Introduction
Fetal cardiac rhabdomyoma is a rare condition,
however, it is the most common cardiac tumor in fetuses, accounting
for 60–86% of primary fetal cardiac tumors (1). Fetal cardiac rhabdomyoma is most often
diagnosed by fetal echocardiography. Cardiac rhabdomyomas have a
tendency for spontaneous regression, however, they may cause
arrhythmias, hemodynamically significant obstruction, heart failure
and sudden mortality (2). Surgery
is not usually required, as cardiac rhabdomyoma often regress and
thus, may be managed conservatively and monitored by serial
echocardiograms and electrocardiograms, with the exception of cases
in which location leads to hemodynamic compromise or untreatable
arrhythmias (3). The present study
reports a rare case of fetal cardiac rhabdomyoma located in the
right atrium, accompanied by premature restriction of the foramen
ovale and moderate pericardial effusion, as determined by
tomographic ultrasound imaging (TUI) and confirmed by pathology.
Fetal mortality occurred late in the second trimester of pregnancy.
Written informed consent was obtained from the patient.
Case report
A 30-year-old female, gravid 2 para 0, was referred
to the Department of Ultrasound, Beijing Anzhen Hospital (Beijing,
China), following a routine prenatal ultrasound examination at
Cangzhou City Maternal and Child Care Service Centre (Cangzhou
City, China) where pericardial effusion (PE) was detected. The
patient had previously suffered a spontaneous abortion at 11 weeks
of pregnancy two years ago and the reasons for this remained
unclear. Two-dimensional (2D) and three-dimensional (3D) ultrasound
imaging was performed using the Voluson E8 ultrasound system (4–8
MHz probe; GE Healthcare, Cleveland, OH, USA). The evaluation
demonstrated a single live intrauterine pregnancy of 26 weeks. The
fetal echocardiography four-chamber view assessment demonstrated a
6.3-mm thickening of the right atrial wall. Moderate PE was also
observed. Color Doppler imaging indicated a narrow foramen ovale
flow of only 1.9 mm in diameter (Fig.
1). A bicaval view revealed superior vena cava and inferior
vena cava diameters of 3.0 mm and 3.4 mm, respectively. The patient
was informed of the possibility of fetal abnormalities and asked to
attend weekly follow-ups. However, the patient did not feel
quickening two days later and fetal mortality was diagnosed by
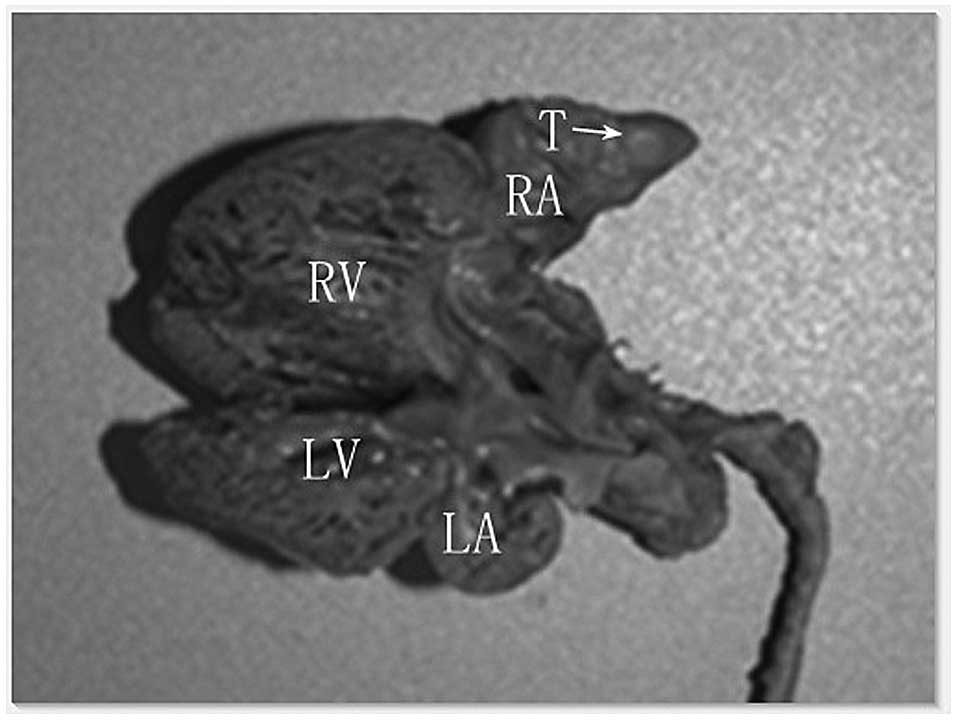
fetal echocardiography. An autopsy of the fetus revealed that the
heart was slightly enlarged, with a subendocardial nodule of
4.3×4.0 mm in size located in the right atrium. The nodule was
sharply demarcated, exhibiting a reddish-gray color with a
moderately firm texture and the typical appearance of a rhabdomyoma
(Fig. 2). Histological hematoxylin
and eosin staining revealed nodular hyperplasia with clear
boundaries, swirl-like cells, cords and a random orientation. The
tumor cells possessed a strong eosinophilic cytoplasm, with
slightly increased nuclear size and chromatin condensation.
