Introduction
Thyroid tuberculosis (TT) is a rare disease even in
countries with a high prevalence of other forms of tuberculosis
(1). The actual incidence of TT is
difficult to assess, but it has been estimated that 0.1–0.4% of all
newly diagnosed tuberculosis cases involve the thyroid gland
(2–4). Thyroid malignancies, suppurative
infections and hemorrhagic cysts are included in the list of the
differential diagnoses of TT. Consequently, this infectious disease
is often overlooked and patients may suffer from an increased risk
of morbidity and mortality due to delayed diagnosis and treatment
(5–7). The use of ultrasound (US) occurs
extensively in the initial evaluation of thyroid nodules and makes
available the relevant information on the characteristics of
thyroid lesions and the adjacent parenchyma. Few studies have
described the US features of TT to date (8,9). No
systematic data have been provided with regard to the evolution of
US findings during the course of the disease, from the initial
diagnosis until the conclusion of treatment. The present study
reports the dynamic monitoring of the US features of a TT case that
was diagnosed by US-guided core-needle biopsy (CNB) and followed-up
sonographically during the whole course of treatment. Consent was
obtained from the patient.
Case report
A 45-year-old male patient presented to the Hangzhou
Red Cross Hospital (Hangzhou, Zhejiang, China) with a painless
swelling in the left side of the neck that had gradually increased
in size over two weeks. There was no complaint of dysphagia or
dyspnea. The patient did not report any history of fever, coughing
or hemoptysis, but complained of weight loss of 4 kg within the
prior three months. The patient had no past or family history of
tuberculosis. Upon examination, a solid, non-tender, 40×30-mm
ill-defined mass was present in the left lobe of the thyroid. The
