Introduction
Cystic lymphangioma, also known as cystic hygroma,
is a congenital malformation originating from lymphatic
hyperplasia. Cystic lymphangioma is a type of hamartoma and verges
on the clinical boundary between tumor and deformity. The majority
of lymphangiomas are observed in patients under the age of five
(1), with extremely few cases
reported in adulthood. This disease can occur in various areas of
the body, with the most common location being the neck. Usually,
the tumors are slow-growing, with an asymptomatic clinical course.
Cystic lymphangiomas are commonly soft and painless masses, but
cannot easily be compressed.
Cystic mediastinal lymphangioma (CML) is an
extremely uncommon benign cystic lymphangioma developed from the
lymphatic vessels. With regard to cystic lymphangioma, only ~1% are
mediastinal (2). CMLs are most
often located in the anterior mediastinum. In order to improve the
diagnosis and treatment of CML in clinical practice, knowledge on
the topic must be compiled and shared. The present study reports
the case of a giant anterior CML for this purpose. Patient provided
written informed consent.
Case report
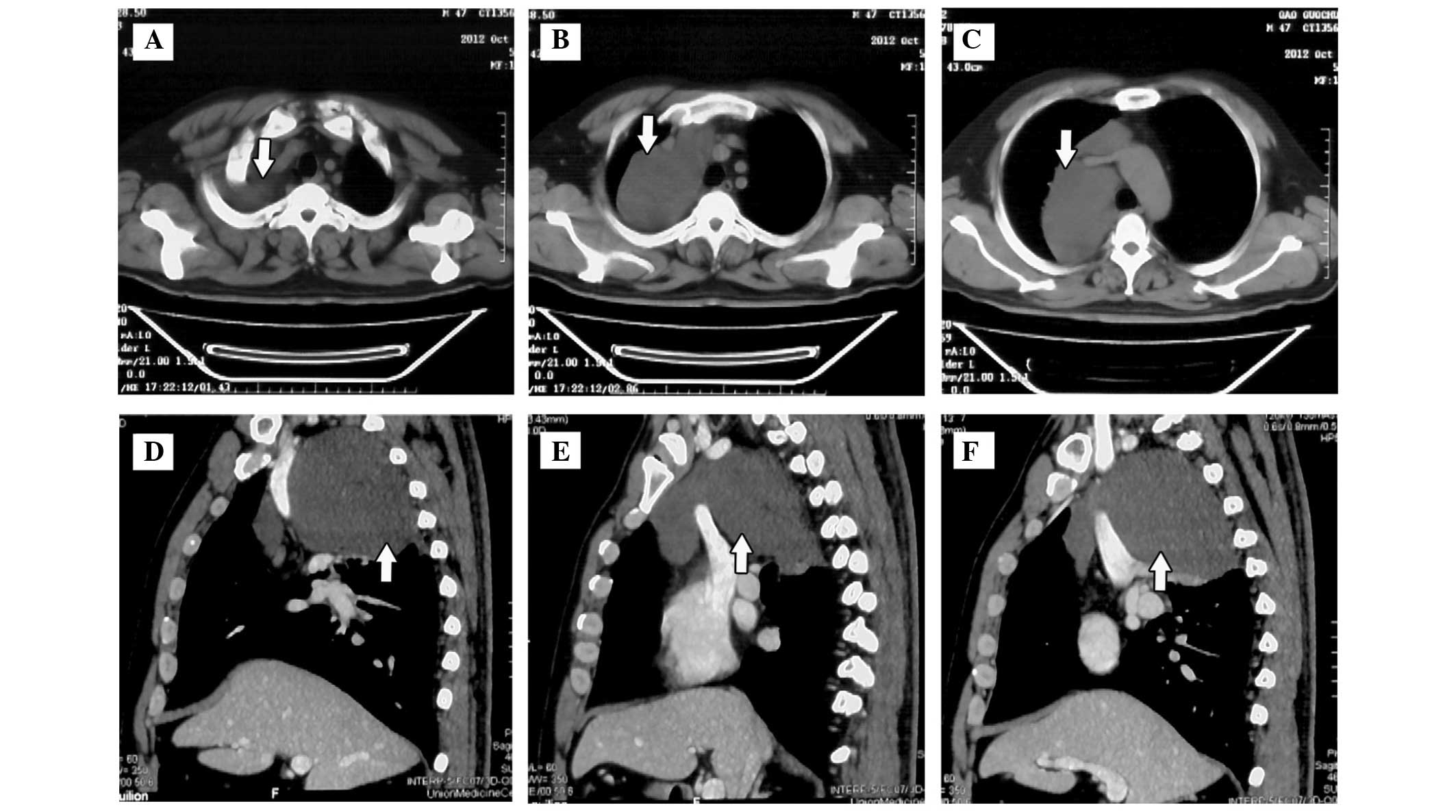
A 46-year-old, male, non-smoker was diagnosed with a
right anterior mediastinal tumor by computed tomography (CT) scan
during a physical examination in October 2012 (Fig. 1). No significant previous medical
history was reported and no specific clinical manifestations.
