Introduction
Myositis ossificans (MO) is a disease where the
formation of heterotropic bone occurs within a muscle or other type
of soft tissue (1). MO is
classified into two groups, MO progressiva (MOP) and post-traumatic
MO (PTMO) (2). MOP is an autosomal
dominant disease observed within families in which multiple
heterotopic ossifications develop systemically in various muscles,
fascia, tendons and ligaments of the body (2,3). PTMO
is characterized by heterotopic bone formation within muscle tissue
as a result of a single or repetitive injury (2,4). PTMO
is frequently reported in the orthopedic literature and is
prevalent in the quadriceps femoris and brachialis anticus, where
there is high risk for injury. However, MO is rare in the
masticatory muscles. Only 20 cases of MO in the masticatory muscles
were identified during a review of the literature (since 2001),
which was conducted in the present study; 16 cases were associated
with an evident traumatic cause and were diagnosed definitively as
PTMO.
In the present study, a rare case of MO in the
medial and lateral pterygoid muscles that was caused by odontogenic
infection is presented, which was diagnosed as post-infectious MO
(PIMO). To the best of our knowledge, this is the first case of
PIMO in multiple masticatory muscles to be reported in the English
literature. Written informed consent was obtained from the
patient.
Case report
In January 2010, a 42-year-old female was referred
to the Department of Oral and Maxillofacial Surgery, Ninth People’s
Hospital (Shanghai, China) with a complaint of the progressive,
painless limitation of mouth opening for three years. The patient
had no history of evident trauma, however, had experienced pain in
the right upper jaw for approximately three years, for which the
patient had not received any endodontic or periodontal treatment.
In addition, the patient had experienced weakness when biting and
chewing, which had endured for more than two years. The patient was
administered with non-steroidal anti-inflammatory agents by The
First Hospital of Jiaxing (Jiaxing, China), however, no clinical
improvement was observed.
Physical examination revealed that the patient was
well-nourished and demonstrated no evidence of developmental
abnormalities. No facial asymmetry was apparent and the maximal
incisal opening at presentation was 2 mm. Despite the limited range
of motion, the patient reported no associated pain or changes in
the occlusion. On palpation the masseter and temporalis muscles
were normal. The lymph nodes (submandibular and deep cervical) were
nonpalpable and nontender. Intraorally, the right maxillary third
molar residual root and missing mandibular central incisors were
examined. The patient’s dental hygiene was poor, however, the oral
mucosa and tongue appeared to be healthy.
The patient’s general medical status was normal and
the laboratory tests, including serum calcium (2.23 mmol/l; normal
range, 2.08–2.65 mmol/l) and phosphorus levels (1.46 mmol/l; normal
range, 0.78–1.65 mmol/l), were within the normal limits. A
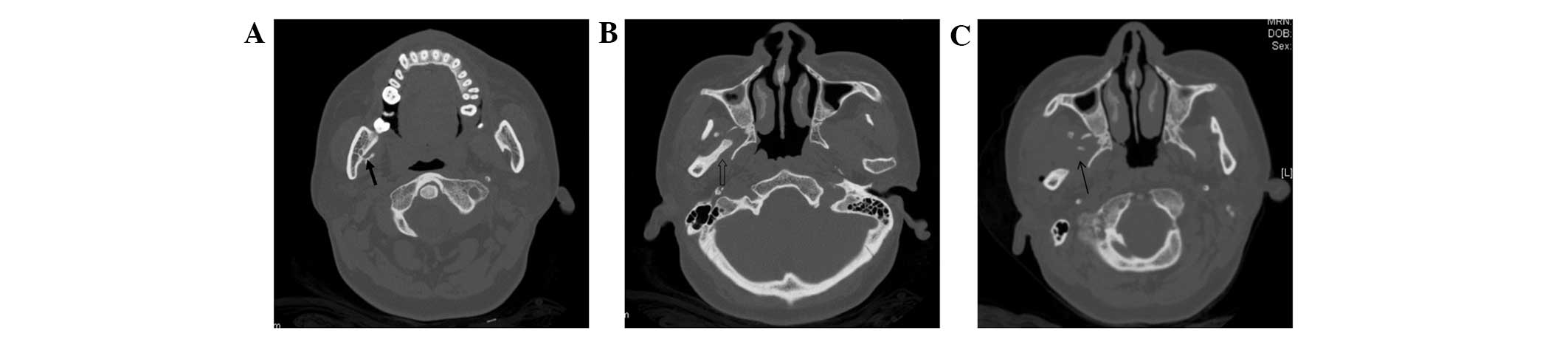
panoramic radiograph (Fig. 1)
showed chronic periapical lesions of the right maxillary third
molar residual root (Fig. 1A).