cervical lump moved with deglutition, and no enlargement of the
regional lymph nodes was observed. The white cell count in the
peripheral blood was 10.9×109/l (normal range,
3.0–9.0×109/l), the neutrophil level was 45% and the
erythrocyte sedimentation rate (ESR) was 60 mm/h. A thyroid
hormonal profile revealed a euthyroid status. Human
immunodeficiency virus testing was negative and investigations for
infectious or inflammatory conditions were unremarkable. A chest
X-ray revealed no pulmonary abnormalities, but the tuberculin test
(1:10,000) was strongly positive.
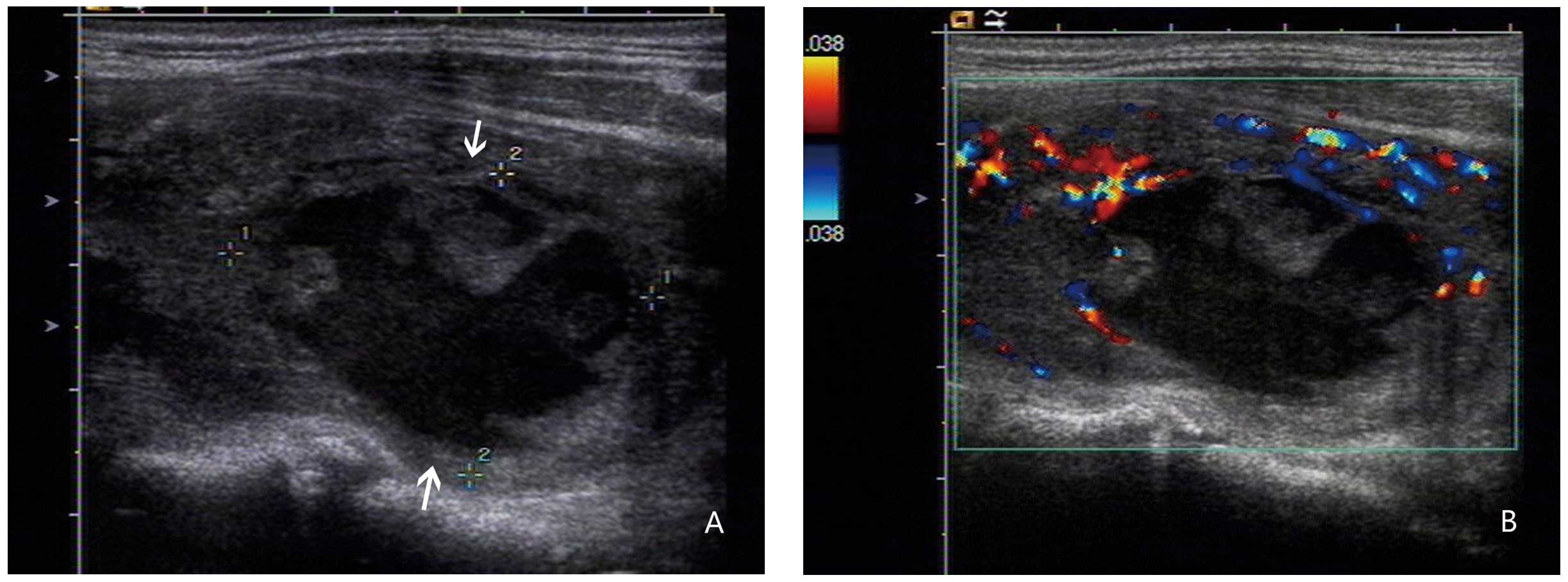
US of the thyroid gland was performed using a
real-time machine equipped with a 9–11 MHz probe (Philips,
Amsterdam, Netherlands). US examination revealed a 34×27×24-mm,
ovoid-shaped mass in the left lobe of the thyroid gland. The
thyroid lesion was inhomogeneously hypoechoic, with ill-defined
margins. An anechoic area with internal hyperechoic spots was
present within the mass (Fig. 1A).
Color Doppler examination revealed punctate or linear flow signals
around the nodule with no intralesional vascularization (Fig. 1B).
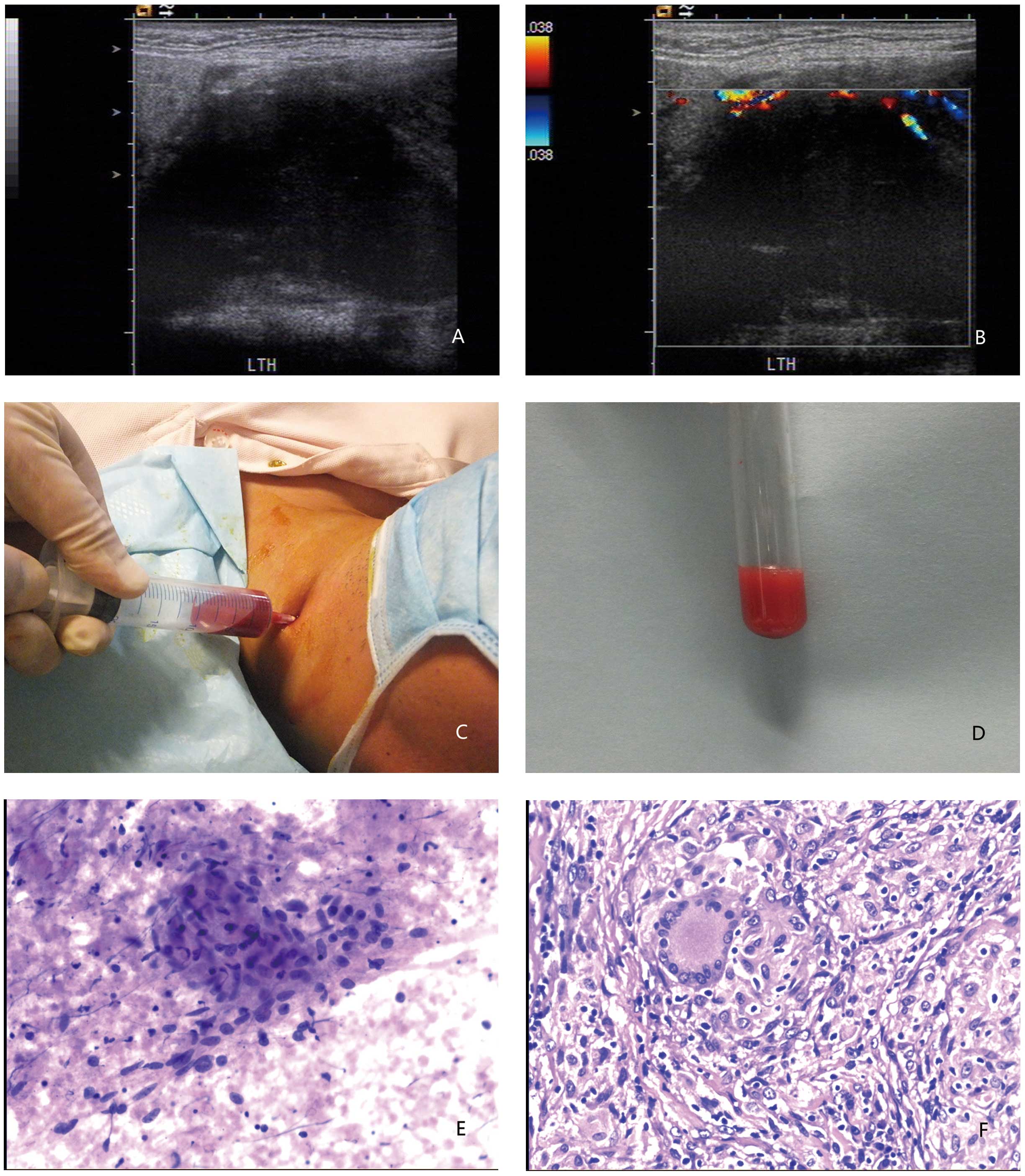
The patient’s general condition worsened three days
after admission. There had been an increase in the size of the
swelling, associated with a 37–38°C low-grade fever. A repeat US
examination demonstrated that the mass in the left lobe of the
gland had increased in volume to 65×35×38 mm. The lesion partially
protruded from the upper pole of the left thyroid lobe (Fig. 2A). Compression with the probe and
positional changes demonstrated the presence of liquid within the
mass. Blood flow signals were observed by color Doppler examination
around, but not inside the lesion (Fig.
2B). A US-guided fine-needle aspiration (FNA) biopsy of the
