Introduction
Lung cancer is the most common type of malignant
tumour worldwide, and the morbidity and mortality rates for lung
cancer are the highest among malignant tumours (1,2). Lung
cancer may remain asymptomatic and lacks common early symptoms.
Therefore, it is typically discovered late and diagnosed at an
advanced stage; early diagnosis accounts for just 15–25% of lung
cancer cases (3). Despite the
application of various treatment strategies, the 5-year survival
rate for lung cancer patients remains low at <15% (4). In the present study, a retrospective
analysis was performed on clinical data from 1,168 lung cancer
patients who had received their initial diagnosis and treatment at
the Tumor Hospital of Shandong Province (Jinan, China) between
January 1 2009 and December 31 2009. The current retrospective
analysis reviewed the initial clinical symptoms upon diagnosis,
duration of patient delay in presenting to a doctor, lung cancer
stage, treatment strategy and prognosis. The aim was to identify
factors which influence survival time.
Patients and methods
Inclusion criteria
Patients were included on the basis that primary
pulmonary lesions were histopathologically or cytologically
diagnosed, and the extent and clinical stage of the cancer were
determined. Cancer staging was achieved by performing comprehensive
physical examinations and enhanced chest computed tomography (CT)
scans. Occasionally, systemic radionuclide bone imaging was
performed and, if foci of abnormal radiotracer uptake were
identified, additional examinations, such as magnetic resonance
imaging (MRI), CT or X-ray imaging were performed, including brain
MRI or CT. In addition, B-mode ultrasound scanning of abdominal
organs and the retroperitoneum were occasionally conducted and, if
tissue abnormalities were detected, enhanced CT scans of the
abdomen were performed. In specific cases, a whole-body positron
emission tomography-computed tomography examination was conducted
(4). All initial diagnoses and
treatments occurred at the Tumor Hospital of Shandong Province;
patients did not receive treatment from other hospitals (5). Readmitted medical cases were excluded
from the present study.
General clinical data
A total of 1,238 lung cancer patients were admitted
to the Tumor Hospital of Shandong Province between January 1, 2009
and December 31, 2009. Of these 1,238 patients, 70 patients did not
receive a histopathological or cytological diagnosis and had
incomplete clinical data, and thus were excluded from the present
study. There were 588 male smokers (71%) and 33 female smokers
(9.7%) included in the study. The clinical data of the remaining
1,168 patients is indicated in Table
I.
 | Table IClinical data of 1,168 patients. |
Table I
Clinical data of 1,168 patients.
| Patients |
|---|
|
|
|---|
| Parameter | n | % |
|---|
| Gender |
| Male | 828 | 78.9 |
| Female | 340 | 29.1 |
| Age, years |
| Mean (range) | 60.2 (19–88) |
| <40 | 49 | 4.2 |
| 40–49 | 158 | 13.5 |
| 50–59 | 342 | 29.3 |
| 60–69 | 350 | 30.0 |
| 70–79 | 235 | 20.1 |
| ≥80 | 34 | 2.9 |
| Smoking history |
| Smoker | 621 | 53.2 |
| Male | 588 | 50.3 |
| Female | 33 | 2.8 |
| Non-smoker | 547 | 46.8 |
| Male | 240 | 20.5 |
| Female | 307 | 26.3 |
| Clinical
symptoms |
| Cough | 87 | 7.4 |
| Chest pain | 74 | 6.3 |
| Shortness of
breath | 85 | 7.3 |
| Cough,
expectoration | 273 | 23.4 |
| Cough, blood-tinged
sputum | 178 | 15.2 |
| Cough,
expectoration, chest tightness | 166 | 14.2 |
| Cough,
expectoration, chest pain | 46 | 3.9 |
| Cough,
expectoration, shortness of breath | 64 | 5.5 |
| Cough,
expectoration, fever | 8 | 0.7 |
| Cough,
expectoration, symptoms occurring outside of the lung | 37 | 3.2 |
| Symptoms occurring
outside of the lung | 102 | 8.7 |
| No symptoms | 48 | 4.1 |
| Duration of patient
delay, months |
| Mean | 2.29 |
| Medium | 2.0 |
| Range | 0.1–24.0 |
| Histo- or
cyto-pathological type |
| Adenocarcinoma | 621 | 53.2 |
| Squamous cell
