Introduction
Osteosarcoma is rare in the head and neck,
accounting for <0.5% (1) of all
malignancies of this type. The majority of osteosarcomas in the
head and neck are reported to occur in the mandible or maxilla, and
few (10%) occur in the skull and facial bones (2). Osteosarcoma arising in the
parapharyngeal space is extremely rare. The current study presents
this unusual case due to the rarity of the site, and subsequently
discusses osteosarcoma of the parapharyngeal space.
Case report
A 56-year-old male presented with a mass in the
right facial bone that had been apparent for three months, and
dysesthesia, which had occurred gradually at this site. The patient
incidentally identified the tumor and visited Wakakusa-Daiichi
Hospital, Higashi-Osaka (Osaka, Japan), where the mass was
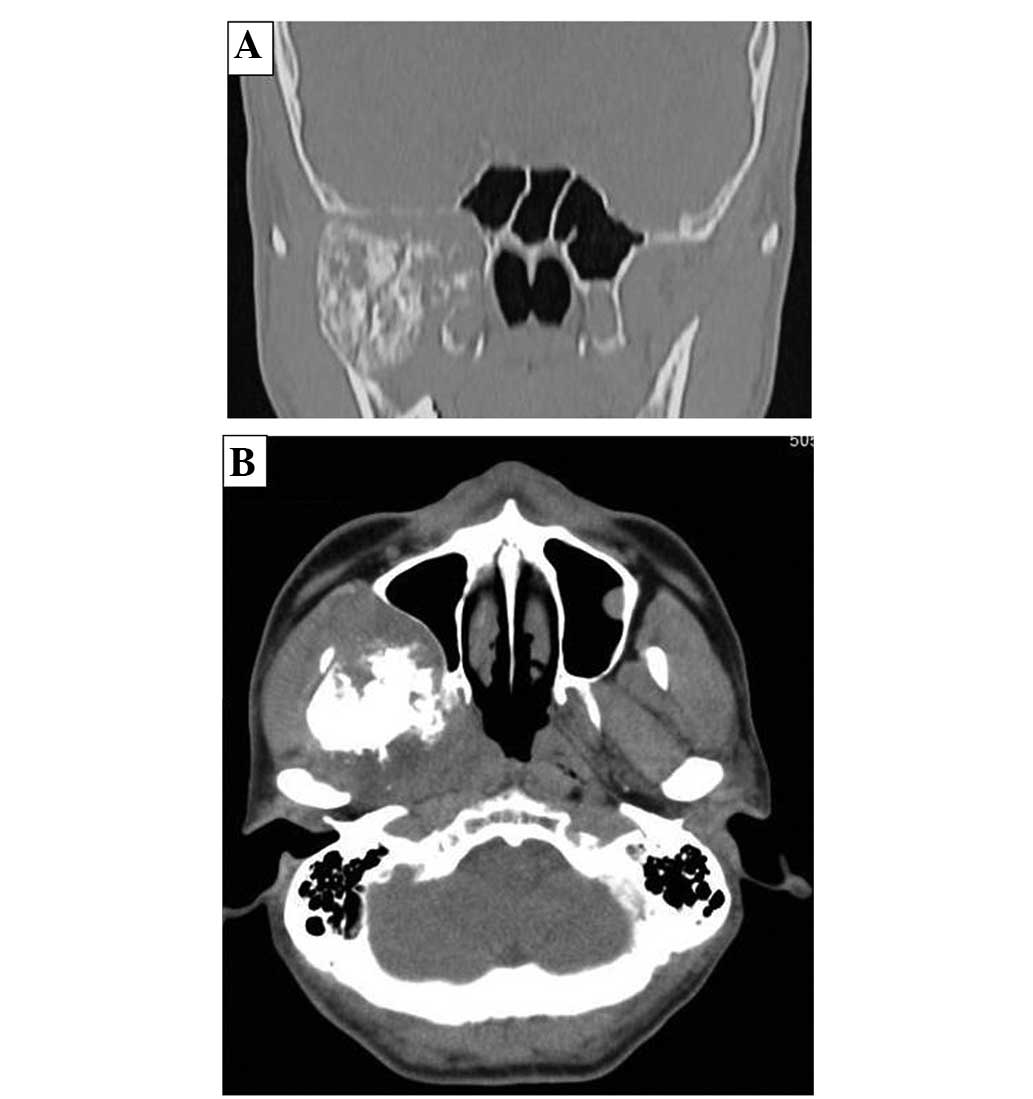
confirmed with computed tomography (CT) examination. Nothing of
note was found in the patient’s past medical and family histories,
and the findings from the routine laboratory studies were within
the normal limits. Plain X-rays showed no particular findings, but
regional CT showed a soft-tissue mass with prominent ossification
in the central region, and involving the parapharyngeal space
(Fig. 1), in which the anterior
septum ballooned owing to compression from the mass. Magnetic
resonance imaging (MRI) revealed heterogeneously low intensity to
isointensity results on T1-weighted sequences and low to moderately
high intensity results on T2-weighted images, with a size of
5.6×4.8 cm (Fig. 2). Lung CT
revealed multiple small nodules that were suspected to be lung
metastases (Fig. 3).
