Introduction
Lipomas of the gastrointestinal tract are benign
tumours and were first reported by Bauer in 1757 (1). Although colonic lipomas are the most
common type of non-epithelial (mesenchymal) neoplasm of the
gastrointestinal tract, they are rare benign tumors (2). Generally, colonic lipomas are
asymptomatic and thus, they are usually detected incidentally
during colonoscopy, surgery or autopsy (3). However, 25% of colonic lipomas are
known to develop symptoms, particularly when their diameter is
>2 cm (4). Symptoms include
anemia, abdominal pain, constipation, diarrhea, bleeding and
intussusception (5). The term
‘giant lipoma’ has been defined as a mass of >5 cm in diameter
(6). Large colonic lipomas are
often misdiagnosed as more serious pathology due to their rarity
and variable presentation (3).
Imaging modality, including computed tomography, contributes to the
preoperative diagnosis of colonic lipomas as its imaging
characteristics are relatively typical for adipose tissue. A firm
diagnosis of colonic lipoma can be established fundamentally based
on the histopathological examination. In 90% of cases, lipomas of
the colon are localized at the submucous level, with only a few
cases presenting in the subserosal layer (7). Although intussusception is a common
disease in children, intussusception caused by colonic lipoma in
adults is a rare condition, and is caused usually by a large
pedunculated lipoma (8). The
current study presents a rare case of a 4-cm sessile lipoma of the
transverse colon causing colonic intussusception.
Case report
In March 2012, a 65-year-old female was admitted to
Wenzhou Central Hospital (Wenzhou, Zhejiang, China) with
intermittent pain in the left abdomen that had been present for two
weeks. The patient had no past history of cancer and no family
history of colorectal cancer. The physical examination was
unremarkable. The laboratory results revealed a white blood cell
count of 12.5×109 cells/l, a neutrophil count of
9.2×109 cells/l (73.2%) and a C-reactive protein level
of 10.4 mg/l. Tumor markers were within the normal ranges.
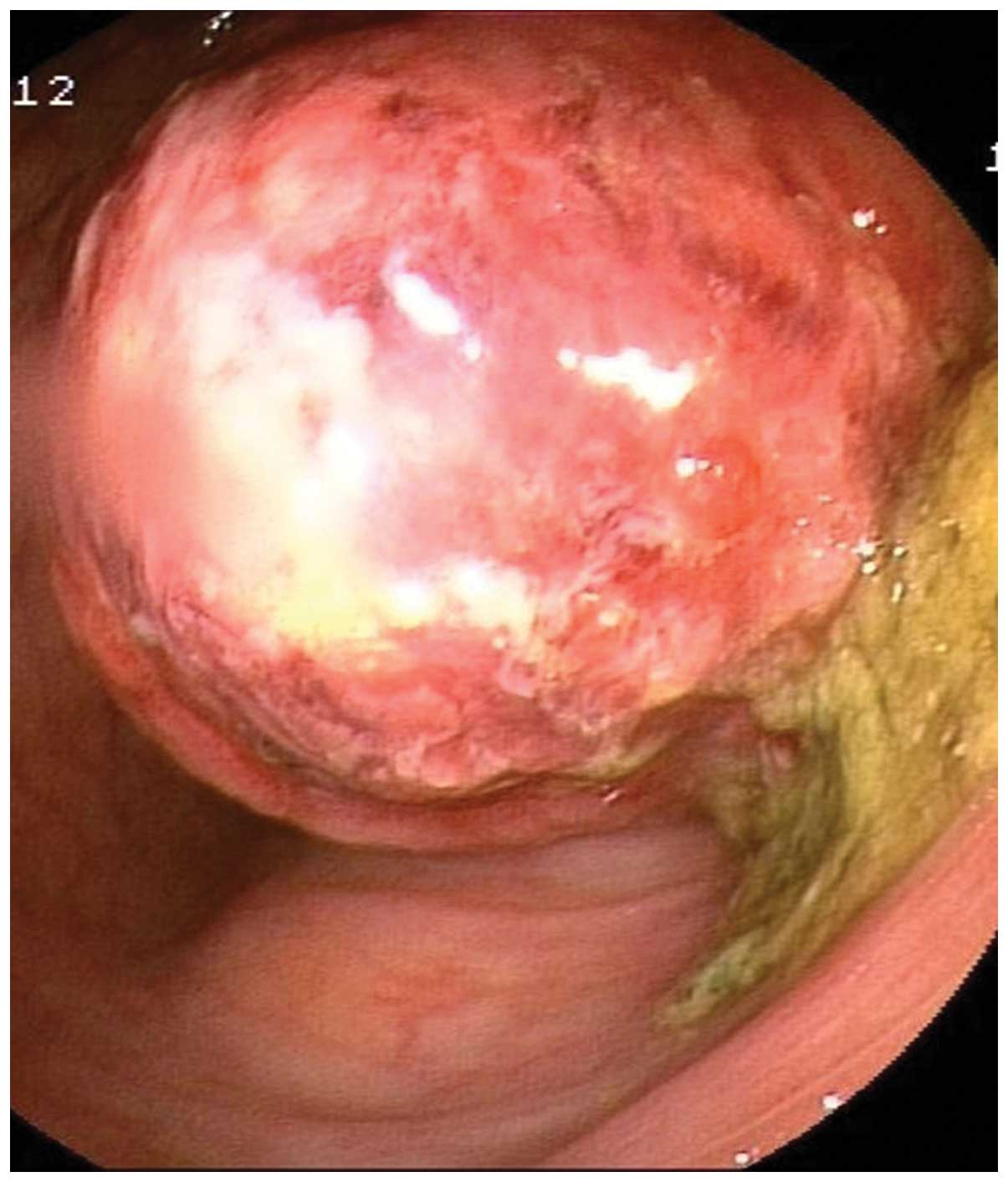