Computed tomography (CT) scans (Fig.
2) revealed heterotopic bone formation in the right lateral
pterygoid and medial pterygoid muscles (Fig. 2A and B). Normal anatomic structures
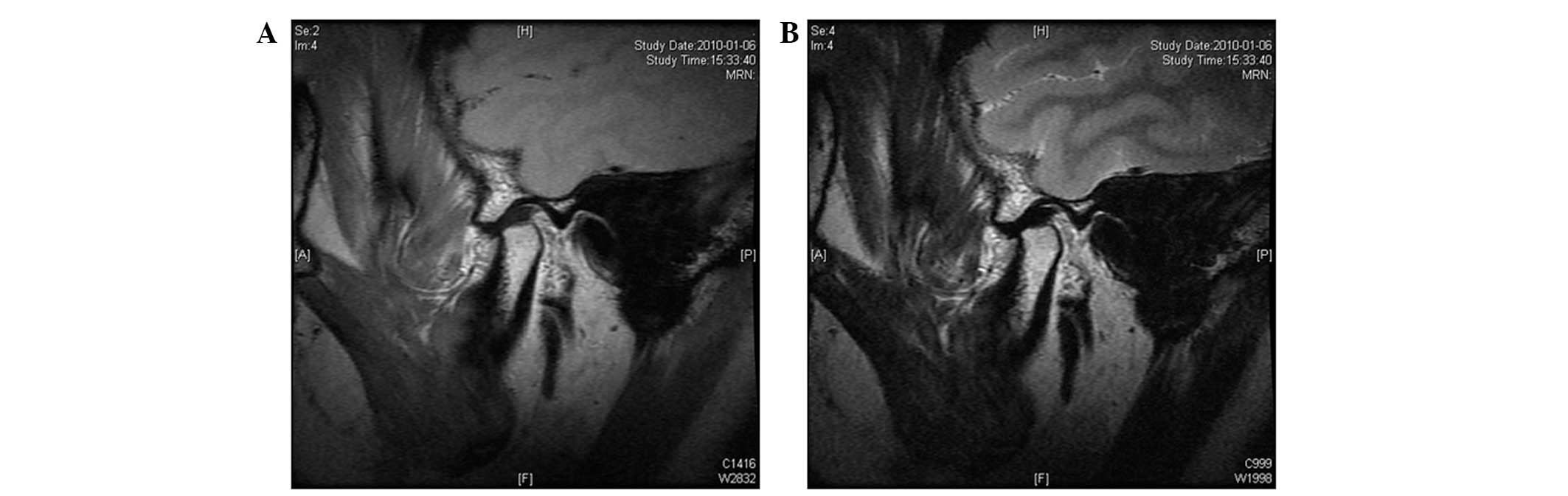
between the articular disk and the condyle were observed on
magnetic resonance imaging (MRI; Fig.
3A and B). Accounting for the medical history and
clinicoradiological results, the patient was diagnosed with MO in
the right lateral and medial pterygoid muscles.
Surgical excision was performed under general
anesthesia and, following fiber optic assisted intubation, access
to the mandibular was achieved via a preauricular incision, which
extended to the temporal region and exposed the condylar process
and sigmoid notch, as well as the coronoid process. To remove the
calcification in the lateral pterygoid muscle and reduce the
tension on the mandible caused by the temporalis, a right
coronoidectomy was performed using a reciprocating saw. The
majority of the calcified and fibrotic fibers of the upper head of
the right lateral pterygoid muscle were removed. An additional
intraoral approach to the medial aspect of the mandibular was
adopted via a mucoperiosteal incision of the retromolar area to
reveal and access the calcified medial pterygoid muscle. A pedicled
buccal fat pad (BFP) flap was used to fill the dead space. A
calcified mass was identified and subsequently excised. In
addition, the masseter attachment was stripped from the ramus of
the mandible to weaken the contractile force of the masseter muscle
and mouth opening of 40 mm was achieved intraoperatively. The right
maxillary third molar residual root was removed. The wound was
closed in layers following the achievement of complete hemostasis.