carcinoma | 337 | 28.8 |
| Small cell
carcinoma | 143 | 12.2 |
| Adenosquamous
carcinoma | 18 | 1.5 |
| Large cell
carcinoma | 12 | 1.0 |
| Atypical
carcinoid | 5 | 0.4 |
| Carcinoid | 3 | 0.2 |
| Histo- or
cyto-pathological type |
| Sarcomatoid
carcinoma | 3 | 0.2 |
| Neuroendocrine
carcinoma | 3 | 0.2 |
| Lymphoma | 2 | 0.2 |
| Spindle cell
carcinoma | 2 | 0.2 |
| Other unclassified
cancer | 19 | 1.6 |
| T stage |
| T1 | 91 | 7.8 |
| T2 | 582 | 49.8 |
| T3 | 250 | 21.4 |
| T4 | 245 | 21.0 |
| N stage |
| N0 | 125 | 10.7 |
| N1 | 119 | 10.2 |
| N2 | 561 | 48.0 |
| N3 | 363 | 31.1 |
| M stage |
| M0 | 629 | 53.8 |
| M1 | 539 | 46.1 |
| Clinical TNM
stage |
| I | 46 | 3.9 |
| II | 85 | 7.3 |
| III | 498 | 42.6 |
| IV | 539 | 46.1 |
Treatment strategies
The predominant treatment strategies received by the
lung cancer patients included surgery, radiation therapy,
chemotherapy, targeted therapy and comprehensive treatment
involving a combination of therapies. However, certain patients
refused treatment. The types of treatment were as follows:
Chemotherapy alone, 164 cases (14.0%); radiation therapy alone, 28
cases (2.4%); surgery alone, 24 cases (2.1%); radiation therapy and
chemotherapy, 593 cases (50.8%); radiochemotherapy and targeted
therapy, 30 cases (2.6%); chemotherapy and targeted therapy, 29
cases (2.5%); radiation therapy and targeted therapy, seven cases
(0.6%); surgery and chemotherapy, 116 cases (9.9%); surgery and
radiochemotherapy, 58 cases (4.9%); surgery, radiochemotherapy and
targeted therapy, two cases (0.2%); targeted therapy alone, eight
cases (0.7%); and no treatment, 109 cases (9.3%).
Follow-up period
As of April 30, 2012, 89 of the 1,168 patients were
lost to follow-up, resulting in a follow-up rate of 92.4%. The
follow-up period ranged from 1 to 41 months, and the mean and
medium follow-up periods were 20.8 and 21 months, respectively. The
follow-up of surviving patients is on-going.
Statistical analysis
Statistical analysis was performed using SPSS
software (version 17; SPSS, Inc., Chicago, IL, USA). Student’s
t-test was utilised to compare the means of two samples and the
χ2 test was used for all other comparisons. Univariate
survival analysis was conducted using Kaplan-Meier analysis and the
log-rank test, and the significance level was α=0.05.
Results
Patient clinical data
The clinical features of 828 and 340 male and female
lung cancer patients, respectively, were compared, including age
and the duration of patient delay in presenting to a doctor
(Table I). The maximum and minimum
ages of the male patients were 88 and 21 years, respectively; and
the maximum and minimum ages of the female patients were 86 and 19
years. Furthermore, the median ages of the male and female patients
were 61 and 59 years, respectively; and the mean ± standard
deviation age of the male and female patients was 60.6±10.8 and
59.1±12.3 years, respectively. No significant difference was
identified between the age of the male and female patients
(t=1.107; P=0.271).
The maximum and minimum duration of patient delay in
male and female patients was 24.0 and 0.10 months. Additionally,
the median duration of patient delay in male and female patients
was 2 months for both, and the mean duration of patient delay in
male and female patients was 2.25±2.44 and 2.38±2.78 months,
respectively. No significant difference was identified between the
duration of male and female patient delay (t=0.752; P=0.816).
The predominant histopathological types of lung
cancer were adenocarcinoma (n=621), squamous cell carcinoma (n=337)
and small cell carcinoma (n=143). In male patients, the number of
cases of adenocarcinoma, squamous cell carcinoma and small cell
carcinoma were 376, 298 and 110, respectively; and in female
patients, these were 245, 39 and 33, respectively. A significant
difference was identified between the histopathological types of
lung cancer in male and female patients (χ2= 8.671;
P<0.001).
