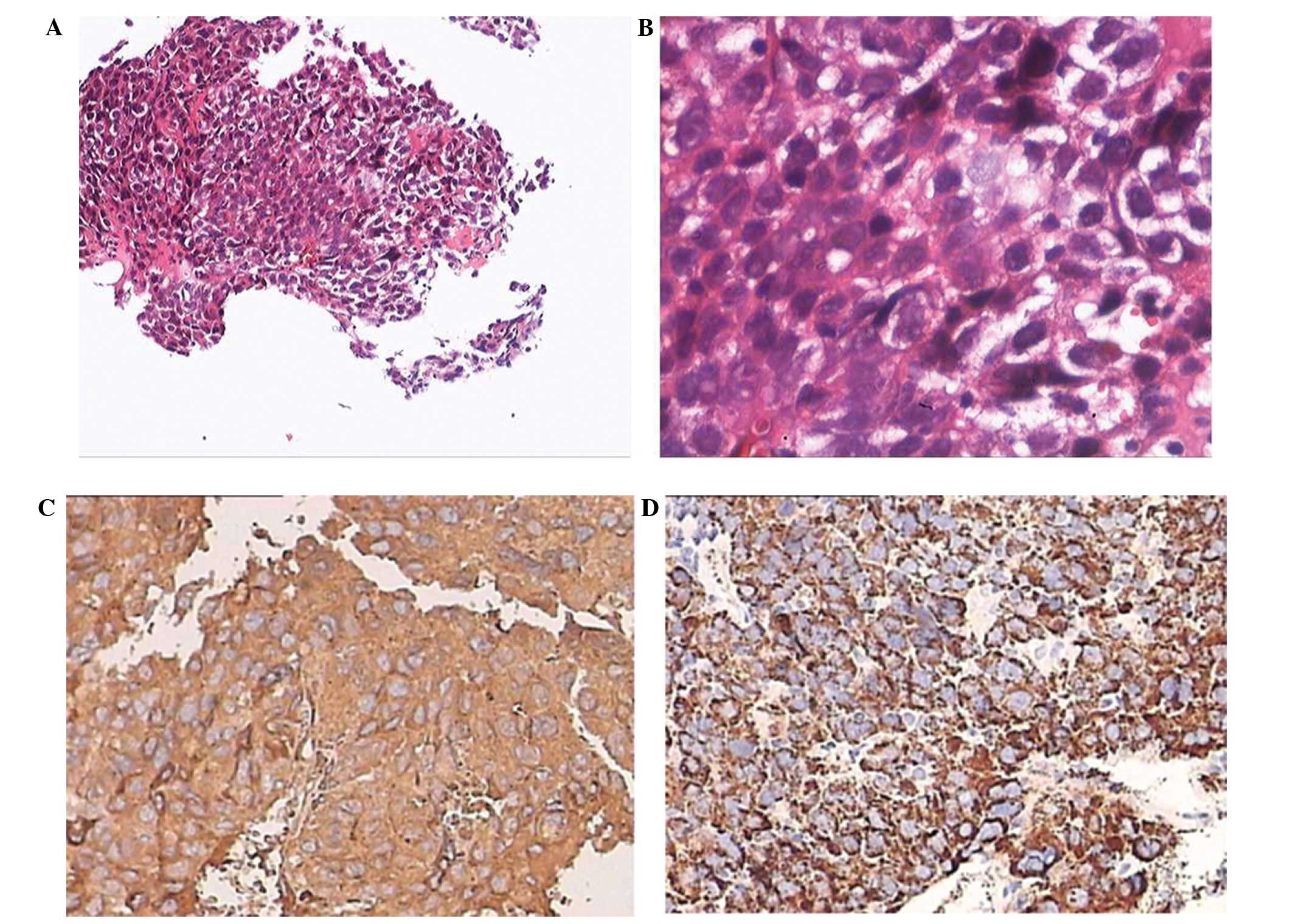
the hilar, abdomen and retroperineum. Histologic examination of the
tonsil revealed an NEC (Fig. 1A and
B). Immunohistochemistry was positive for chromogranin A (CgA),
synaptophysin (Syn), cluster of differentiation (CD)56, AFP, and
some hepatocytes and negative for cytokeratin (CK), p63, melan-A,
CD3, CD10, CD20, CD30, anaplastic lymphoma kinase, CAM5.2,
PAX-5 and CD43. The cell growth index was 80%. Various
tumors located in the right hepatic posterior lobe and right
adrenal gland were identified by color Doppler ultrasound. The
largest liver tumor measured 3.3×3.1 cm and was located in the
right lobe. Histologic examination of the liver revealed a poorly
differentiated primary HCC (Fig. 2A and
B). Immunohistochemistry was positive for Hepatocyte Specific
Antigen antibody (Hep Par-1), AFP, and a small quantity of CK and
was negative for CgA, Syn, CD56 and inhibin. The cell growth index
was 50%. A biopsy of the right adrenal tumor was not performed, as
it was located between the right hepatic lobe and the right kidney
which is unsuitable for biopsy. The size of the oval-shaped tumor
was observed via color Doppler ultrasound to be ~5.3×4.0 cm. The
patient was diagnosed with NEC of the right tonsil with metastatic
disease to the neck, a poorly differentiated HCC, right adrenal
metastatic tumor and level 3 hypertension, and was considered to be
at a particularly high-risk stage. The patient received one cycle
of palliative chemotherapy lasting two days with a cycle duratino
of 21 days with carboplatin (0.5 g) and etoposide (EP; 0.2 g) on
days one to two. The masses continued to grow and the size of the
hepatic tumor increased to 8.0×6.2 cm. Treatment with carboplatin
and EP failed to inhibit the disease progression, and the tonsil
carcinoma became larger and was almost completely blocking the
oropharyngeal airway. Radiotherapy was administered with the aim of
controlling the growth of the tonsil tumor. However, the patient
abandoned the treatment and succumbed due to asphyxia two days
after leaving The Cancer Center of Guangzhou Medical University
(Guangzhou, China).