However, atypia was not evident (Fig.
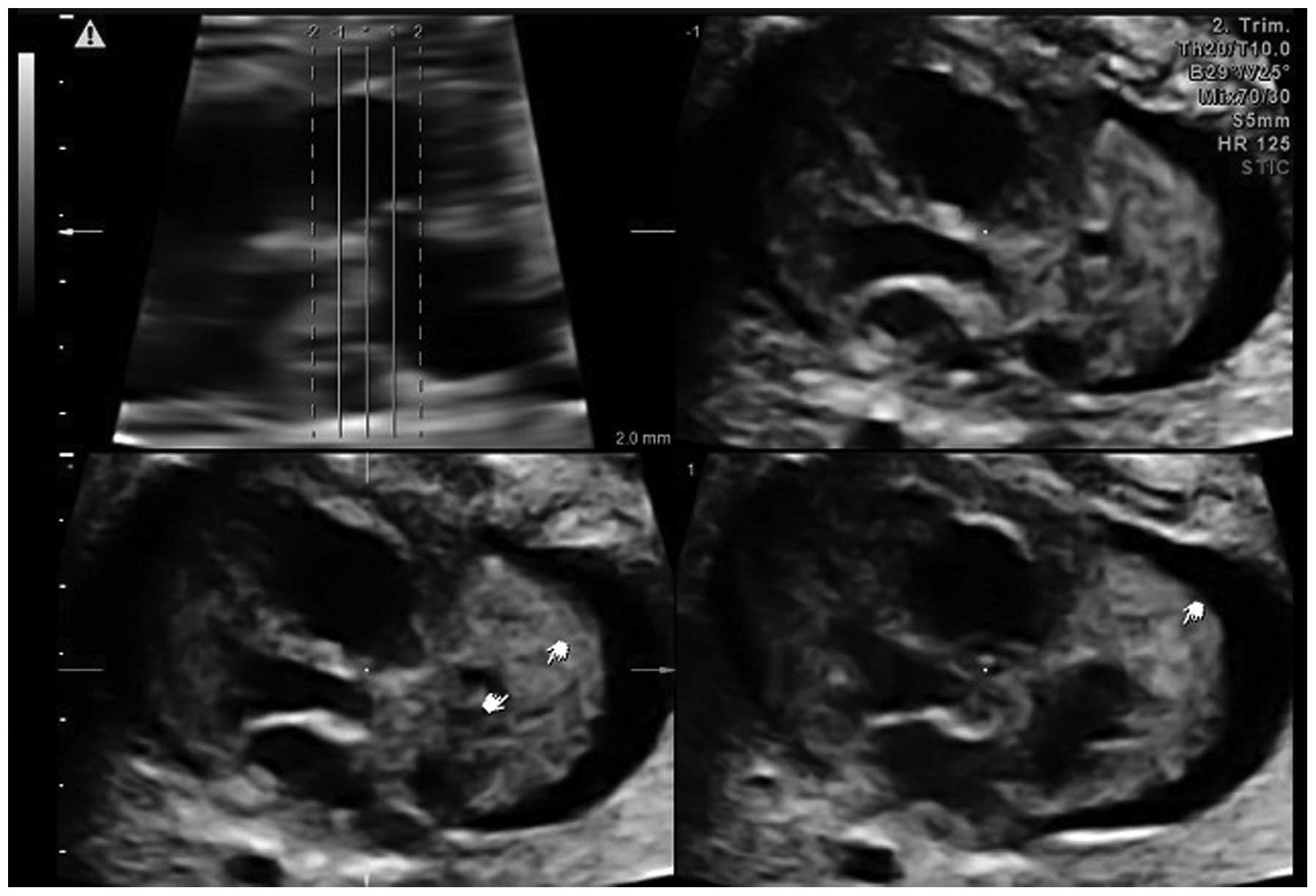
3A and B). The images were reviewed offline by tomographic
ultrasound imaging (TUI) and spatio-temporal image correlation
(STIC) imaging, which clearly displayed a 5.0×4.0-mm mass located
in the right atrial wall area (Fig.