Patient survival rates
As of April 30, 2012, 208 of the 1,168 lung cancer
patients had received surgery alone, surgery plus radiochemotherapy
and/or targeted therapy, accounting for 17.1% of the patients in
the present study. The 1-, 2- and 3-year survival rates for these
patients were 80.4, 44.9 and 15.8%, respectively. A comparison of
the survival curves for the male and female patients in the present
study indicated no significant differences.
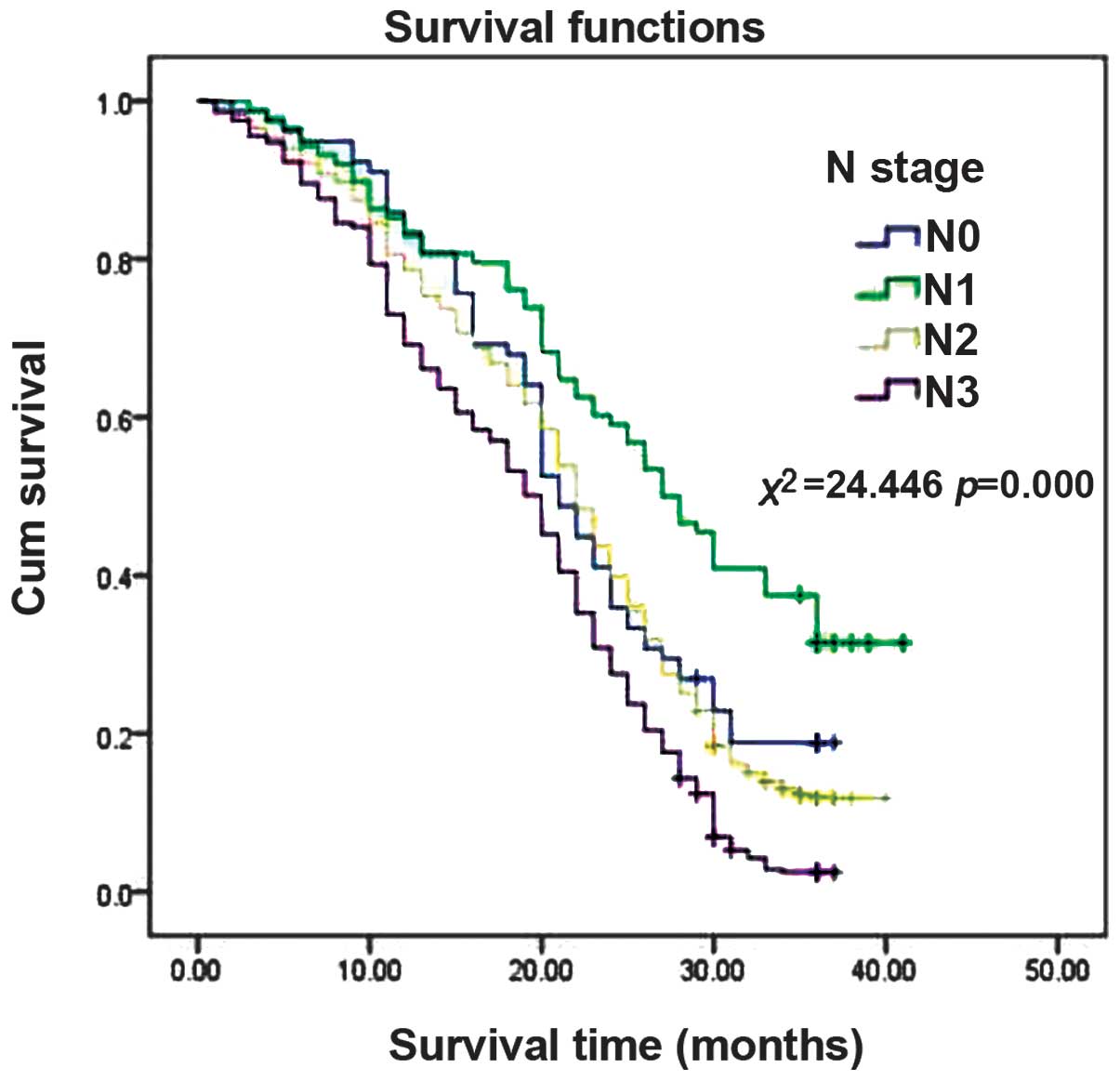
Association between TNM staging and
patient survival
The effect of the tumour extent (T), lymph node
involvement (N) and clinical stage of the lung cancer on patient
survival are demonstrated in Figs.