thyroid mass yielded a thick, caseous and bloody material (Fig. 2C and D). Microscopic examination
revealed the presence of follicular epithelial cells in flaked or
honeycombed formations on a bloody background, together with
clusters of purple-stained colloid and a field of granular caseous
necrosis (Fig. 2E). In order to
obtain a histological diagnosis, a US-guided CNB of the adjacent
solid tissue was performed with a 21-gauge cutting needle.
Histopathological examination revealed that multifocal
granulomatous nodules were distributed in between atrophic thyroid
follicles, chronic inflammatory cell infiltration and fibrous
tissue proliferation (Fig. 2F).
Acid-fast staining on frozen-sections did not indicate the presence
of bacteria. However, the presence of multifocal granulomatous
inflammation associated with caseous necrosis was strongly
suggestive of tuberculous infection.
The patient was administered an oral three-drug
regimen of antituberculous medication (0.3 g isoniazid, 0.6 g
rifampicine and 0.2 g ciprofloxacine, once daily for a total of 3
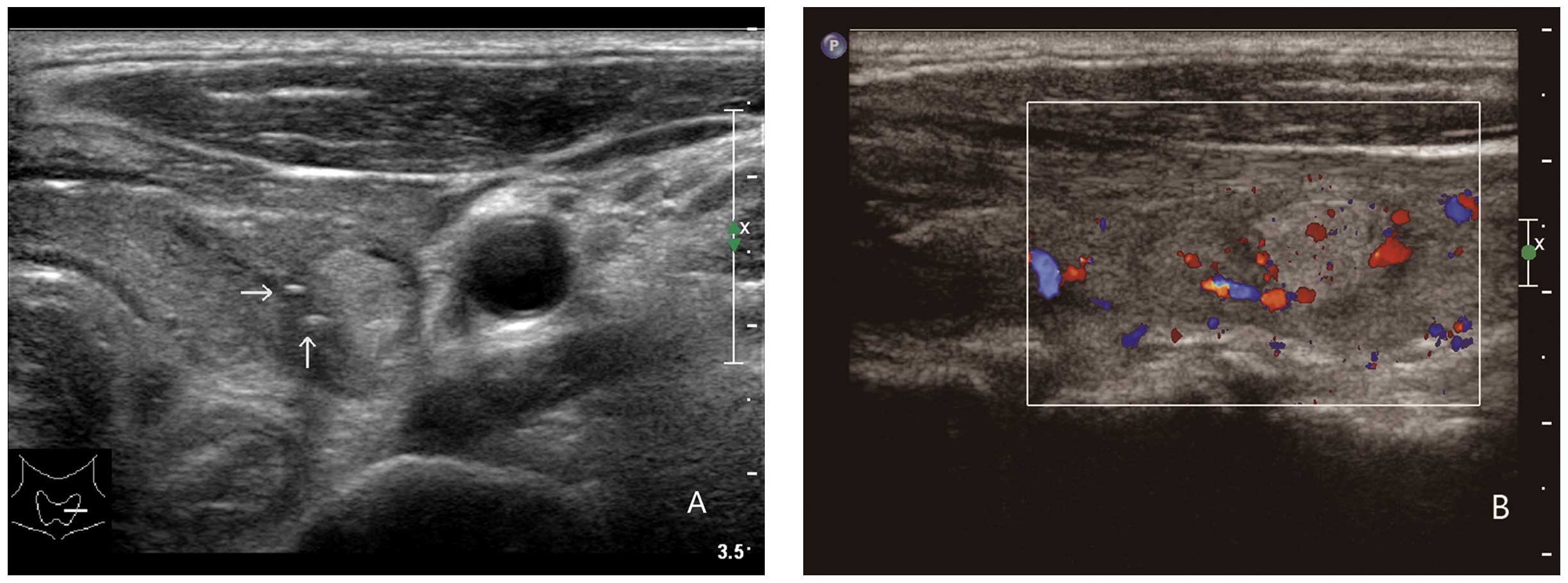
months). Subsequent to three months of treatment, US demonstrated
clinically significant shrinkage of the nodule down to 16×10×12 mm
and the appearance of coarse calcifications inside the lesion. A
repeat US examination was performed six months later without any
marked changes in size, but with progressive loss of the definition
of the nodule limits (Fig. 3). The
patient remains without clinical symptoms at the time of
writing.
Discussion
Tuberculosis affects almost all organs of the human
body, but involvement of the thyroid gland, although initially
reported in 1863, is rare (1).
Resistance to tuberculous infection due to the bactericidal action
of thyroid colloid, the high blood flow and tissue oxygenation, and