4). No major or minor manifestations of tuberous sclerosis or
other notable family histories were documented.
Discussion
Fetal cardiac rhabdomyoma is the most common cardiac
tumor in fetuses, with an extremely low reported incidence rate in
fetal echocardiograms (0.17%) and accounting for 60–86% of primary
fetal cardiac tumors. Currently, fetal echocardiography is the
primary tool for the early detection of primary cardiac rhabdomyoma
(4). However, in the present case,
only right atrial wall thickening was observed, as the tumor was
not noticeable in traditional 2D imaging. A possible mass was
observed following offline review of the images using TUI. In
echocardiography, rhabdomyomas are often observed as round,
homogeneous and hyperechogenic ventricular masses, occasionally
appearing in the ventricles and septal wall areas of the atrium
(5). The occurrence of a single
tumor in the right atrium and masses in the pericardium are rare
(6). Although fetal cardiac
rhabdomyomas are histologically benign, the increased size and
hydrops are significantly associated with poor neonatal outcomes.
In certain cases, these features may cause intrauterine mortality.
Overall, the risk of fetal mortality is 4–6% (7).
The incidence of the premature restriction of
foramen ovale-accompanied tumors in the right atrium is rare.
Premature foramen ovale restriction can lead to pericardial or
pleural effusion, right-sided heart failure, dysrhythmia,
congestion, non-immune hydrops and ascites. Fetal mortality may be
associated with premature restriction of the foramen ovale. Also,
up to 80% of prenatally-diagnosed cardiac rhabdomyomas have been
associated with postnatal tuberous sclerosis complex (TSC)
(8). However, in the present case,
the parents had no family history of TSC.
Other cardiac tumors, including fibromas, teratomas,
hemangiomas and myxomas, are extremely rare (9). Fibromas differ from cardiac
rhabdomyoma, usually originate from the left ventricular apex and
are mostly solitary. Teratomas are extracardiac, with attachment to
the aortic root or pulmonary artery, and tend to grow within the
pericardial cavity. Myxomas are located in the atrium and have a
stalk that allows free movement during the cardiac cycle, and
hemangiomas are usually situated at the base of the heart adjacent
to the atria (10).
The ultrasound images in the present study suggested
a solid, non-calcified tumor located in the right atrium. The
differential diagnosis for this finding may include a rhabdomyoma,
teratoma or hemangioma, among other diagnoses. Although fetal
cardiac hemangiomas and teratomas are also often found in the right
atrium, hemangiomas demonstrate a more complex echogenicity, with
cystic and solid parts mixed with calcifications (11), while teratomas can be either cystic
or solid. The differential morphological characterization of
cardiac tumors requires fetal cardiac evaluation. As the use of
echocardiography to differentiate rhabdomyoma from teratoma or
hemangioma for a single cardiac mass located in the atrium is
occasionally difficult, the combination of other newly-developed
prenatal imaging techniques, including STIC, physician experience,
family history and patient symptoms, may be more appropriate for
the confirmation of the diagnosis (12). In the present study, it was
hypothesized that reviewing images offline by TUI mode with STIC
could reveal a solitary tumor located in the right atrium.
DeVore et al first reported the prenatal
diagnosis of a cardiac tumor in 1982 (13). The prenatal diagnosis of fetal
cardiac tumors has become feasible due to the advancement in fetal
echocardiography. TUI and STIC are two novel types of volume data
imaging techniques that are processed by 3D and 4D ultrasound. STIC
associated with the TUI mode is a novel modality, which allows for
the exhibition of a complete sequential analysis of cardiac
structures on a single panel that demonstrates all
echocardiographic transverse views at the same time. The fetal
cardiac rhabdomyoma diameter range has previously been reported to
be 4–52 mm in the majority of cases (14), which is consistent with the present
results, as the tumor size was 5.0×4.0 mm. However, it is difficult
to detect tumors of this size using the conventional 2D mode;
initially, only a thick fetal right atrial wall was identified in
the present study. By contrast, the tumor was clearly observed by
TUI and STIC. STIC is a technique that allows examination of the
fetal heart within a real-time 3D volume, through display in a
cine-loop. At the same time, real-time 3D echocardiography with
instantaneous volume rendering reveals mobile views of cardiac
tumors (15). Through surface
rendering of the STIC volume, an operator has the ability to
observe virtual planes that are impossible to observe by
conventional 2D ultrasound imaging. Thus, the 3D/4D ultrasound
modalities may have advantages at evaluating certain abnormalities
in the fetal cardiovascular structure (16).
