Introduction
Esthesioneuroblastoma (ENB) is an uncommon malignant
neuroectodermal tumor originating from the olfactory membrane of
the sinonasal tract (1). The
various appellations include olfactory neuroblastoma,
esthesioneurocytoma, esthesioneuroepithelioma and olfactory placode
tumor (1,2). The incidence has been reported at 0.4
per million (1). Complete surgical
eradication including craniofacial resection followed by
radiotherapy is the cornerstone of treatment. Chemotherapy is
employed in patients with advance locoregional, local recurrent or
metastatic disease and is used as adjuvant therapy in high grade,
Kadish’s stage C, ENB (1,3). An endoscopic microsurgical technique
has gained wide acceptance for a novel therapeutic approach of ENB
(4). The overall five-year survival
rate is 78% (1). A regional
sinonasal involvement is characteristic, but metastasis is
uncommon. The most common metastatic sites are the cervical lymph
nodes, lungs and bone (1,2). Metastasis in the breast from
extramammary malignant neoplasm is uncommon (5). The present study reports of a rare
case of breast metastasis in a 30-year-old female with ENB
(Kadish’s stage C). The patient underwent a radical ethmoidectomy
with radiotherapy followed by chemotherapy including platinum-based
protocols.
Case report
Clinical summary
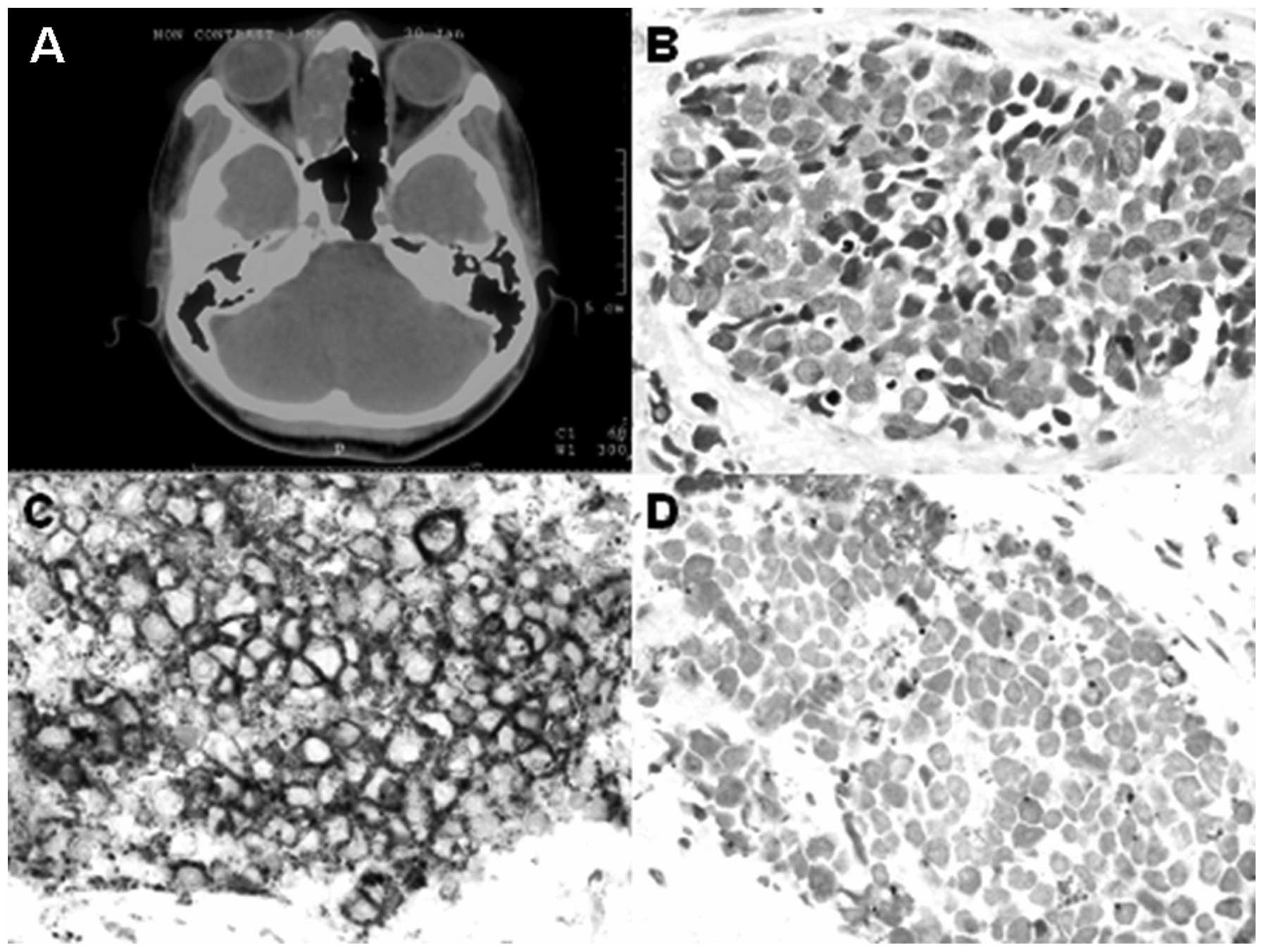
A 31-year-old Thai female with known ENB, Hyams’
histologic grade 2, Kadish’s stage C, T4N0M0, presented with a
rapidly enlarging lump of the right breast. Fourteen months
previously, the patient was referred to the Faculty of Medicine,
Ramathibodi Hospital (Bangkok, Thailand) due to nasal congestion. A
radical ethmoidectomy was performed and the pathology was shown to
be ENB with multiple foci of lymphovascular space invasion
(Fig. 1). The patient received
5,000 cGy of external beam radiotherapy, followed by postoperative
chemotherapy including five cycles of cisplatin and etoposide. The
patient was disease-free for seven months prior to presenting at