The healing period was uneventful and a postoperative panoramic
radiograph and a CT scan were performed four days following
surgery, which revealed that the ossification had been excised
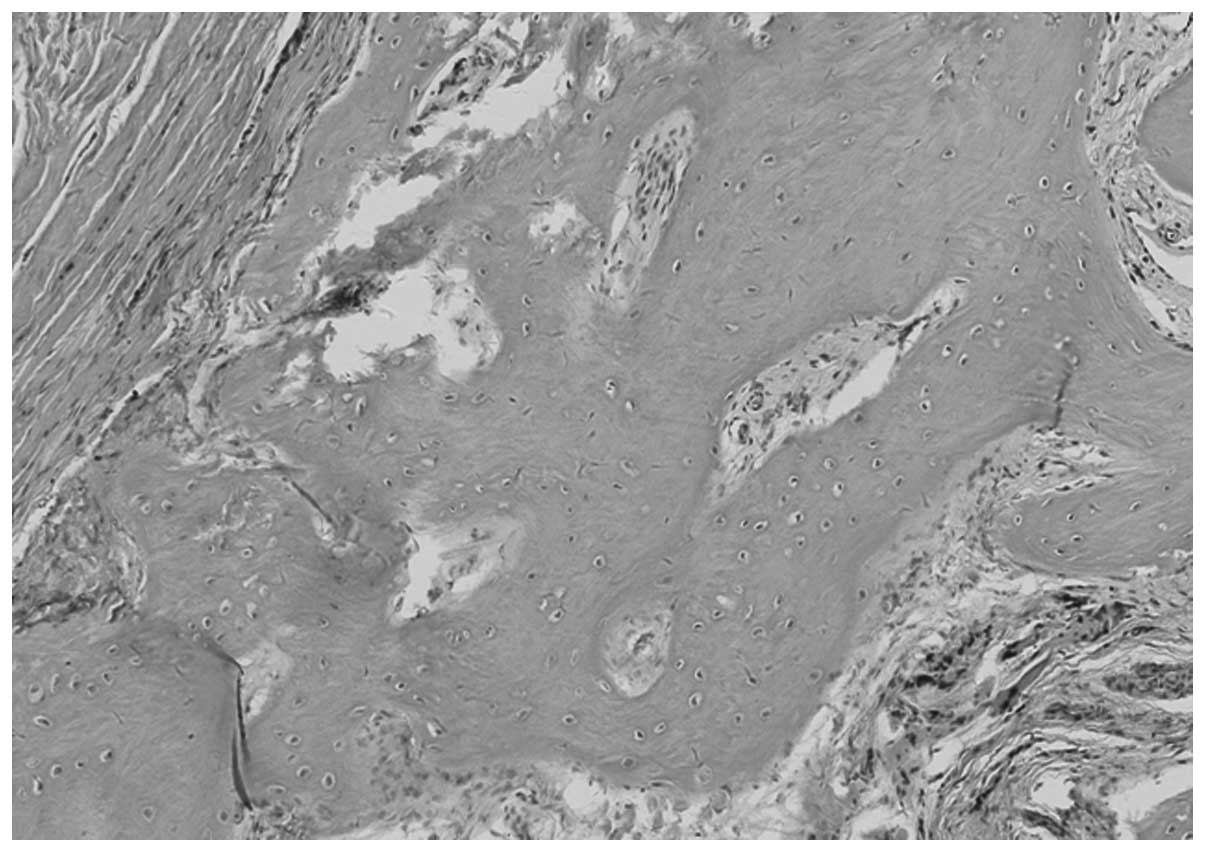
(Figs. 1B and 2C). Histopathology of the excised tissue
specimens (Fig. 4) identified the
novel formation of bone and osteoid within the muscle fibers.
Physical therapy was initiated in the immediate postoperative
period using suitable analgesics (200 mg celecoxib, twice a week,
for one week) and was continued following discharge from the
hospital. Maximum spontaneous mouth opening of 30 mm was achieved
seven days following surgery.
The patient was followed up for a total of 36 months
postoperatively. At present, the patient exhibits a stable
interincisal opening of 25 mm.
Discussion
MO presenting in the masticatory muscles is rare; a
review of the literature, which was conducted in the present study
identified only 20 cases reported since 2001. The results of the
literature review are presented in Tables I–III. The mean patient age was 36.75 years
(range, 18–68 years). Nineteen of the 20 patients initially
attended the hospital presenting with restricted mouth opening. Of
the 20 patients, 16 were diagnosed with PTMO as a result of facial
trauma (4–10), local infiltration of anesthetics
(1,11–15),
dental surgery (16,17) or absolute alcohol injection
(18). However, the remaining four
patients had no evident history of trauma, tooth extraction or
infection (2,19,20,22).