the high concentration of iodine within the gland are possible
explanations (10).
The clinical presentation of TT is non-specific and
variable (11,12). TT may be asymptomatic or may present
with an occasionally elusive spectrum of manifestations. Physical
examination may reveal an isolated nodule, as observed in the
present case, a nodular goiter or a cold abscess. Laboratory
examination may also fail to provide a substantial clue for the
exact diagnosis. In the present study, laboratory examination only
noted a slight increase in the white blood cell count and ESR,
which were not specific for TT. Consequently, the diagnosis of TT
is frequently delayed and may represent an incidental finding at
pathological examination. By contrast, an unnecessary thyroidectomy
may occur in cases mimicking a fast-growing thyroid malignancy
(4,13).
US-guided FNA biopsy of the lesion appears to be a
useful tool for the timely and accurate diagnosis of TT (14,15).
In the present case, however, the initial FNA biopsy revealed only
non-diagnostic necrotic material. US-guided CNB of the intra- and
perilesional solid component made the correct diagnosis of TT
possible. Notably, the microbiological evaluation of FNA specimens
for Mycobacterium tuberculosis was negative in the present
case. This finding highlights the pivotal role of US-guided
histopathological examination for a timely diagnosis.
A variable spectrum of US findings from few TT cases
have been sporadically reported in previous studies. Kang et
al (9) presented a case in
which US examination revealed multifocal, heterogeneous, hypoechoic
lesions with ill-defined margins in each lobe of the thyroid. Kang
et al (8) performed US
examinations on two cases, one of which demonstrated an enlarged
right lobe of the gland and a well-defined lesion that was
predominantly anechoic, with internal echoes and irregular margins.