An open biopsy was performed, and histologically,
the lesion showed atypical cell proliferation with production of
calcified malignant osteoid. The pathological diagnosis was of an
osteoblastic osteosarcoma (Fig. 4).
The disease was classified as advanced-stage IVB. At first,
systemic chemotherapy was started with caffeine-assisted systemic
high-dose chemotherapy, consisting of 60 mg/m2
Adriamycin and 120 mg/m2 cisplatin. However, subsequent
to two courses of the regimen, a perforation of the sigmoid colon
was found, and surgical repair was immediately performed with a
colostomy. Moreover, irreversible renal dysfunction occurred, and
this was worsened by sepsis following surgery. No discernable
effect was observed from the chemotherapy on the mass in the
parapharyngeal space and the lung target lesion. High-dose
chemotherapy was deemed to be unsuitable for treating conventional
osteosarcoma owing to the adverse effects. Thus, local radiation
therapy, with a total dose of 39 Gy, and a total of seven courses
of low-dose systemic chemotherapy (50–100mg/m2
cyclophospamide per day) for palliation, were administered. At the
last follow-up, 24 months after the first visit, the size of the
mass occupying the parapharyngeal space was unchanged, but the size
and number of lung metastases had increased. At the time of writing
this study, the patient was alive with the disease. Written
informed consent was obtained from the patient for publication of
this case study and the accompanying images.
Discussion
Osteosarcoma is a primary high-grade malignant tumor
in which the neoplastic cells produce osteoid (3). Osteosarcoma affects males more
frequently than females. Young adolescents and adults under the age
of 25 years are predominantly affected. Osteosarcoma usually arises
in the bones around the knee, humeral joint and pelvis (4). The five-year survival rate is
generally estimated to be 60–80% (3). However, the incidence of osteosarcoma
in the head and neck regions is extremely low, and this form is
reported to occur in adults in their 30s and older (5). Cranial facial lesions account for
<10% of the total cases of osteosarcoma; these occur in the
mandible and maxillary bones in particular. However it is difficult
to find studies on osteosarcoma involving the parapharyngeal space
(6).
Radiologically, tumor matrix mineralization and
aggressive bone destruction are strongly suggestive of
osteosarcoma. The present case demonstrated a high-density mass in
the central area of the tumor on CT examination. On MRI, an
intermediate intensity region was observed T1-weighted images and a
heterogeneously high intensity region was observed on T2-weighted
images. An ossified region in the central lesion, which was
produced by tumor cells, showed a low intensity on each of the T1-
and T2-weighted images. There was no discernible bone-forming
reaction to indicate an osteosarcoma (7).
Histologically, osteosarcoma is an osteoid-producing
tumor, and the identification of anaplastic stromal cells and the
osteoid they produce aid in the histological diagnosis. The
incidence of the classic type of osteosarcoma presents as
osteoblastic (50%), chondroblastic (25%), or fibroblastic (25%) in
the extremities (3). Among head and
neck osteosarcomas, chondroblastic osteosarcoma is the most common
histopathological variant (8),
while osteoblastic osteosarcoma is associated with a poor
prognosis, differing from the chondroblastic type in the
extremities (5).
Osteosarcoma usually presents with an aggressive
course, with a high rate of distant metastasis and recurrence. In
the absence of distant metastasis, the major therapeutic approach
is surgery to achieve local control for high-grade osteosarcoma;
surgery with a negative margin is necessary (9), and multimodality management, in
addition to chemotherapy (10) and
radiotherapy (11), is preferable.