Among the patients diagnosed with PTMO, males predominated (ratio
of males to females, 11:5), which may be attributed to the fact
that males are more likely to be subject to trauma in daily life
(10). The region where PTMO most
frequently occurred was the medial pterygoid muscles, which was
often caused by a local anesthesia injection, followed by the
application of external force directly to the temporalis and
masseter muscles. The present review of the literature revealed
that out of the 20 cases observed, the surgical management of one
case (14) was performed at the
early stage of PTMO in the temporalis without the observation of
calcification, however, in the other cases, surgery was conducted
when trismus occurred and calcification was identified via CT. In
addition, of the 17 patients that were followed up, 10 patients
were continued with the follow-up for more than one year and four
patients exhibited recurrence subsequent to the first surgical
treatment.
 | Table ICase reports of myositis ossificans in
mascatory muscles (20 cases reported since 2001). |
Table I
Case reports of myositis ossificans in
mascatory muscles (20 cases reported since 2001).
| Author (Ref.) | Patient (Age,
years/Gender) | Location | Chief complaint | History of
trauma | Disease duration | MIO
(preopertion) | Treatment | MIO
(Intraoperation) | MIO (follow-up) | Outcome |
|---|
| Nemoto et al
(5) | 39/M | Masseter; temporalis;
lateral pterygoid; frontalis | Trismus mass | Repeatedly struck on
the face with a plastic hammer | >1 year | 5 mm | Excision + muscle
release + bilateral coronoidecomy | 55 mm | 37 mm (1 year) | No recurrence |
| Jayade et al
(2) | 25/F | Medial pterygoid;
lateral pterygoid; temporalis | Pain; swelling;
trismus | None | >6 months | 2 mm | Osteotomy + excision
+ contralateral coronoidectomy | 45 mm | 39 mm (3 months) | No recurrence |
| Guarda-Nardini et
al (4) | 50/M | Temporalis | Pain; trismus | Trauma injury | 40 days | 12 mm | Excision +
coronoidectomy | Good | 35 mm (6 months) | No recurrence |
| Choudharya et
al (6) | 31/M | Medial pterygoid | Trismus; mass | Panfacial trauma | 3 years | 8 mm | Excision | 37 mm | 27 mm (30
months) | No recurrence |
| Thangavelu et
al (11) | 36/F | Medial
pterygoid; | Trismus; pain | Anesthesia injection
+ tooth extraction | 3 months | 3 mm | Osteotomy + excision
+ abdominal fat graft | 32 mm | 28 mm (9 months) | No recurrence |
| Godhi et al
(19) | 21/M | Medial pterygoid;
lateral pterygoid; temporalis | Pain; swelling;
trismus; mass | None | 6 years | 5 mm | Osteotomy + excision
+ reconstruction plate with a condyle | 42 mm | Gradual decline (1
year) | Unknown |
| Trautmann et
al (12) | 33/M | Medial pterygoid | Trismus; tenderness;
swelling | Anesthetic injection
+ endodontic treatment | 2 months | 5 mm | Coronoidectomy +
partial resection of calcified medial pterygoid | Unknown | Limitation (3 years
after the second surgery) | Recurred twice |
| Ramieri et al
(13) | 64/M | Medial pterygoid | Swelling;
trismus | Anesthetic injection
+ tooth extraction | 3 years | 15 mm | Excision | 38 mm | Unknown | Unknown |
| Kruse et al
(20) | 35/F | Masseter | Trismus;
tenderness | None | 12 years | 10 mm | Conservation
treatment | Unknown | Unchanged (10
mm) | Regular
follow-up |
| Conner and Duffy
(1) | 18/F | Medial pterygoid;
temporalis masseter | Pain; trismus; | Anesthetic
injection + teeth extraction | 4 months | 4 mm | Excision +
coronoidectomy | Unknown | 25 mm (>18
months after the third surgery) | No recurrence
(after the third surgery) |
| Bansal et al
(16) | 20/F | Buccinators; medial
pterygoid | Trismus | Dento alveolar
trauma | 2 years | 1 mm | Excision +
bilateral coronoidecomy + ipsilateral palatal pedicle flap | 35 mm | 30 mm (1 year) | No recurrence |
| Rattan et al
(18) | 45/M | Medial
pterygoid | Trismus | Absolute alcohol
injection | 8 months | 7 mm | Excision + pedicled