Discussion
NEC are a heterogeneous family of neoplasms that
possess a broad spectrum of types of histomorphology, tissue
origins and clinical behaviors (7).
NEC generally exhibit slow growth, however, prognosis is dependent
on the tumor site, histological type, degree of differentiation,
mitotic rate, Ki-67 proliferative index, tumor size, depth,
location and the presence of lymph node or liver metastases
(8). The recent WHO classification
(year 2000) defines tumors, on the basis of histopathological and
biological characteristics, into well-differentiated NEC (benign or
uncertain malignancy), well-differentiated NEC (low-grade
malignancy), poorly differentiated NEC (high-grade malignancy) and
mixed tumors (9).
NEC of the head and neck are rare and, therefore,
case reports are only sporadically observed in the literature. A
previous study reported metastatic NEC to the head and neck in
certain primary lung or breast NEC patients (7). In addition, a previous study described
a case of tonsillar metastasis from a primary early-stage large
cell NEC of the lung (10). In the
current patient, the origin of the tumor was hypothesized to be the
tonsil as no tumors were observed in the lung by radiological
examination and there are currently few reports concerning the
metastasis of a tonsil NEC from a primary liver NEC. Furthermore,
the microscopic findings, large size of the tumor and the enlarged
neck lymph nodes supported this hypothesis. Thus, primary NEC
arising from the tonsil was considered to be the most appropriate
diagnosis. To the best of our knowledge, this may be the first
report of a primary tonsil NEC.
The majority of previous reports describe cases of
tumors with a laryngeal origin where the tumors are predominantly
moderately differentiated (11).
However, the pathology slides of the patient in the present study
failed to provide the level of differentiation. In addition, as the
standard therapy for tonsil NEC has not yet been established, the
treatment was conducted with a strategy that is commonly used for
laryngeal NEC. Barker et al (12) investigated 23 adults with
nonsinonasal NEC (NSNEC) of the head and neck, and recommended the
treatment strategy of sequential chemotherapy and radiation. In
this study, there were 19 cases of small-cell undifferentiated
carcinomas and the use of combination chemotherapy approximately
doubled the two-year overall survival and disease-free survival
rates, and reduced the two-year rate of distant metastasis by half.
As NSNEC was found to be highly responsive to cisplatin/EP
combination chemotherapy the induction chemotherapy strategy was
adopted in the present case. However the outcome was not positive
and the efficacy of radiotherapy remains unknown. Further studies
are required to elucidate an optimal treatment strategy for tonsil
NEC.
A total of 50–95% of patients with NEC develop liver
metastases and 80% of patients exhibiting advanced liver disease
succumb within five years of diagnosis (13). Furthermore, certain cases of primary
hepatic NEC have been described in previous studies (14,15).
Therefore, a careful clinical evaluation is essential to
distinguish the extrahepatic origins of tumors; either primary
hepatic NEC or HCC (as in the present case). Kaya et al
(15) reported one case of primary
NEC of the liver in 2001. In this case, the tumor cells were
positively stained for CgA and Syn (the immunological markers for
tumors derived from the neuroendocrine system) and negatively
stained for AFP. In contrast to HCC, hepatic NEC has not previously
been associated with liver cirrhosis. A review of the literature
identified that the immunohistochemical characteristics of HCC
include positivity for the neurosecretory markers, CgA, Syn and
NSE, and negativity for Hep Par-1 (OCH1E5), AFP, thyroid
transcription factor-1, CDX2 and leukocyte common antigen. A
percutaneous biopsy of the liver mass was performed in the present
case and immunohistochemistry revealed a poorly differentiated
HCC.