Colonoscopy revealed a 4×5-cm intraluminal spherical mass, 60 cm
above the anal verge, which prevented further progression of the
endoscope. The mass was covered by a 2×3-cm superficial mucosal
erosion, indicating the presence of a malignant gastrointestinal
stromal tumor (Fig. 1). In
addition, a biopsy of the mass revealed numerous ulcerative lesions
with local epithelial regeneration. Furthermore, contrast-enhanced
computed tomography (CT) revealed a well-defined fatty tissue mass
of 4 cm in diameter in the distal transverse colon proximal to the
splenic flexure (Fig. 2A), with
intussusception (Fig. 2B and C) and
local bowel-wall thickening.
The patient underwent segmental resection of the
transverse colon following the initial diagnosis. The
intraoperative frozen section revealed a submucosal lipoma of the
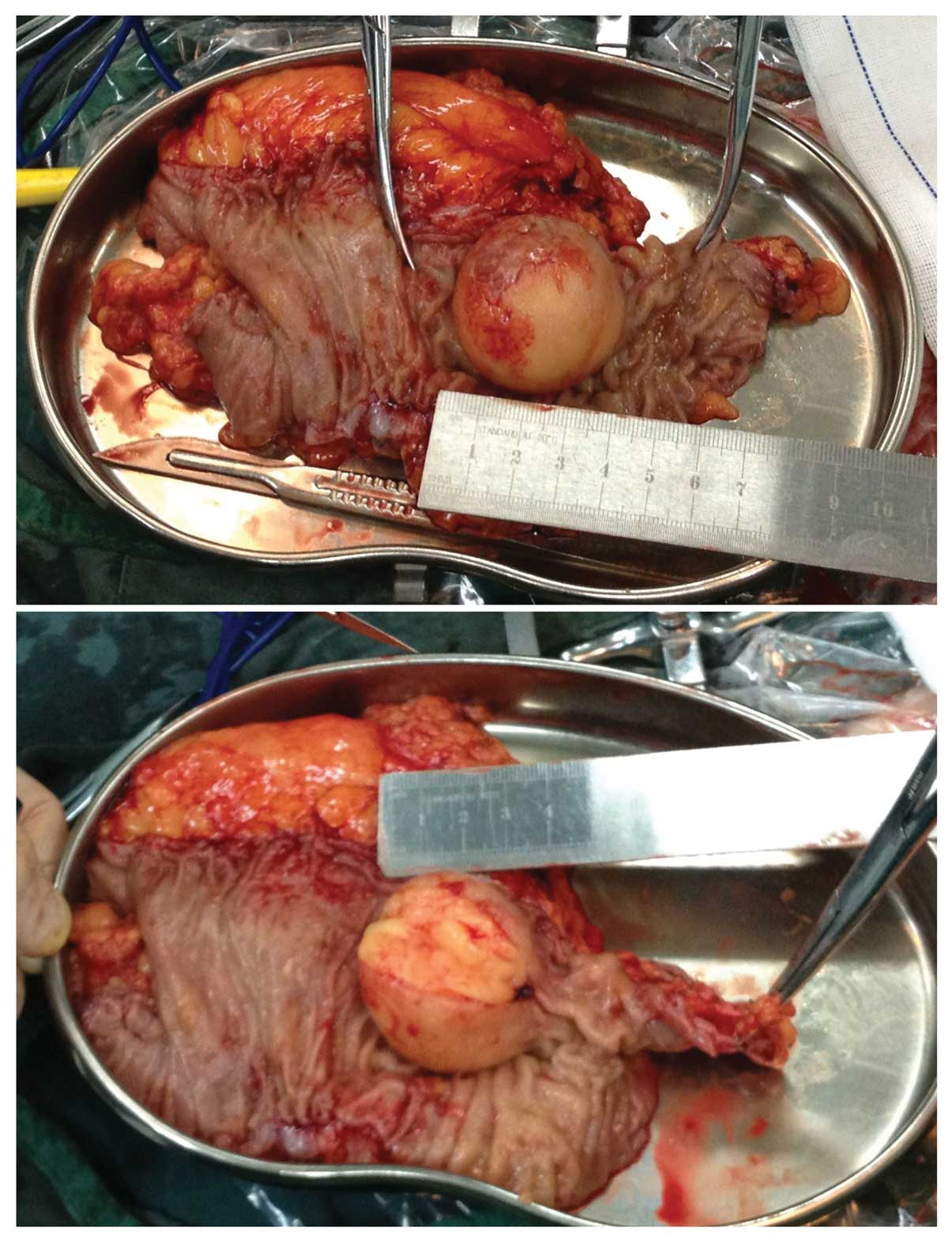
transverse colon. No further resection was required. Macroscopic
assessment of the resected specimen identified the presence of a
yellow, round and broader-based 4×4-cm mass exhibiting the features
of a lipoma (Fig. 3).