buccal fat pad flap | 30 mm | 45 mm (2
years) | No recurrence |
| Mazano et al
(21) | 51/M | Temporalis | Trismus; mass | Severe trauma | 25 years | 13 mm | Excision | Unknown | 38 mm (1 year) | No recurrence |
| Yano et al
(8) | 34/M | Masseter | Trismus | Criminal
violence | Half year | 5 mm | Excision +
coronoidecomy | 30 mm | 40 mm (10
months) | No recurrence |
| Uematsu et
al (22) | 38/F | Temporalis | Pain; mass | None | 2 weeks | Unknown | Excision | Unknown | Unknown | Unknown |
| St Hilaire et
al (14) | 68/M | Masseter;
temporalis | trismus | Anesthesia
injection + tooth treatment | 2 weeks | 5 mm | Coronoidectomy +
excision + a penrose drain placed | 41 mm | 40 mm (3.5
years) | No recurrence |
| Saka et al
(9) | 33/M | Temporalis | Trismus; pain;
swelling | Blunt trauma | 3 weeks | Limited mouth
opening | Excision | Unknown | Unlimited mouth
opening (4 years) | No recurrence |
| Aoki et al
(10) | 44/M | Masseter; lateral
pterygoid; | Trismus; pain;
swelling; tenderness | Blunt trauma to the
face | 1 year | 7 mm | Excision | 32 mm | 10 mm (10th day
after surgery) | Recurrence |
| Kim et al
(15) | 30/F | Lateral
pterygoid; | Trismus | Anesthesia
injection + tooth treatment | 3 years | 8 mm | Coronoidectomy +
excision + interpositional abdominal fat graft placed | 27 mm (in the final
surgery) | 12 mm passively
(after the final surgery) | Multiple
recurrences |
| Mevio et al
(17) | 55/F | Temporalis | Trismus | Dental surgery | 18 months | 6 mm | Coronoidectomy +
excision | Unknown | Correct mouth
opening | No recurrence |
 | Table IIIPrecipitating factors of myositis
ossificans in the masticatory muscles (20 cases reported from
2001). |
Table III
Precipitating factors of myositis
ossificans in the masticatory muscles (20 cases reported from
2001).
| Patients |
|---|
|
|
|---|
| Precipitating
factor | n | % |
|---|
| Facial trauma | 8 | 40 |
| Local infiltration
of anesthetics | 6 | 30 |
| Dental surgery | 1 | 5 |
| Local infiltration
of absolute alcohol | 1 | 5 |
| Unknown | 4 | 20 |
The exact mechanism for the pathogenesis of MO
remains unclear, however, trauma is considered to be the inciting
event. According to the literature, a signal, such as a bone
morphogenetic protein (BMP) signal from the site of injury, may
induce mesenchymal cells to differentiate into osteoblasts or
chondroblasts, given the appropriate environment (23,24).
In the field of stomatology, odontogenic infection is a common
condition when accompanied by trauma. In the present case, the
smaller, superficial head of the medial pterygoid muscle, which
originates from the maxillary tuberosity was proximal to the
maxillary third molar. Therefore, apical periodontitis of the third
maxillary molar may have spread toward the medial pterygoid
muscles. Furthermore, infections in the medial pterygoid muscles
may have spread toward the lateral pterygoid muscles through
potential fascial spaces containing loose connective tissue.
Long-term, low-grade inflammation may have stimulated the
appropriate signaling agents, such as BMP, to induce heterotopic
bone formation. Thus, it is hypothesized in the present report that
infection and trauma exhibit an equally important role in the
pathogenesis of MO in the masticatory muscles. Therefore, the
present case was diagnosed as PIMO.
Ossification, the symptom of MO, may be observed by
diagnostic imaging tests a minimum of 2–5 weeks subsequent to
injury (25–27). After eliminating temporomandibular
joint disease using MRI, CT and three-dimensional CT scans are
considered to be particularly efficacious investigative tools in
the oral and maxillofacial region. These imaging techniques aid
with identifying the exact location and shape of the ossification,
as well as establishing the association between the lesion and
surrounding tissues, which is important for surgical treatment.