Examinations performed prior to surgery included test of pulmonary
function and narrow band imaging bronchoscopy, and no abnormal
findings were observed. The results of the analysis for
tuberculosis (TB) antibody and TB-DNA in the serum were all
negative. Serum tumor markers for lung carcinoma, including
carcinoembryonic antigen, carbohydrate antigen-125 (CA-125),
squamous cell carcinoma (SCC), CA72-4, cytokeratin 19 fragments,
neuron-specific enolase and ferritin were all within the normal
ranges. The initial tentative diagnosis was of a thymoma or
bronchocele.
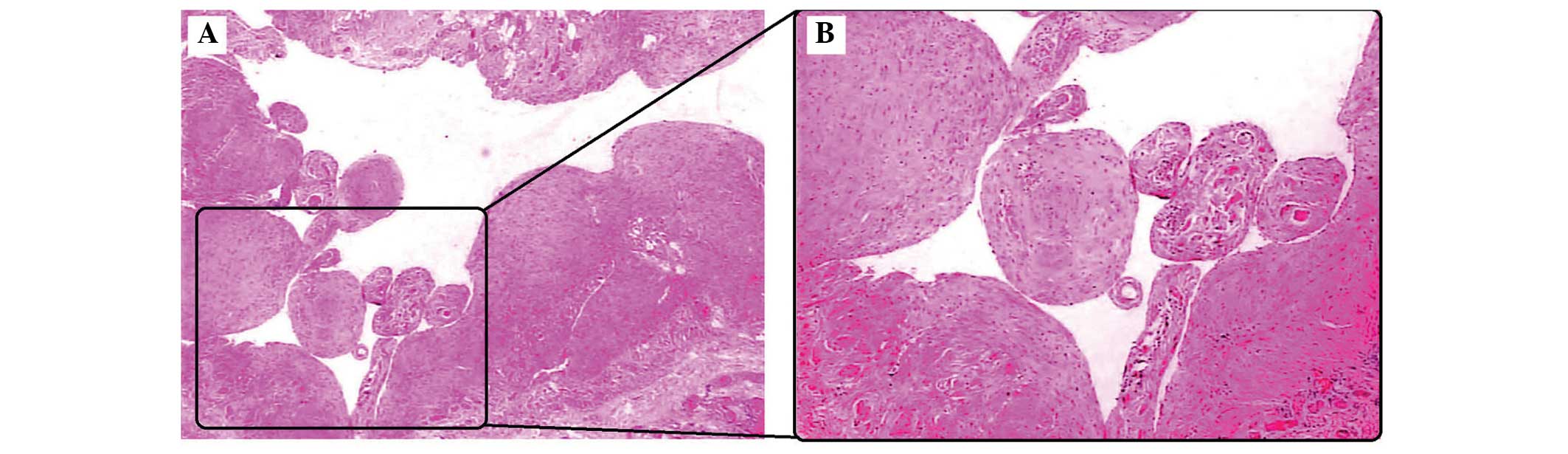
Subsequently, the lung resection of the mediastinal
tumor was performed by video-assisted thoracoscopy. A cystic and
globose tumor, with the largest diameter of 18.0 cm, was located in
the lateral section of the right anterior mediastinum (Fig. 2A). Following separation of the cyst
wall from the base, the cystic wall was removed (Fig. 2B). During the surgery, ~400 ml of
pale yellow liquid was absorbed from the cystic cavity (Fig. 2C). Following resection of the cystic
wall and hematoxylin-eosin staining, the histopathology was
observed under a light microscope (Nikon Eclipse 80i; Nikon, Tokyo,
Japan). The postoperative pathological examination of the cystic
wall showed multilocular cystic cavity in the cystic wall,
surrounded by smooth muscle and lymphoid tissue, as well as the
neoplasm. As a result, a diagnosis of CML was determined (Fig. 3). At the one-year follow-up there
were no signs of recurrence.