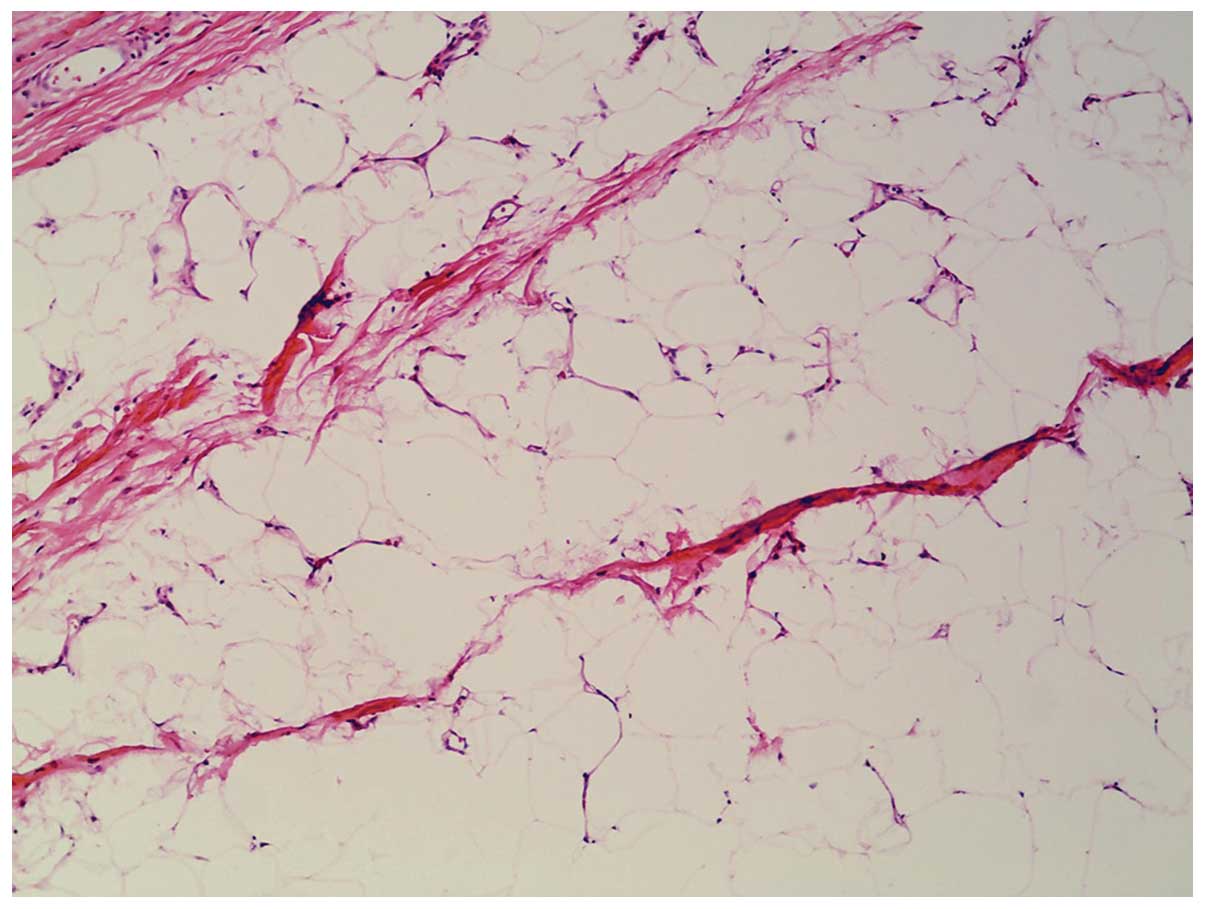
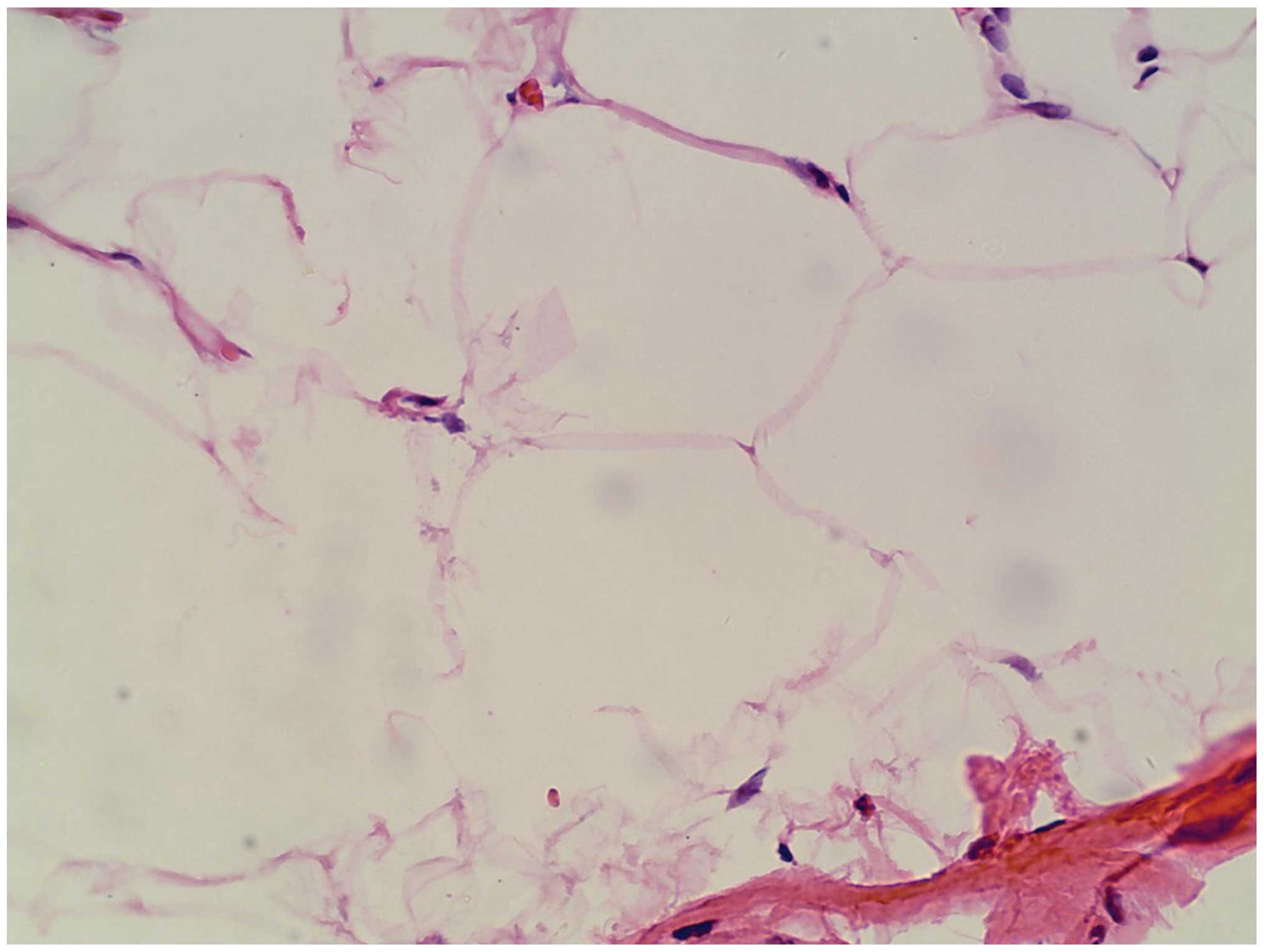
Histopathological examination of the resected specimen revealed
that the mass was composed of mature fat cells, focal erosion and
ulceration of the overlying colonic mucosa (Figs. 4 and 5). A conclusive diagnosis of a submucosal
lipoma of the transverse colon was achieved. The post-operative
course was uneventful. The patient was followed up for one year and
10 months following the segmental resection of the transverse
colon, with a good prognosis. Written informed consent was obtained
from the patient for the publication of this case study and any
accompanying images.
Discussion
Colonic lipomas are rare benign tumors of the
gastrointestinal tract and are classified as a type of benign
non-epithelial tumor. The incidence of colonic lipoma ranges
between 0.035 and 4.4% (9), and the
peak incidence occurs within the fifth and sixth decades of life,
most commonly in females (7,10).
Usually, colonic lipoma is solitary, with the most common locations
for solitary colonic lipoma being the ascending colon and cecum,
followed by the transverse colon, descending colon, sigmoid colon
and rectum (7). The majority of
colonic lipomas are asymptomatic and do not require treatment,
however, a small number may cause symptoms when the lesion is
large, particularly those with a diameter >2 cm (11). Colonic intussusception is also a
rare complication of colonic lipoma (12).
The size of colonic lipomas ranges between 2 mm and
30 cm and may mimic colonic malignancies (13). The present case revealed that large
colonic lipomas and malignant tumors may be difficult to
differentiate prior to resection if only endoscopic observations
are used. Due to the non-specific clinical presentations and
endoscopic appearance, including the multiple areas of erosion and
ulceration that were identified on the mass surface, together with
the relatively hard texture, the two may be indistinguishable.
However, for colonic lipomas of a large size and in acutely ill
patients, CT is the preferred diagnostic method, as the imaging
characteristics of the tumors are fairly typical for adipose tissue
(14).