The incidence of two types of cancer presenting in
one patient is rare; however, ~20% of patients with NEC develop
secondary cancers (8). Combined
primary NEC and HCC of the liver in a 65-year-old male patient was
reported in 2009 by Yang et al (14). It was proposed that the NEC
originated from a poorly differentiated tumor clone of an HCC that
had undergone neuroendocrine differentiation. Ki-67 and p53
expression were identified to be higher in the NEC compared with
that in the HCC. Furthermore, HCC is one of the leading causes of
cancer-associated mortality. HCC progress so rapidly that the
majority of patients are diagnosed with locally advanced or distant
metastasis; therefore, the resulting treatment efficacy and
prognosis is poor. The tumor exhibited a more aggressive clinical
course in accordance with being an NEC, rather than a conventional
HCC, and the patient succumbed due to multiple recurrent tumors and
metastases within a year after surgery. In the present case, the
Ki-67 proliferative index in the tonsil NEC was identified to be
higher than that in the HCC. Considering the aggressive biological
behavior of the NEC, the tonsil NEC was initially treated using
chemotherapy. However, the patient deteriorated and succumbed
within two months of the diagnosis.
In conclusion, NEC of the head and neck is uncommon
and has rarely been described in the tonsil. With regard to NEC,
the prognosis of this type of tumor appears to be poorer when it is
located in the tonsil compared with in other sites of the head and
neck. In addition, it was identified that tonsil NEC is not
sensitive to a chemotherapy regimen that contained carboplatin and
EP. Thus, the optimal treatment for NEC of the tonsil remains
unclear.
References
|
1
|
Clark OH, Benson AB III, Berlin JD, et al:
NCCN Neuroendocrine Tumors Panel Members: NCCN Practice Guidelines
in Oncology: neuroendocrine tumors. J Natl Compr Canc Netw.
7:712–747. 2009.
|
|
2
|
Hochwald SN, Zee S, Conlon KC, et al:
Prognostic factors in pancreatic endocrine neoplasms: an analysis
of 136 cases with a proposal for low-grade and intermediate-grade
groups. J Clin Oncol. 20:2633–2642. 2002.
|
|
3
|
Pape UF, Jann H, Müller-Nordhorn J, et al:
Prognostic relevance of a novel TNM classification system for upper
gastroenteropancreatic neuroendocrine tumors. Cancer. 113:256–265.
2008.
|
|
4
|
Soga J1, Yakuwa Y and Osaka M: Carcinoid
syndrome: a statistical evaluation of 748 reported cases. J Exp
Clin Cancer Res. 18:133–141. 1999.
|
|
5
|
Bruix J and Sherman M; American
Association for the Study of Liver Diseases. Management of
hepatocellular carcinoma: an update. Hepatology. 53:1020–1022.
2011.
|
|
6
|
Chen WB, Pan XL, Kang XX, et al: Head.
Diagnostics. 7th edition. People’s Medical Publishing House;
Beijing: pp. 1012007, (In Chinese).
|
|
7
|
Salama AR, Jham BC, Papadimitriou JC and
Scheper MA: Metastatic neuroendocrine carcinomas to the head and
neck: report of 4 cases and review of the literature. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 108:242–247. 2009.
|
|
8
|
Ian DH and John AHW: Classification of
neuroendocrine tumors. Clinical Endocrine Oncology. (Part 5)2nd
edition. Wiley-Blackwell; Malden, MA: pp. 4422008
|
|
9
|
Solcia E, Klöppel G and Sonbin LH: World
Health Organization international histological classification of
tumours: Histological typing of endocrine tumours. Clin Endocrinol.
53:7–15. 2000.
|
|
10
|
Sugiura Y, Kaseda S, Kakizaki T, et al:
Tonsillar metastais from primary lung large cell neuroendocrine
carcinoma in the early stage; report of a case. Kyobu Geka.
62:1101–1104. 2009.(In Japanese).
|
|
11
|
Mills SE: Neuroectodermal neoplasms of the
head and neck with emphasis on neuroendocrine carcinomas. Mod
Pathol. 15:264–278. 2002.
|
|
12
|
Barker JL Jr, Glisson BS, Garden AS, et
al: Management of nonsinonasal neuroendocrine carcinomas of the
head and neck. Cancer. 98:2322–2328. 2003.
|
|
13
|
Renner G: Small cell carcinoma of the head
and neck: a review. Semin Oncol. 34:3–14. 2007.
|
|
14
|
Yang CS, Wen MC, Jan YJ, et al: Combined
primary neuroendocrine carcinoma and hepatocellular carcinoma of
the liver. J Chin Med Assoc. 72:430–433. 2009.
|
|
15
|
Kaya G, Pasche C, Osterheld MC, et al:
Primary neuroendocrine carcinoma of the liver: an autopsy case.
Pathol Int. 51:874–878. 2001.
|