1, 2 and 3, respectively. The results indicated that
more advanced T, N and clinical stages of lung cancer were
associated with shorter survival times.
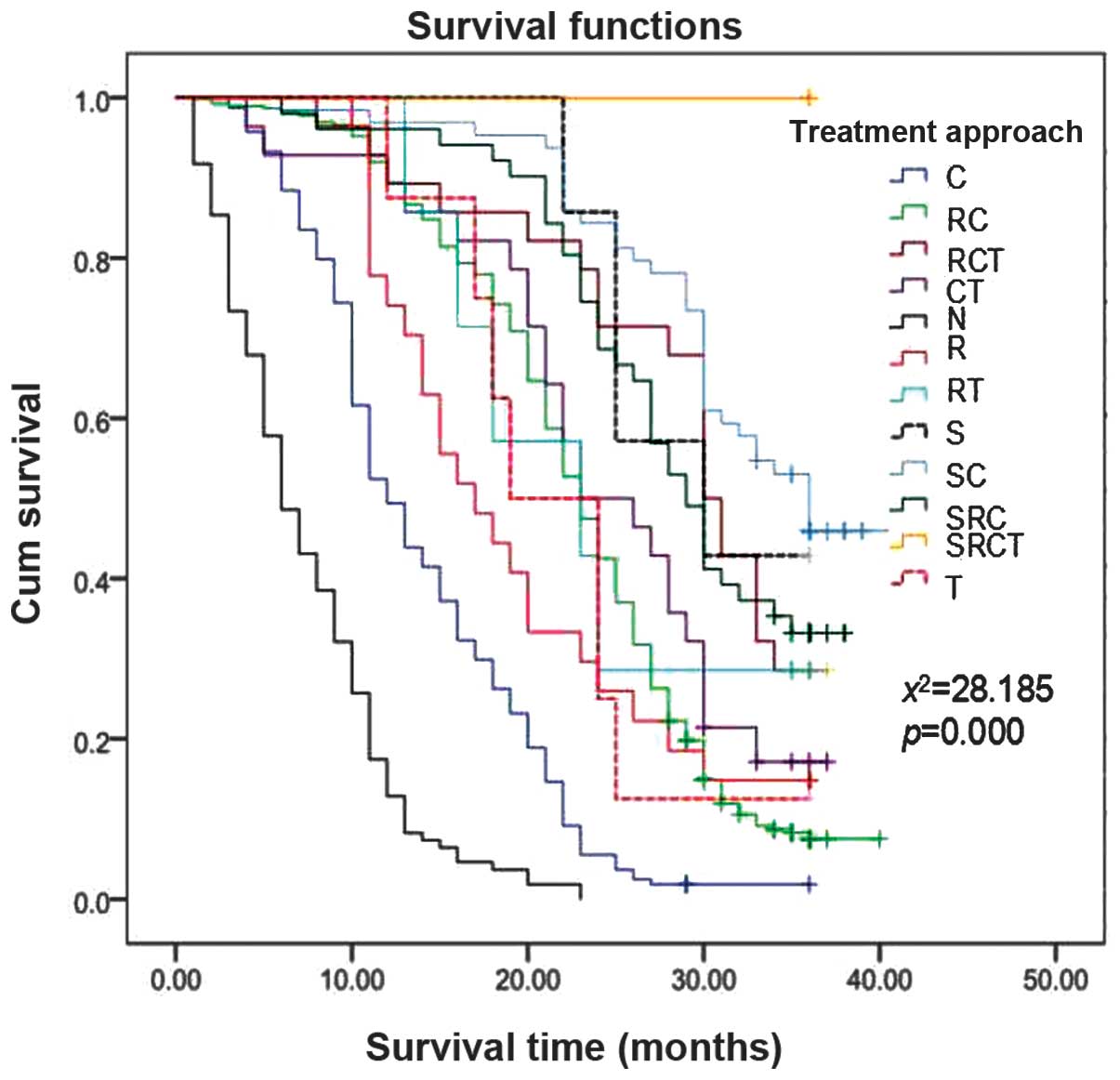
Association between treatment strategy
and patient survival
The effect of the treatment strategy on survival is
demonstrated in Fig. 4. The
survival curves of all of the treatment strategies demonstrated a
gradual decline. Furthermore, these results indicated that a
combination of surgery and chemotherapy, surgery alone, and a
combination of surgery and radiochemotherapy achieved therapeutic
effects. By contrast, the lung cancer patients who received no
treatment or chemotherapy alone demonstrated a poor prognosis.