the hospital four days prior to this admission with a rapidly
enlarging lump in her right breast and a cervical lymphadenopathy.
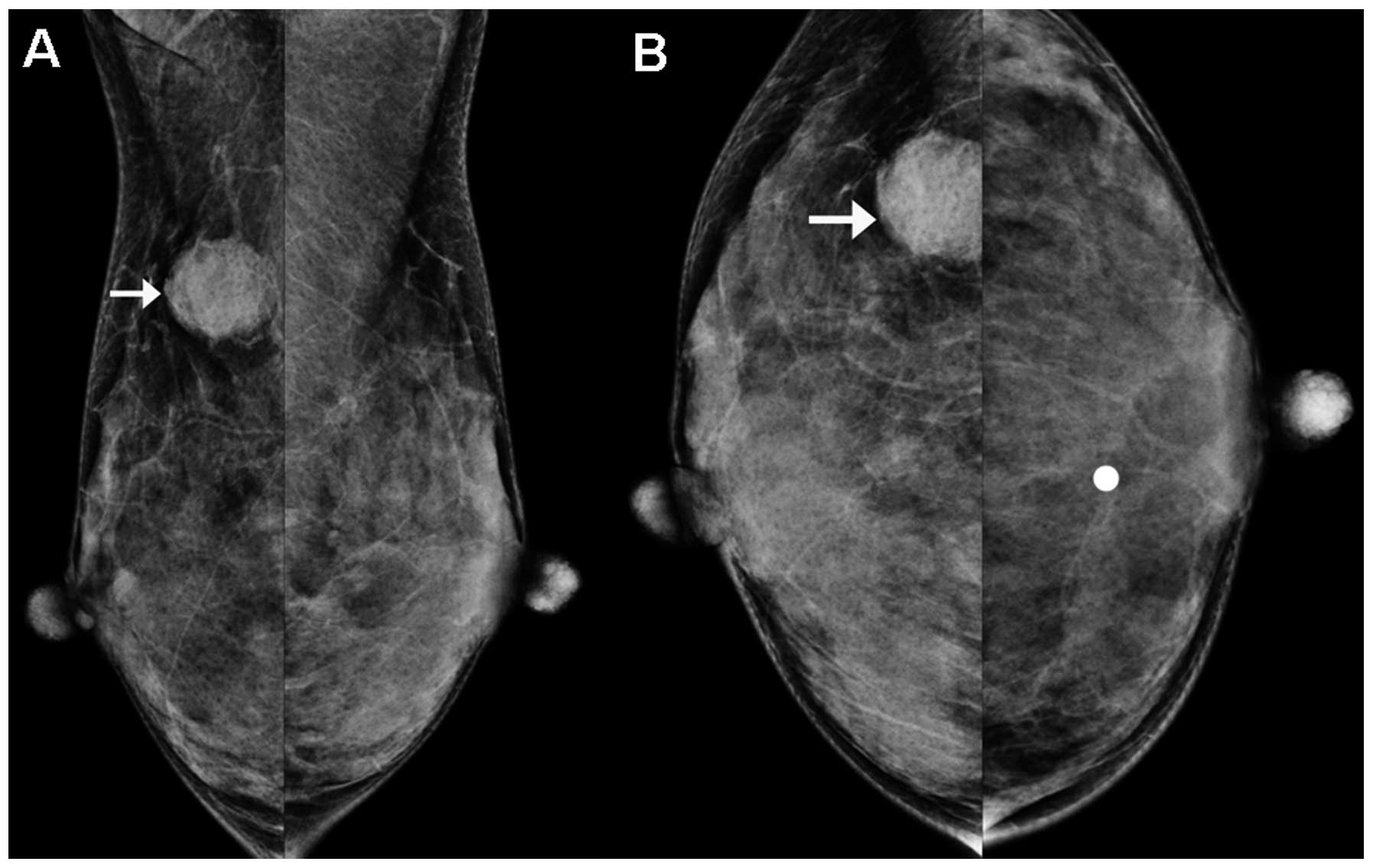
A physical examination revealed a palpable, 2.5-cm, firm and
movable mass in the right breast. A digital mammography showed a
hyperdense mass with circumscribed border in the background of
extremely dense fibroglandular mammary tissue at the upper outer
quadrant of the right breast (Fig.
2). No associated microcalcification was identified.
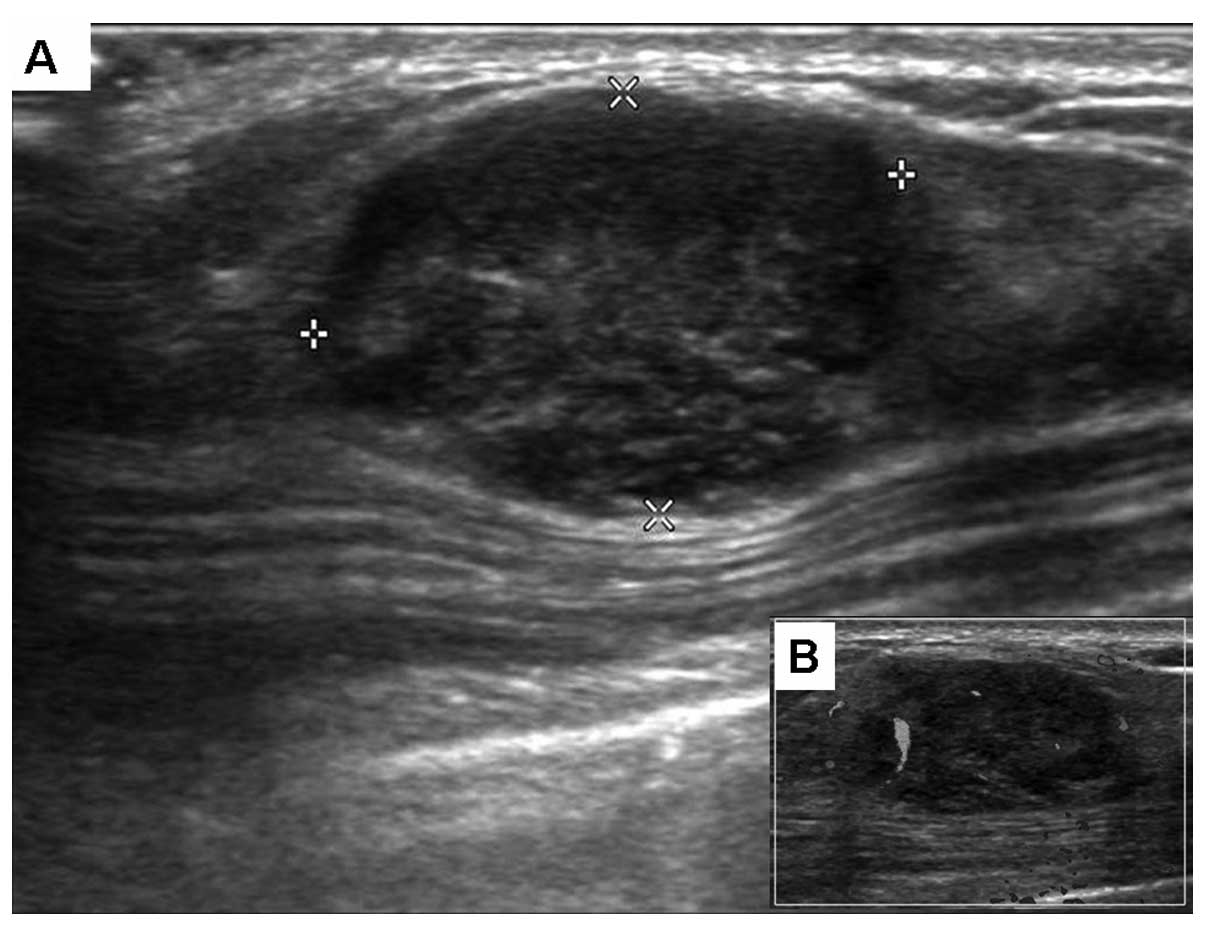
Ultrasonography showed a solid mass with heterogenous echogenicity
and a gently lobulated border measuring 2.2×1.4×2.6 cm. A posterior
acoustic enhancement was observed (Fig.
3A). Intralesional blood vessels were observed on the color
Doppler ultrasound (Fig. 3B). No
change of the overlying skin or axillary lymphadenopathy was
observed. The patient underwent a fine needle aspiration (FNA), and
a systemic work-up revealed pulmonary and mediastinal nodal
metastases. Subsequently, the patient received two courses of
chemotherapy, including vincristine, doxorubicin and
cyclophosphamide and 300 cGy of palliative radiation to the chest.
The patient then refused further treatment. Local recurrence and
systemic vertebral, pulmonary and nodal metastases were detected,
and the patient developed septicemia. Hemoculture grew Candida
albicans. The patient succumbed to the disease seven months
after the diagnosis of metastatic ENB to the right breast. No
autopsy was performed.
Cytopathological findings
FNA of the breast mass revealed neuroendocrine cells
with slightly pleomorphic hyperchromatic nuclei, salt and pepper
chromatin, indistinct nucleoli and scant cytoplasm (Fig. 4). Immunocytochemically, the
neuroendocrine cells were positive for CD56, and negative for
cytokeratin and gross cystic disease fluid protein-15.
Morphologically and immunocytochemically, these characteristics
were almost identical to the tumor observed in the sinonasal
ethmoidectomy specimen.