In summary, the present study reports a case of rare
fetal cardiac rhabdomyoma located in the right atrium, accompanied
by premature restriction of the foramen ovale and moderate
pericardial effusion, which led to fetal mortality late in the
second trimester of pregnancy. It was demonstrated that TUI mode
with STIC offline imaging provides the physician with clear views
of abnormal intracardiac structures of the beating heart. With
improved sonographic technology, the diagnosis of fetal cardiac
rhabdomyoma may become easier and more accurate in the clinical
arena.
References
|
1
|
Pruksanusak N, Suntharasaj T, Suwanrath C,
et al: Fetal cardiac rhabdomyoma with hydrops fetalis: report of 2
cases and literature review. J Ultrasound Med. 31:1821–1824.
2012.
|
|
2
|
Atalay S, Aypar E, Uçar T, et al: Fetal
and neonatal cardiac rhabdomyomas: clinical presentation, outcome
and association with tuberous sclerosis complex. Turk J Pediatr.
52:481–487. 2010.
|
|
3
|
Mariano A, Pita A, León R, et al: Primary
cardiac tumors in children: a 16-year experience. Rev Port Cardiol.
28:279–288. 2009.(In English and Portuguese).
|
|
4
|
Ozeren S, Cakiroglu Y, Doger E and
Caliskan E: Sonographic diagnosis of fetal cardiac rhabdomyomas in
two successive pregnancies in a woman with tuberous sclerosis. J
Clin Ultrasound. 40:179–182. 2012.
|
|
5
|
Gamzu R, Achiron R, Hegesh J, et al:
Evaluating the risk of tuberous sclerosis in cases with prenatal
diagnosis of cardiac rhabdomyoma. Prenat Diagn. 22:1044–1047.
2002.
|
|
6
|
Fesslova V, Villa L, Rizzuti T,
Mastrangelo M and Mosca F: Natural history and long-term outcome of
cardiac rhabdomyomas detected prenatally. Prenat Diagn. 24:241–248.
2004.
|
|
7
|
Holley DG, Martin GR, Brenner JI, et al:
Diagnosis and management of fetal cardiac tumors: a multicenter
experience and review of published reports. J Am Coll Cardiol.
26:516–520. 1995.
|
|
8
|
Benyounes N, Fohlen M, Devys JM, et al:
Cardiac rhabdomyomas in tuberous sclerosis patients: a case report
and review of the literature. Arch Cardiovasc Dis. 105:442–445.
2012.
|
|
9
|
Isaacs H Jr: Fetal and neonatal cardiac
tumors. Pediatr Cardiol. 25:252–273. 2004.
|
|
10
|
Zhou QC, Fan P, Peng QH, et al: Prenatal
echocardiographic differential diagnosis of fetal cardiac tumors.
Ultrasound Obstet Gynecol. 23:165–171. 2004.
|
|
11
|
Hou CF, Chao A, Wang CJ, Chao AS and Hsueh
C: Atrial hemangioma: a rare cause of hydrops fetalis and
intrauterine fetal death. Eur J Obstet Gynecol Reprod Biol.
130:271–272. 2007.
|
|
12
|
Chao AS, Chao A, Wang TH, et al: Outcome
of antenatally diagnosed cardiac rhabdomyoma: case series and a
meta-analysis. Ultrasound Obstet Gynecol. 31:289–295. 2008.
|
|
13
|
DeVore GR, Hakim S, Kleinman CS and
Hobbins JC: The in utero diagnosis of an interventricular septal
cardiac rhabdomyoma by means of real-time-directed, M-mode
echocardiography. Am J Obstet Gynecol. 143:967–969. 1982.
|
|
14
|
Chao AS, Chao A, Wang TH, et al: Outcome
of antenatally diagnosed cardiac rhabdomyoma: case series and a
meta-analysis. Ultrasound Obstet Gynecol. 31:289–295. 2008.
|
|
15
|
Hata T, Yan F, Dai SY, Kanenishi K and
Yanagihara T: Real-time 3-dimensional echocardiographic features of
fetal cardiac tumor. J Clin Ultrasound. 35:338–340. 2007.
|
|
16
|
Yagel S, Cohen SM, Rosenak D, et al: Added
value of three-/four-dimensional ultrasound in offline analysis and
diagnosis of congenital heart disease. Ultrasound Obstet Gynecol.
37:432–437. 2011.
|