In the other case, a large, heterogeneous, predominantly anechoic
lesion with an irregular wall and few internal echoes in the left
lobe was revealed. All these studies highlight the importance of
using US in arriving at an accurate diagnosis of TT. In the present
case, the initial US examination revealed a heterogeneous,
fluid-filled nodule coexisting with internal bleeding, which was
hardly distinguishable from a colliquated thyroid adenoma. The
repeat US examination revealed progressive changes in the US
findings until the nodule was solid and hyperechoic with
ill-defined margins. Two, tiny, calcified foci were also found
inside the mass, which made this lesion similar to calcified
tubercular goiters. These changes in the US examination may be of
use in monitoring the efficacy of antitubercular treatment and
suggest the importance of dynamic US monitoring for TT
patients.
TT should be considered in the differential
diagnosis of neck masses, particularly in those lesions that
increase rapidly in size and resemble thyroid malignancy. US
examination and US-guided CNB are important techniques for a timely
and accurate diagnosis of thyroid malignancies. These rapid, safe
and inexpensive diagnostic procedures can prevent an unnecessary
thyroidectomy and make an appropriate antitubercular therapy
possible.
References
|
1
|
Khan EM, Haque I, Pandey R, Mishra SK and
Sharma AK: Tuberculosis of the thyroid gland: a clinicopathological
profile of four cases and review of the literature. Aust N Z J
Surg. 63:807–810. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Simkus A: Thyroid tuberculosis. Medicina
(Kaunas). 40:201–204. 2004.
|
|
3
|
Majid U and Islam N: Thyroid tuberculosis:
a case series and a review of the literature. J Thyroid Res.
2011:3598642011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Al-Mulhim AA, Zakaria HM, Abdel Hadi MS,
et al: Thyroid tuberculosis mimicking carcinoma: report of two
cases. Surg Today. 32:1064–1067. 2002. View Article : Google Scholar
|
|
5
|
Bulbuloglu E, Ciralik H, Okur E, et al:
Tuberculosis of the thyroid gland: review of the literature. World
J Surg. 30:149–155. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ozekinci S, Mizrak B, Saruhan G and
Senturk S: Histopathologic diagnosis of thyroid tuberculosis.
Thyroid. 19:983–986. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
El Malki HO, Mohsine R, Benkhraba K, et
al: Thyroid tuberculosis: diagnosis and treatment. Chemotherapy.
52:46–49. 2006. View Article : Google Scholar
|
|
8
|
Kang M, Ojili V, Khandelwal N and Bhansali
A: Tuberculous abscess of the thyroid gland: a report of two cases.
J Clin Ultrasound. 34:254–257. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kang BC, Lee SW, Shim SS, et al: US and CT
findings of tuberculosis of the thyroid: three case reports. Clin
Imaging. 24:283–286. 2000. View Article : Google Scholar
|
|
10
|
Luiz HV, Pereira BD, Silva TN, et al:
Thyroid tuberculosis with abnormal thyroid function - case report
and review of the literature. Endocr Pract. 19:e44–e49. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Akbulut S, Gomceli I, Cakabay B, et al:
Clinical presentation of primary thyroid tuberculosis. Thyroid.
20:231–232. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Terzidis K, Tourli P, Kiapekou E and
Alevizaki M: Thyroid tuberculosis. Hormones (Athens). 6:75–79.
2007.
|
|
13
|
Silva BP, Amorim EG, Pavin EJ, et al:
Primary thyroid tuberculosis: a rare etiology of hypothyroidism and
anterior cervical mass mimicking carcinoma. Arq Bras Endocrinol
Metabol. 53:475–478. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Das DK, Pant CS, Chachra KL and Gupta AK:
Fine needle aspiration cytology diagnosis of tuberculous
thyroiditis. A report of eight cases. Acta Cytol. 36:517–522.
1992.PubMed/NCBI
|
|
15
|
Mondal A and Patra DK: Efficacy of fine
needle aspiration cytology in the diagnosis of tuberculosis of the
thyroid gland: a study of 18 cases. J Laryngol Otol. 109:36–38.
1995. View Article : Google Scholar : PubMed/NCBI
|