Discussion
The overall incidence of extramammary metastasis to
the breast is 0.2–1.3% of all malignant breast tumors (5). Patients with non-Hodgkin lymphoma,
melanoma, and carcinoma of the lung, stomach, ovary, kidney and
colorectum in adults and children with rhabdomyosarcoma, have a
higher risk of metastasis to the breast (5). Table I
compares the present rare case of ENB metastasis with two reported
cases of ENB metastasis to the breast that have been previously
described in the English literature (Table I) (6,7). The
patients had an average age of 20.3 years with a range of 13 to 30
years at the first time of diagnosis. All cases were at Kadish’s
stage C. Mammary metastasis was reported to appear during the
course of the treatment two years following the ENB diagnosis. The
patients typically presented with a palpable breast mass, generally
well-circumscribed and rapidly growing. All cases presented as a
right breast lump and all succumbed following the diagnosis of
esthesioneuroblastoma metastasis to the breast.
 | Table ISummary of cases of
esthesioneuroblastoma metastasis to the breast. |
Table I
Summary of cases of
esthesioneuroblastoma metastasis to the breast.
| Author (ref.) | Gender | Age at ENB diagnosis
(years) | Symptoms | Kadish’s stage | Radiotherapy
(cGy) | Chemotherapy | Interval between ENB
and breast metastasis (months) | Breast
metastasis | Systemic
metastasis | Survival |
|---|
|
|---|
| Side | Site | Size (mm) |
|---|
| Shetty et al
(4) | F | 13 | Left facial pain,
nasal obstruction, epiphora, anosmia and epistaxis | C | 5500 | Cyclophosphamide and
vincristine | During the course of
radiotherapy | Right | NP | NP | Bone marrow and right
ovary | Died during the
course of radiotherapy |
| Mrad et al
(5) | F | 18 | NP | C | NP | NP | 24 | Right | Lower inner
quadrant | 30 | Vertebra | Died |
| Present case | F | 30 | Nasal stuffiness | C | 5000 | Cisplatin and
etoposide | 7 | Right | Upper outer
quadrant | 22 | Vertebra, lung and
lymph node | Died 14 months after
diagnosis |
The mammographic and ultrasonographic appearances of
the extramammary neoplasm metastasis to the breast may mimic benign
mammary neoplasm and primary malignancy including carcinoma with
medullary features. Metastatic tumors to the breast have three
classic radiological patterns, consisting of: i) solitary tumor
with a well-circumscribed border (as was exhibited in the presented
case); ii) multiple diffuse and bilateral involvement; and iii)
diffuse skin and trabecular thickening (8–12).
Unlike the classical appearance of primary invasive mammary
carcinoma, particularly ductal subtype, a speculated border is
typically observed, since there is little or no desmoplastic
reaction. Microcalcification is not a typical feature of metastatic
tumors, with the exception of the previously reported case of
metastatic ovarian serous carcinoma with psammoma bodies (9). Awareness of the patient history of
extramammary cancer is essential in order to give an accurate
diagnosis. Mammographic and ultrasonographic imaging studies may
facilitate the diagnosis, but a full diagnosis should be
established after a cytohistopathologic biopsy is performed.
It is important to distinguish between a primary
mammary neoplasm and a metastasis in the breast, as well as to
consider the possibly of a metastasis from an extramammary
malignancy. This is particularly crucial with the increasing use of
fine needle aspiration. The combination of cytology and
immunocytochemistry is useful in separating metastasis from a
primary malignancy (13).
Identification and confirmation of the primary tumor is important
to facilitate treatment. The treatment of a metastatic tumor is
usually expectant and directed at treating the primary tumor. A
mastectomy is generally not performed for metastatic tumors in the
breast; however, wide excision may be performed to obtain local
control of bulky, ulcerated, bleeding, necrotic or otherwise
symptomatic lesions. The overall prognosis is dependent on the
histopathology, tumor grade and tumor stage of the primary
malignancy. Therefore, it is noteworthy to consider the possibility
of an ENB metastasis to the breast when diagnosing a mass lesion of
breast. Early diagnosis and prompt medical treatment are
essential.