Although a panoramic radiograph may not be effective for
determining the exact extent of the lesion, due to the
superimposition of the cranial bones, it may aid with the
identification of odontogenic infection foci. Bone scans and
ultrasound may also be used, however, are rarely applied for the
craniofacial region (28).
Treatment of PTMO and PIMO usually includes surgical
excision of the calcification and the surrounding muscles. Patients
with MO of the temporalis or masseter area often undergo a
coronoidectomy and the excision of the involved calcified muscles;
whereas MO of the pterygoid muscle is more debilitating and, thus,
the management of these types of patient is more complicated than
that of the patients exhibiting MO of other masticatory muscles.
According to the experiences of the present study, the following
approaches should be considered: i) Transoral and extraoral
approaches, which are often used to provide access to the medial
aspect of the mandibular ramus to allow complete excision of the
ossified muscle; ii) protection of the internal maxillary artery
and inferior alveolar nerves (this is considered to be critical);
and iii) using a BFP flap to fill the dead space for preventing
hematoma formation and heterotopic bone reformation (29,30).
Two types of free fat, abdominal fat and the BFP, have been
reported that may serve as interpositional material. The BFP has
been identified as a particularly effective autogenous tissue,
which has been demonstrated in a multitude of surgical procedures
in the maxillofacial region (31,32).
The BFP lies in close proximity to the site of surgery and may be
used as a pedicled or random-pattern flap along with its own blood
supply, so there are fewer instances of resorption when compared
with an abdominal fat transfer.
In conclusion, a case of PIMO in the medial and
lateral pterygoid muscles is presented and chronic low-grade
infection was identified to be an important consideration in
addition to other possible precipitating factors in the occurrence
of MO. Panoramic radiography revealed the source of infection and
CT scans effectively delineated the calcified mass. A positive
outcome was achieved for the patient by the surgical excision of
the calcification and ossified muscles, and via the use of a BFP
flap to fill the dead space. This study indicates that symptomatic
wisdom teeth must be removed as soon as possible, to prevent
infection. In addition, it is important to considered infection as
a factor which may lead to myositis ossificans.
Acknowledgements
The present study was supported by National Science
Foundation of China (grant no’s. 81100824 and 81070848) and the
Foundation of Shanghai Municipal Education Commission (grant no’s.
12YZ044 and 13XD1402300).
References
|
1
|
Conner GA and Duffy M: Myositis
ossificans: a case report of multiple recurrences following third
molar extractions and review of the literature. J Oral Maxillofac
Surg. 67:920–926. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jayade B, Adirajaiah S, Vadera H, et al:
Myositis ossificans in medial, lateral pterygoid, and contralateral
temporalis muscles: a rare case report. Oral Surg Oral Med Oral
Pathol Oral Radiol. 3:e1–e6. 2012.
|
|
3
|
Kaplan FS, Seemann P, Haupt J, et al:
Investigations of activated ACVR1/ALK2, a bone morphogenetic
protein type I receptor, that causes fibrodysplasia ossificans
progressiva. Methods Enzymol. 484:357–373. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Guarda-Nardini L, Piccotti F, Ferronato G
and Manfredini D: Myositis ossificans traumatica of the temporalis
muscle: a case report and diagnostic considerations. Oral
Maxillofac Surg. 16:221–225. 2012. View Article : Google Scholar
|
|
5
|
Nemoto H, Sumiya N, Ito Y, et al: Myositis
ossificans traumatica of the masticatory muscles. J Craniofac Surg.
23:e514–e516. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Choudharya AK, Sahoob NK and
Chattopadhyaya PK: Myositis ossificans traumatica of the medial
pterygoid muscle: A case report. J Oral Maxillofac Surg.
24:241–244. 2012.
|
|
7
|
Manzano D, Silván A, Saez J and Moreno JC:
Myositis ossificans of the temporalis muscle. Case report. Med Oral
Patol Oral Cir Bucal. 12:E277–E280. 2007.PubMed/NCBI
|
|
8
|
Yano H, Yamamoto H, Hirata R and Hirano A:
Post-traumatic severe trismus caused by impairment of the
masticatory muscle. J Craniofac Surg. 16:277–280. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saka B, Stropahl G and Gundlach KK:
Traumatic myositis ossificans (ossifying pseudotumor) of temporal
muscle. Int J Oral Maxillofac Surg. 31:110–111. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Aoki T, Naito H, Ota Y and Shiiki K:
Myositis ossificans traumatica of the masticatory muscles: review
of the literature and report of a case. J Oral Maxillofac Surg.