However, an intraoperative frozen section may
provide an accurate diagnosis to guide surgery (15). In the present case, the
pre-operative biopsy during colonoscopy revealed numerous
ulcerative lesions with local epithelial regeneration, without
malignant tumor cells. The patient underwent segmental resection of
the transverse colon and intraoperative frozen sections were
obtained. As a result of the intraoperative frozen sections, which
revealed a submucosal lipoma of the transverse colon, an
unnecessary radical resection was avoided.
In conclusion, colonic lipoma is a relatively rare
benign tumor, which as a clinical entity may be easily misdiagnosed
as a malignant tumor. The clinical awareness of colonic lipomas
must be increased. Open surgery combined with the use of
intraoperative frozen sections should be recommended for large
symptomatic colonic lipomas accompanied by colonic intussusception,
thus avoiding unnecessary radical resection and improving the
patient prognosis.
References
|
1
|
Ryan J, Martin JE and Pollock DJ: Fatty
tumours of the large intestine: a clinicopathological review of 13
cases. Br J Surg. 76:793–796. 1989.
|
|
2
|
Bardají M, Roset F, Camps R, Sant F and
Fernández-Layos MJ: Symptomatic colonic lipoma: differential
diagnosis of large bowel tumors. Int J Colorectal Dis. 13:1–2.
1998.
|
|
3
|
Jiang L, Jiang LS, Li FY, et al: Giant
submucosal lipoma located in the descending colon: a case report
and review of the literature. World J Gastroenterol. 13:5664–5667.
2007.
|
|
4
|
Atmatzidis S, Chatzimavroudis G, Patsas A,
et al: Pedunculated cecal lipoma causing colo-colonic
intussusception: a rare case report. Case Rep Surg.
2012:2792132012.
|
|
5
|
Ladurner R, Mussack T, Hohenbleicher F,
Folwaczny C, Siebeck M and Hallfeld K: Laparoscopic-assisted
resection of giant sigmoid lipoma under colonoscopic guidance. Surg
Endosc. 17:1602003.
|
|
6
|
Ullah S, Ahmed H and Jehangir E: Giant
colonic lipoma presenting with intermittent intestinal obstruction.
J Coll Physicians Surg Pak. 22:792–793. 2012.
|
|
7
|
Rogy MA, Mirza D, Berlakovich G,
Winkelbauer F and Rauhs R: Submucous large-bowel lipomas -
presentation and management. An 18-year study. Eur J Surg.
157:51–55. 1991.
|
|
8
|
Lee CS, Lee MJ, Kim KL, et al: A case of
giant lipoma causing chronic recurrent intussusception of the
colon. Clin Endosc. 45:165–168. 2012.
|
|
9
|
Goasguen N, Cattan P, Godiris-Petit G, et
al: Colonic lipoma: case report and literature review.
Gastroenterol Clin Biol. 32:521–524. 2008.(In French).
|
|
10
|
Chung YF, Ho YH, Nyam DC, Leong AF and
Seow-Choen F: Management of colonic lipomas. Aust N Z J Surg.
68:133–135. 1998.
|
|
11
|
Kim CY, Bandres D, Tio TL, Benjamin SB and
Al-Kawas FH: Endoscopic removal of large colonic lipomas.
Gastrointest Endosc. 55:929–931. 2002.
|
|
12
|
Rogers SO Jr, Lee MC and Ashley SW: Giant
colonic lipoma as lead point for intermittent colo-colonic
intussusception. Surgery. 131:687–688. 2002.
|
|
13
|
Lazaraki G, Tragiannidis D, Xirou P, Nakos
A, Pilpilidis I and Katsos I: Endoscopic resection of giant lipoma
mimicking colonic neoplasm initially presenting with massive
haemorrhage: a case report. Cases J. 2:64622009.
|
|
14
|
Liessi G, Pavanello M, Cesari S,
Dell’Antonio C and Avventi P: Large lipomas of the colon: CT and MR
findings in three symptomatic cases. Abdom Imaging. 21:150–152.
1996.
|
|
15
|
Wang L, Chen P, Zong L, Wang GY and Wang
H: Colon angiolipoma with intussusception: a case report and
literature review. World J Surg Oncol. 11:692013.
|