ENB is a rare neoplasm originating from the
olfactory membrane of the sinonasal tract and has a high incidence
of local recurrence. A systemic metastasis is uncommon. The present
case report highlights the unusual site of a metastasis from ENB to
the breast. ENB metastasis to the breast commonly presents in young
adults, occurs with ENB with Kadish’s stage C, favors the right
breast, is accompanied by systemic metastasis, exhibits rapid
growth of mammary lump, has a poor response to chemotherapy and/or
radiotherapy, carries a short disease free survival and overall
survival, and portends a poor prognosis.
References
|
1
|
Wenig BM, Dulguerov P, Kapadia SB, et al:
World Health Organization Classification of Tumours of the Nasal
Cavity and Paranasal Sinuses: Neuroectodermal Tumours. Pathology
and Genetics of Head and Neck Tumours. Barnes EL, Eveson JW,
Reichart P and Sidransky D: IARC Press; Lyon: pp. 65–75. 2005
|
|
2
|
Finkelstein SD, Hirose T and VandenBerg
SR: World Health Organization Classification of Tumours. Olfactory
neuroblastoma. Pathology and Genetics of Tumours of the Nervous
System. Kleihues P and Cavenee WK: IARC Press; Lyon: pp. 150–152.
2000
|
|
3
|
Herr MW, Sethi RK, Meier JC, et al:
Esthesioneuroblastoma: an update on the massachusetts eye and ear
infirmary and massachusetts general hospital experience with
craniofacial resection, proton beam radiation, and chemotherapy. J
Neurol Surg B Skull Base. 75:58–64. 2014.
|
|
4
|
Gallia GL, Reh DD, Lane AP, Higgins TS,
Koch W and Ishii M: Endoscopic resection of esthesioneuroblastoma.
J Clin Neurosci. 19:1478–1482. 2012.
|
|
5
|
Lee A and Sahin A: World Health
Organization Classification of Tumours of the Breast. Metastases of
extramammary malignancies to the breast. Lakhani SR, Ellis IO,
Schnitt SJ, Tan PH and van de Vijver MJ: IARC Press; Lyon: pp.
162–163. 2012
|
|
6
|
Shetty SC, Gupta S, Chary G, et al:
Olfactory neuroblastoma metastatic to the breast. Rhinology.
38:144–146. 2000.
|
|
7
|
Mrad K, Mansouri D, Driss M, et al:
Esthesioneuroblastoma metastatic to the breast in a young woman.
Acta Cytol. 49:427–430. 2005.
|
|
8
|
Feder JM, de Paredes ES, Hogge JP and
Wilken JJ: Unusual breast lesions: radiologic-pathologic
correlation. Radiographics. 19:S11–S26. 1999.
|
|
9
|
Recine MA, Deavers MT, Middleton LP, Silva
EG and Malpica A: Serous carcinoma of the ovary and peritoneum with
metastases to the breast and axillary lymph nodes: a potential
pitfall. Am J Surg Pathol. 28:1646–1651. 2004.
|
|
10
|
Qureshi SS, Shrikhande SV, Tanuja S and
Shukla PJ: Breast metastases of gastric signet ring cell carcinoma:
a differential diagnosis with primary breast signet ring cell
carcinoma. J Postgrad Med. 51:125–127. 2005.
|
|
11
|
Gupta S, Gupta MK, Gupta R and Mishra RS:
Breast metastasis of cervical carcinoma diagnosed by fine needle
aspiration cytology: A case report. Acta Cytol. 42:959–962.
1998.
|
|
12
|
Alvarez RH, Gong Y, Ueno NT, et al:
Metastasis in the breast mimicking inflammatory breast cancer. J
Clin Oncol. 30:e202–e206. 2012.
|
|
13
|
Faragalla H and Weinreb I: Olfactory
neuroblastoma: a review and update. Adv Anat Pathol. 16:322–331.
2009.
|