Multivariate Cox regression analysis
The results of the multivariate Cox regression
analysis are summarised in Table
II. Patient age, T stage, N stage, overall clinical stage and
treatment strategy were independent risk factors for survival.
 | Table IIMultivariate Cox regression
analysis. |
Table II
Multivariate Cox regression
analysis.
| Factor | Regression
coefficient (β) | Wald value | P-value | Relative risk |
|---|
| Age | −0.018 | 30.666 | 0.000 | 1.019 |
| T stage | −0.140 | 15.427 | 0.000 | 1.150 |
| N stage | −0.206 | 25.120 | 0.000 | 1.228 |
| Clinical stage | −0.741 | 268.006 | 0.000 | 2.098 |
| Treatment
strategy | 0.398 | 32.771 | 0.000 | 1.367 |
Discussion
The morbidity and mortality rates associated with
lung cancer are the highest among malignant tumours. As medical
technology advances, the diagnosis rate of lung cancer is expected
to gradually rise; however, an increase in the early diagnosis rate
has yet to be observed (1,2). Among the 1,168 lung cancer patients
analysed in the present study, the percentages of patients
exhibiting stage I, II, III and IV lung cancer were 3.9, 7.3, 42.6
and 46.1%, respectively. The percentage of patients exhibiting
early-stage (stages I and II) lung cancer was relatively low,
accounting for only 11.2% of the total patients analysed, whereas a
significantly higher percentage of patients exhibited advanced lung
cancer (stage IV; 46.1%). The percentages of stage IIIA and IIIB
lung cancer patients were 23.0 and 19.6%, respectively. Under
normal circumstances, surgery is not the preferred treatment
strategy for patients with stage IIIB lung cancer (6). The total percentage of stage IIIB or
IV lung cancer patients was 65.7%, indicating that the majority of
patients were in the late stages of lung cancer at the time of the
initial diagnosis and, thus, had missed the opportunity to receive
surgery. It is possible that the majority of patients exhibiting
early-stage lung cancer were diagnosed and treated locally, at
city- and county-level hospitals, and only the patients with
advanced lung cancers or complications were referred to the Tumor
Hospital of Shandong Province. This may explain why the majority of
patients in the current study presented in the late stages of lung
cancer.
In addition, the 1,168 lung cancer patients were
analysed from a gender perspective. There were 828 male and 340
female patients, resulting in a male to female ratio of 2.4:1. The
incidence of lung cancer in male patients was significantly higher
compared with that in females; however, no gender differences were
identified with regard to the patient age at lung cancer onset or
the duration of patient delay. The higher incidence of lung cancer
in males may be a result of the higher prevalence of smoking among
males compared with females. In the present study, a total of 588
male smokers (71%) and 33 female smokers (9.7%) were included.
Smoking is a major cause of lung cancer, and numerous studies have
reported a significantly worse prognosis among patients with a
history of smoking compared with non-smokers (7,8).
Furthermore, Chen et al (9)
reported that smoking is positively associated with lung tumour
size at diagnosis (TSD) in a dose-dependent manner. The study
identified that TSD was largest in current smokers, smallest in
never-smokers and intermediate in former smokers. Multivariate
linear regression analysis determined that smoking status (never
vs. former vs. current), histopathological tumour type
(adenocarcinoma vs. squamous cell carcinoma) and gender (male vs.
female) were significant predictors of TSD; therefore, gender may
be a predictor of TSD due to differences in smoking duration and
intensity between males and females.