60:1083–1088. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Thangavelu A, Vaidhyanathan A and Narendar
R: Myositis ossificans traumatica of the medial pterygoid. Int J
Oral Maxillofac Surg. 40:545–549. 2012. View Article : Google Scholar
|
|
12
|
Trautmann F, Moura Pd, Fernandes TL, et
al: Myositis ossificans traumatica of the medial pterygoid muscle:
a case report. J Oral Sci. 52:485–489. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ramieri V, Bianca C, Arangio P and Cascone
P: Myositis ossificans of the medial pterygoid muscle. J Craniofac
Surg. 21:1202–1204. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
St-Hilaire H, Weber WD, Ramer M and
Lumerman H: Clinicopathologic conference: trismus following dental
treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
98:261–266. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim DD, Lazow SK, Har-El G and Berger JR:
Myositis ossificans traumatica of masticatory musculature: A case
report and literature review. J Oral Maxillofac Surg. 60:1072–1076.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bansal V, Kumar S and Mowar A: Unusual
causes of trismus: a report of two cases. J Maxillofac Oral Surg.
8:377–380. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mevio E, Rizzi L and Bernasconi G:
Myositis ossificans traumatica of the temporal muscle: a case
report. Auris Nasus Larynx. 28:345–347. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rattan V, Rai S and Vaiphei K: Use of
buccal pad of fat to prevent heterotopic bone formation after
excision of myositisossificans of medial pterygoid muscle. J Oral
Maxillofac Surg. 66:1518–1522. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Godhi SS, Singh A, Kukreja P and Singh V:
Myositis ossificans circumscripta involving bilateral masticatory
muscles. J Craniofac Surg. 22:e11–e13. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kruse AL, Dannemann C and Grätz KW:
Bilateral myositis ossificans of the masseter muscle after
chemoradiotherapy and critical illness neuropathy-report of a rare
entity and review of literature. Head Neck Oncol. 1:30–35. 2009.
View Article : Google Scholar
|
|
21
|
Manzano D, Silván A, Saez J and Moreno JC:
Myositis ossificans of the temporalis muscle. Case report. Med Oral
Patol Oral Cir Bucal. 12:E277–E280. 2007.PubMed/NCBI
|
|
22
|
Uematsu Y, Nishibayashi H, Fujita K, et
al: Myositis ossificans of the temporal muscle as a primary scalp
tumor. Case report. Neurol Med Chir (Tokyo). 45:56–58. 2005.
View Article : Google Scholar
|
|
23
|
Yu PB, Deng DY, Lai CS, et al: BMP type I
receptor inhibition reduces heterotopic ossification. Nat Med.
14:1363–1369. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Katagiri T: BMP signaling and bone
formation. Clin Calcium. 22:1677–1683. 2012.PubMed/NCBI
|
|
25
|
Shirkhoda A, Armin AR, Bis KG, et al: MR
imaging of myositis ossificans: variable patterns at different
stages. J Magn Reson Imaging. 5:287–292. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Amendola MA, Glazer GM, Agha FP, et al:
Myositis ossificans circumscripta: computed tomographic diagnosis.
Radiology. 149:775–779. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
McCarthy EF and Sundaram M: Heterotopic
ossification: a review. Skeletal Radiol. 34:609–619. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Trautamann F, Moura Pd, Fernandes TL,
Gondak RO, Castilho JC and Filho EM: Myositis ossificans traumatica
of the medial pterygoid muscle: a case report. J Oral Sci.
52:485–489. 2010. View Article : Google Scholar
|
|
29
|
Chen MJ, Yang C, Qui YT, et al: Local
resection of the mass to treat the osteochondroma of the mandibular
condyle: indications and different methods with 38-case series.
Head Neck. 36:273–279. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chen MJ, Yang C, Cai XY, et al: Synovial
chondromatosis in the inferior compartment of the temporomandibular
joint: different stages with different treatments. J Oral
Maxillofac Surg. 70:e32–e38. 2012. View Article : Google Scholar
|
|
31
|
Rattan V: A simple technique for use of
buccal pad of fat in temporomandibular joint reconstruction. J Oral
Maxillofac Surg. 64:1447–1451. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Stuzin JM, Wagstrom L, Kawamoto HK, et al:
The anatomy and clinical applications of the buccal fat pad. Plast
Reconstr Surg. 85:29–37. 1990. View Article : Google Scholar : PubMed/NCBI
|