Discussion
Mainly occurring in childhood, cystic lymphangiomas
are extremely rare, with 90% being diagnosed prior to two years of
age. A limited number of studies exist with regard to cystic
lymphangioma in adults (3). CML is
an extremely rare vascular tumor originating from the lymphatic
vessels. In total, <1% of cystic lymphangiomas occur in the
mediastinum and >90% are discovered in individuals under two
years old (4). CML is benign and is
usually an incidental finding unless there are symptoms caused by
compression of local tissues and structures or infection. The CT
images of CML often resemble adenopathy or a mass. For adult
patients, the probable diagnosis would be of a thymoma, bronchocele
or malignancy.
Complete resection may be difficult in certain cases
due to their proximity to vital structures in the mediastinum
(5). Although other treatment
methods, such as sclerotherapy and radiotherapy, have been reported
in unresectable cases, they are generally ineffective and may
result in hemorrhage and infection (6). Therefore, surgery remains the superior
method for treatment with curative intent. Complete surgical
resection remains the treatment of choice for lymphangioma in order
to eliminate symptoms and prevent recurrences (7). The risk of tumor recurrence due to an
incomplete excision ranges between 0 and 13.6%, while the
aspiration of cystic fluid only decreases cyst size for a short
time and introduces the patient to the risk of infection (8). Currently, there are few documented
cases of giant CML (9–11). In the present study, the largest
diameter of the CML was 18.0 cm and the volume removed from the
cystic cavity during surgery was ~400 ml. Histological analysis,
the gold standard method, was able to confirm the CML
diagnosis.
In summary, CML, particularly giant CML, is
extremely rare in adults. Complete surgical resection provides a
definitive histological diagnosis and prevents recurrence.
References
|
1
|
Chung JH, Suh YL, Park IA, Jang JJ, Chi
JG, Kim YI and Kim WH: A pathologic study of abdominal
lymphangiomas. J Korean Med Sci. 14:257–262. 1999.
|
|
2
|
Minato H, Kaji S, Kinoshita E, Kurose N,
Nojima T, Kohno M, Konuma K and Ikawa H: Solitary intrapulmonary
cystic lymphangioma in an infant: a case report with literature
review. Pathol Res Pract. 206:851–856. 2010.
|
|
3
|
Kambakamba P, Lesurtel M, Breitenstein S,
Emmert MY, Wilhelm MJ and Clavien PA: Giant mesenteric cystic
lymphangioma of mesocolic origin in an asymptomatic adult patient.
J Surg Case Rep. 2012:42012.
|
|
4
|
Khabbaza J, Sethi S, Raymond D and Almeida
F: Mediastinal cyst mimicking malignancy in a pipe smoker. Chest.
144:21A2013.
|
|
5
|
Singh O, Singh Gupta S, Upadhyaya VD,
Sharma SS, Lahoti BK and Mathur RK: Cystic lymphangioma of the
breast in a 6-year-old boy. J Pediatr Surg. 44:2015–2018. 2009.
|
|
6
|
Celikten A, Melek H, Citak N, Metin M,
Sayar A, Urer N and Gürses A: Minimally invasive excision of
multiple cystic lymphangiomas of the mediastinum: a case report.
Thorac Cardiovasc Surg. 58:498–500. 2010.
|
|
7
|
Aprea G, Guida F, Canfora A, Ferronetti A,
Giugliano A, Ciciriello MB, Savanelli A and Amato B: Mesenteric
cystic lymphangioma in adult: a case series and review of the
literature. BMC Surg. 13(Suppl 1): A42013.
|
|
8
|
Mohite PN, Bhatnagar AM and Parikh SN: A
huge omental lymphangioma with extension into labia majorae: a case
report. BMC Surg. 6:182006.
|
|
9
|
Fisher D and Hiller N: Case report: giant
tuberculous cystic lymphangioma of posterior mediastinum,
retroperitoneum and groin. Clin Radiol. 49:215–216. 1994.
|
|
10
|
Bossert T, Gummert JF and Mohr FW: Giant
cystic lymphangioma of the mediastinum. Eur J Cardiothorac Surg.
21:3402002.
|
|
11
|
Khobta N, Tomasini P, Trousse D, Maldonado
F, Chanez P and Astoul P: Solitary cystic mediastinal lymphangioma.
Eur Respir Rev. 22:91–93. 2013.
|