In the present study, the predominant symptoms of
lung cancer included cough, expectoration, blood-tinged sputum,
chest pain, chest tightness and other symptoms occurring outside of
the lung. The duration of patient delay ranged from 0.1 to 24.0
months, the median delay period was 2 months, and the mean delay
period was 2.29 months; thus, the duration of patient delay was
long. The age of onset of lung cancer ranged from 19 to 88 years,
and the mean and median ages of cancer onset were 60.2 and 60
years, respectively. Furthermore, the overall cancer incidence
rates gradually increased with age, and the peak incidence of lung
cancer was among patients aged between 50 and 70 years. Patients
<50 years of age exhibited an incidence rate of 17.7%. The
results of this study similar to those of Miron et al (10), which demonstrated that NSCLC
occurence was highest in the 56–71 year old age group and the most
common histological type was adenocarcinoma. If any of the
abovementioned symptoms are present, patients should visit a health
care facility promptly and be examined by chest radiograph or
low-dose CT scan to obtain a clear diagnosis as quickly as
possible. In addition, it has also been reported that lung cancer
screening by low-dose CT is most beneficial to asymptomatic
patients ≥40 years of age. In a previous study, low-dose CT scans
of 1,151 asymptomatic patients >40 years of age determined a
lung cancer incidence rate of 0.51% (8/1551 patients). In addition,
the incidence rates were significantly higher in high-risk patients
(1.21%; 7/577 patients) and heavy smokers (2.01%; 6/298 patients)
(11). The present study
demonstrated that the incidence of cancer was significantly
increased in individuals >50 years of age. Therefore, routine
check-ups are recommended for patients who are ≥50 years of age, at
least once per year, to promote the early detection, diagnosis and
treatment of lung cancer.
In the current study, the predominant
histopathological types of lung cancer were adenocarcinoma,
squamous cell carcinoma and small cell carcinoma, which accounted
for 53.2, 28.8 and 12.2% of total lung cancers, respectively. The
incidence of different histopathological types of lung cancer
varied between males and females: In females, adenocarcinoma,
squamous cell carcinoma and small cell carcinoma occurred at a rate
of 72.1, 11.5 and 9.7%, respectively; however, in males, these
incidence rates were 45.4, 36.0 and 13.3%, respectively.
Adenocarcinoma was the most common type of lung cancer among males
and females in the present study, and the incidence rate of lung
adenocarcinoma is rising in numerous countries, particularly among
Asian females (12). Notably, the
number of mortalities caused by lung adenocarcinoma account for 50%
of the total number of mortalities caused by lung cancer-related
diseases (13–15). However, Yao et al (16) reported that, in Western China, the
incidence rates of lung squamous cell carcinoma and small cell
carcinoma were increasing, whereas the incidence rate of lung
adenocarcinoma was decreasing. In the United States, non-small cell
lung cancer (NSCLC) accounts for almost 85% of all cases of lung
cancer (17). Furthermore,
discrepancies between studies may be due to the presence of
regional differences in the histopathological types of lung cancer.
In clinical practice, different treatment strategies should be
formulated for different histopathological types of lung
cancer.
Treatment strategies for lung cancer include
surgery, chemotherapy, radiation therapy and targeted therapy, and
different treatment strategies have different effects on patient
survival. The present analysis of the association between treatment
strategy and survival demonstrated that 208/1,168 (17.1%) lung
cancer patients analysed were suitable candidates for surgery. The
patients who were treated with a combination of surgery and
chemotherapy, surgery alone or a combination of surgery and
radiochemotherapy demonstrated an improved prognosis. These results
indicate that survival is associated with the stage of the cancer,
as surgery was generally a more feasible therapeutic option for
patients with early-stage disease. The patients who received no
treatment demonstrated the worst prognosis. In addition, patients
who received chemotherapy or radiotherapy alone demonstrated a poor
prognosis. Therefore, treatment strategies are typically associated
with the general condition of the patient and the stage of the
cancer. Lung cancer patients who were in poor general condition,
exhibited severe chronic complications or were in the late stages
of the disease received only palliative treatment or no treatment
and, thus, had a poor prognosis. By contrast, patients treated with
targeted therapy demonstrated an improved prognosis compared with
those who received no treatment or chemotherapy alone. According to
the literature, patients with epidermal growth factor receptor
mutation-positive lung cancer tend to have a good prognosis
following treatment with targeted therapy (9,18).