The anatomical site of the parapharyngeal space occupied by the
tumor is adjacent to more critical structures in the head and neck,
and radical surgery would have great disadvantages in terms of
function and possible cosmetic problems. However, systemic
chemotherapy with high-dose treatment may be the main treatment for
cases with distant metastases. The adverse effect of irreversible
renal dysfunction emerged in the present case following the two
initial courses of chemotherapy, and high-dose chemotherapy could
not be recommended.
The five-year survival rate of patients with head
and neck osteosarcoma is estimated to be 57–63% (2,11),
which is lower than the 70–80% survival rate of patients with
osteosarcoma of the extremities (12). Regarding prognostic factors, Smith
et al (5) proposed that a
poor prognosis is associated with an age of >60 years, a
non-mandibular tumor location, a tumor size of >6 cm, an
osteoblastic histological type, an advanced disease stage,
non-surgical initial therapy and a positive margin of resection. At
the latest follow-up, the present patient was alive with the
disease, but unfortunately possessed a number of these poor
prognostic factors.
In conclusion, the present study presents a rare
case of osteoblastic osteosarcoma arising from a rare lesion of the
parapharyngeal space. Although a definitive diagnosis requires a
biopsy, the CT and MRI findings described in this study suggest the
inclusion of this rare tumor in the differential diagnosis when
such findings occur in the parapharyngeal space.
References
|
1
|
de Fries HO, Perlin E and Leibel SA:
Treatment of osteogenic sarcoma of the mandible. Arch Otolaryngol.
105:358–359. 1979.
|
|
2
|
Canadian Society of Otolaryngology-Head
and Neck Surgery Oncology Study Group. Osteogenic sarcoma of the
mandible and maxilla: a Canadian review (1980–2000). J Otolaryngol.
33:139–144. 2004.
|
|
3
|
Raymond AK, Ayala AG and Knuuutila S:
Conventional osteosacoma. Fletcher CDM, Unni KK and Mertens F:
World Health Organization Classification of Tumors: Pathology and
Genetics; Tumors of Soft Tissue and Bone. 4. IARC Press; Lyon: pp.
264–270. 2002
|
|
4
|
Unni KK, Inwards CY, Kindblom LG and Wold
LE: Osteosarcoma of bone. Tumors of the Bones and Joints umors of
the bones and joints. (AFIP atlas of tumor pathology, series 4).
American Registry of Pathology; Washington DC: pp. 135–170.
2005
|
|
5
|
Smith RB, Apostolakis LW, Karnell LH, Koch
BB, Robinson RA, Zhen W, Menck HR and Hoffman HT: National Cancer
Data Base report on osteosarcoma of the head and neck. Cancer.
98:1670–1680. 2003.
|
|
6
|
Dorfman HD and Czerniak B: Osteosarcoma.
Bone Tumors. Mosby, Inc; St. Louis: pp. 128–253. 1998
|
|
7
|
Park HR, Min SK, Cho HD, Cho SJ, Lee JH,
Lee Y and Park YK: Osteosarcoma of the ethmoid sinus. Skeletal
Radiol. 33:291–294. 2004.
|
|
8
|
Laskar S, Basu A, Muckaden MA, D’Cruz A,
Pai S, Jambhekar N, Tike P and Shrivastava SK: Osteosarcoma of the
head and neck region: lessons learned from a single-institution
experience of 50 patients. Head Neck. 30:1020–1026. 2008.
|
|
9
|
Patel SG, Meyers P, Huvos AG, Wolden S,
Singh B, Shaha AR, Boyle JO, Pfister D, Shah JP and Kraus DH:
Improved outcomes in patients with osteogenic sarcoma of the head
and neck. Cancer. 95:1495–1503. 2002.
|
|
10
|
Tsuchiya H, Tomita K, Mori Y, Asada N and
Yamamoto N: Marginal excision for osteosarcoma with caffeine
assisted chemotherapy. Clin Orthop Relat Res. 358:27–35. 1999.
|
|
11
|
Guadagnolo BA, Zagars GK, Raymond AK,
Benjamin RS and Sturgis EM: Osteosarcoma of the jaw/craniofacial
region: outcomes after multimodality treatment. Cancer.
115:3262–3270. 2009.
|
|
12
|
Kawaguchi N, Ahmed AR, Matsumoto S, Manabe
J and Matsushita Y: The concept of curative margin in surgery for
bone and soft tissue sarcoma. Clin Orthop Relat Res. 419:165–172.
2004.
|