However, the agents used in targeted therapy are expensive and
unaffordable for the majority of patients; therefore, this
treatment strategy is chosen by relatively few patients. In
addition, the majority of patients who do select targeted therapy
are in the late stages of the disease and have no other feasible
therapeutic options available to them.
Lung cancer is a debilitating disease that results
in as many mortalities as the next four most common malignancies
combined, and is the leading cause of cancer-related mortality
globally (19,20). The high mortality rates of NSCLC
patients may be due to the fact that the disease usually presents
in an advanced stage (21). In
metastatic NSCLC patients, overall survival (OS) is improved by the
addition of adjuvant chemotherapy treatment to best supportive
care, as an initial therapy and as a therapy following relapse
(22–25). Furthermore, modern chemotherapeutic
approaches may be associated with positive effects on the survival
of good and poor performance status (PS) patients (26).
The OS for lung cancer patients is poor (4,27). A
total of 75% of lung cancer patients present with incurable
advanced local or metastatic disease (28). In the present study, the 1-, 2-and
3-year survival rates were 80.4, 44.9 and 15.8%, respectively. Less
than 50% of the lung cancer patients survived >2 years in the
research. The main reason is late by stages. In the present study,
the survival time of lung cancer patients was associated with the
clinical stage of the cancer (Fig.
3). The present analysis of tumour, node, metastasis (TNM)
staging and survival demonstrated that more advanced T and N stages
were significantly associated with shorter survival times.
Furthermore, a correlation was revealed between the overall TNM
stage and the survival rate, whereas no differences were identified
in the OS between males and females. Multivariate Cox regression
analysis demonstrated that patient age, T stage, N stage, overall
clinical stage and treatment strategy were independent risk factors
for survival. In addition, patient age, T stage, N stage and
overall clinical stage were negatively correlated with the survival
time of the patients, whereas treatment strategy was positively
correlated with prognosis. Therefore, effective treatment may
improve the OS of lung cancer patients (28,29).
In conclusion, lung cancer patients typically
exhibit a long duration of patient delay. The majority of patients
suffer from late-stage lung cancer at the time of diagnosis,
therefore, the prognosis is poor. Annual, low-dose chest CT
examination is recommended for high-risk patients to enable early
detection and treatment, thus improving patient prognosis.
Acknowledgements
The authors would like to thank the Natural Science
Foundation of Shandong Province (grant no. ZR2009CM120).
References
|
1
|
Scheff RJ and Schneider BJ: Non-small-cell
lung cancer: treatment of late stage disease: chemotherapeutics and
new frontiers. Semin Intervent Radiol. 30:191–198. 2013. View Article : Google Scholar :
|
|
2
|
Humphrey LL, Deffebach M, Pappas M,
Baumann C, Artis K, Mitchell JP, Zakher B, Fu R and Slatore CG:
Screening for lung cancer with low-dose computed tomography: a
systematic review to update the US Preventive services task force
recommendation. Ann Intern Med. 159:411–420. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Becker N, Motsch E, Gross ML, et al:
Randomized study on early detection of lung cancer with MSCT in
Germany: study design and results of the first screening round. J
Cancer Res Clin Oncol. 138:1475–1486. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Varela G and Thomas PA: Surgical
management of advanced non-small cell lung cancer. J Thorac Dis.
6(Suppl 2): S217–S223. 2014.PubMed/NCBI
|
|
6
|
Wrona A and Jassem J: The new TNM
classification in lung cancer. Pneumonol Alergol Pol. 78:407–417.
2010.(In Polish).
|
|
7
|
Ferketich AK, Niland JC, Mamet R, et al:
Smoking status and survival in the national comprehensive cancer
network non-small cell lung cancer cohort. Cancer. 119:847–853.
2013. View Article : Google Scholar
|
|
8
|
Tabutin M, Couraud S, Guibert B, et al:
Completion pneumonectomy in patients with cancer: postoperative
survival and mortality factors. J Thorac Oncol. 7:1556–1562. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen X, Gorlov P, Merriman KW, et al:
Association of smoking with tumor size at diagnosis in non-small
cell lung cancer. Lung Cancer. 74:378–383. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Miron L, Bosanceanu M, Filimon R and
Petrariu FD: Clinical-epidemiological study on advanced non-small
cell lung cancer. Rev Med Chir Soc Med Nat Iasi. 118:492–496.
2014.PubMed/NCBI
|
|
11
|
Lei Y, Chen BJ, Zeng L and Li WM:
Application value of low-dose computed tomography for the screening
of lung cancer in high-risk group. Sichuan Da Xue Xue Bao Yi Xue
Ban. 43:584–587. 2012.(In Chinese). PubMed/NCBI
|
|
12
|
Wolf AS: Resection for subcentimeter
non-small cell lung cancer: outcomes for a Chinese population with
70% adenocarcinoma. J Surg Oncol. 110:225–226. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kadara H, Kabbout M and Wistuba II:
Pulmonary adenocarcinoma: a renewed entity in 2011. Respirology.
17:50–65. 2012. View Article : Google Scholar
|
|
14
|
Herbst RS, Heymach JV and Lippman SM: Lung
cancer. N Engl J Med. 359:1367–1380. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gazdar AF and Thun MJ: Lung cancer, smoke
exposure, and sex. J Clin Oncol. 25:469–471. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yao X, Liu L, Zhang H, et al: Comparative
analysis of clinical features of lung cancer in west China hospital
in 2000 and 2010. Zhongguo Fei Ai Za Zhi. 15:355–360. 2012.(In
Chinese). PubMed/NCBI
|
|
17
|
Behera M, Owonikoko TK, Chen Z, et al:
Single agent maintenance therapy for advanced stage non-small cell
lung cancer: a meta-analysis. Lung Cancer. 77:331–338. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim YT, Seong YW, Jung YJ, et al: The
presence of mutations in epidermal growth factor receptor gene is
not a prognostic factor for long-term outcome after surgical
resection of non-small-cell lung cancer. J Thorac Oncol. 8:171–178.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jemal A, Center MM, DeSantis C and Ward
EM: Global patterns of cancer incidence and mortality rates and
trends. Cancer Epidemiol Biomarkers Prev. 19:1893–1907. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2012. CA Cancer J Clin. 62:10–29. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
National Comprehensive Cancer Network.
NCCN Clinical Practice Guidelines in Oncology™. Non-Small Cell Lung
Cancer. 2:2012, http://www.tri-kobe.org/nccn/guideline/lung/english/non_small.pdf.
Accessed November 28, 2011
|
|
22
|
Non-Small Cell Lung Cancer Collaborative
Group. Chemotherapy and supportive care versus supportive care
alone for advanced non-small cell lung cancer. Cochrane Database
Syst Rev. CD0073092010.PubMed/NCBI
|
|
23
|
Shepherd FA, Dancey J, Ramlau R, et al:
Prospective randomized trial of docetaxel versus best supportive
care in patients with non-small-cell lung cancer previously treated
with platinum-based chemotherapy. J Clin Oncol. 18:2095–2103.
2000.PubMed/NCBI
|
|
24
|
Souquet PJ, Chauvin F, Boissel JP, et al:
Polychemotherapy in advanced non small cell lung cancer: a
meta-analysis. Lancet. 342:19–21. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hatzidaki D, Agelaki S, Mavroudis D, et
al: A retrospective analysis of second-line chemotherapy or best
supportive care in patients with advanced-stage non-small-cell lung
cancer. Clin Lung Cancer. 8:49–55. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Salloum RG, Smith TJ, Jensen GA and Lafata
JE: Survival among non-small cell lung cancer patients with poor
performance status after first line chemotherapy. Lung Cancer.
77:545–549. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Horeweg N and de Koning H: The importance
of screening for lung cancer. Expert Rev Respir Med. 8:597–614.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jett JR: Current treatment of unresectable
lung cancer. Mayo Clin Proc. 68:603–611. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen VW, Ruiz BA, Hsieh MC, Wu XC, Ries LA
and Lewis DR: Analysis of stage and clinical/prognostic factors for
lung cancer from SEER registries: AJCC staging and collaborative
stage data collection system. Cancer. 120(Suppl 23): 3781–3792.
2014. View Article : Google Scholar : PubMed/NCBI
|