Introduction
Olfactory ensheathing cell tumors (OECTs) are rare
malignancies of the anterior fossa that share similar clinical and
radiological features with olfactory groove schwannomas (OGS)
(1). Forming a pre-operative
diagnosis is challenging due to these similarities, which include
anosmia. It is also necessary to differentiate these malignancies
from common meningiomas in the anterior fossa (2). OECT was first identified as a distinct
entity by Yasuda et al in 2006 (1), and only seven cases have been reported
to date (1,3–8).
Therefore, little information is available with regard to the
clinical, radiological and immunohistochemical characteristics of
OECTs (5). The current study presents
the first reported case of OECT in China, which occurred in a
20-year-old male. In addition, the seven known cases are reviewed,
with a summary of the clinical manifestations, imaging
characteristics, intraoperative findings and immunohistochemical
features of OECTs. This provides important clinical information for
the pre-operative diagnosis and intraoperative removal of
OECTs.
Case report
A 20-year-old male was admitted to The First
Hospital of Jilin University (Changchun, Jilin, China), after
presenting with a severe headache lasting for one day and a
generalized convulsion, during which the patient lost consciousness
for 30 min. The medical history included intermittent headaches for
four years, which had been treated with painkillers as required.
Upon examination, no neurological deficits were identified.
Olfactory function was normal and no stigmata of neurofibromatosis
were observed.
Cranial magnetic resonance imaging (MRI) revealed a
round, patchy mass of 3.4×2.6×5.0 cm in the left anterior fossa,
with long T1 and T2 signals. The lesion was hypointense on the
fluid-attenuated inversion recovery sequence. Heterogeneous
enhancement and necrosis of the tumor were observed following
intravenous gadolinium injection (Fig.
1). Abnormal long T1 and T2 signals were observed in the
tumor-adjacent tissues without enhancement. The lateral ventricles
and third ventricle were enlarged with a right and posterior shift
of the midline. Abnormal long T2 signals were observed in the
thickened mucosa of the bilateral ethmoidal sinuses. The diagnosis
was of an occupying lesion (possible meningioma) in the left
anterior fossa.
The patient was placed under general anesthesia and
a left frontal craniotomy was performed via a coronal incision. The
tumor was located on the base of the left anterior fossa,
posteriorly extending into the anterior clinoid process. The tumor
was slightly adherent to the dura mater of the anterior fossa, and
was surrounded by the arachnoid membrane. The tumor had grown
toward the left olfactory groove and compressed the left frontal
cortex. The tumor presented with a greyish-red appearance, cystic
necrosis and a rich blood supply, with a rubbery encapsulation
creating a distinct boundary from the surrounding brain tissue. The
tumor was debulked and completely removed, as confirmed by a
post-operative computed tomography (CT) scan. The left olfactory
bulb and nerve tract were not observed during the surgery.
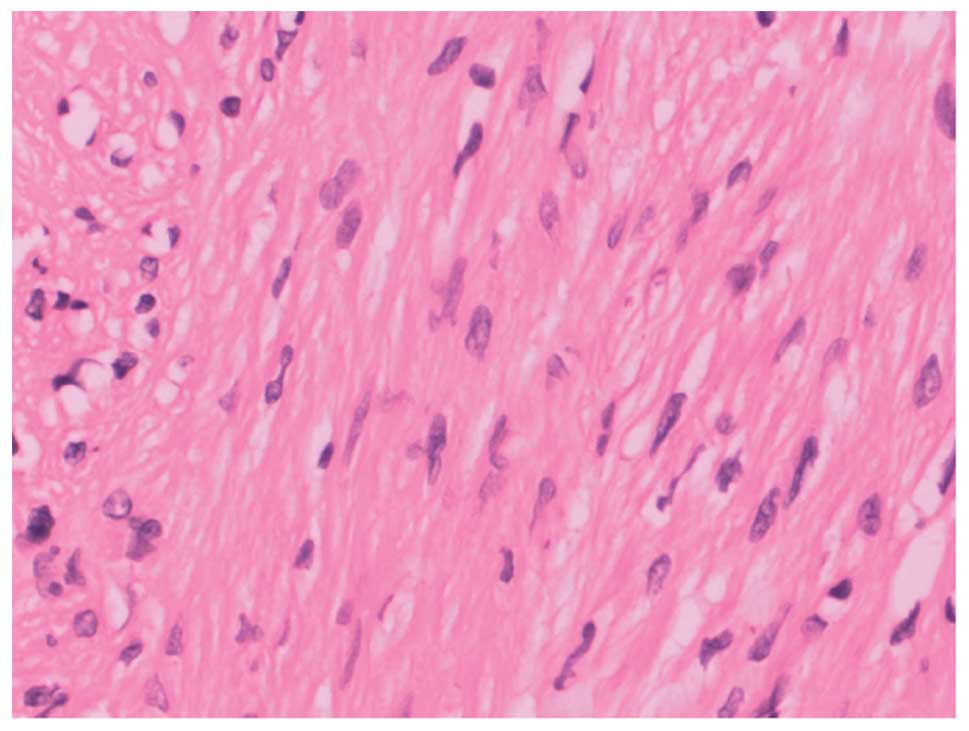
Post-operative hematoxylin and eosin (HE)-stained
sections revealed that the tumor was composed of spindle-shaped
cells, predominantly arranged in compact fascicles or fibrous
cords, with a few cells arranged in whorls. The matrix contained
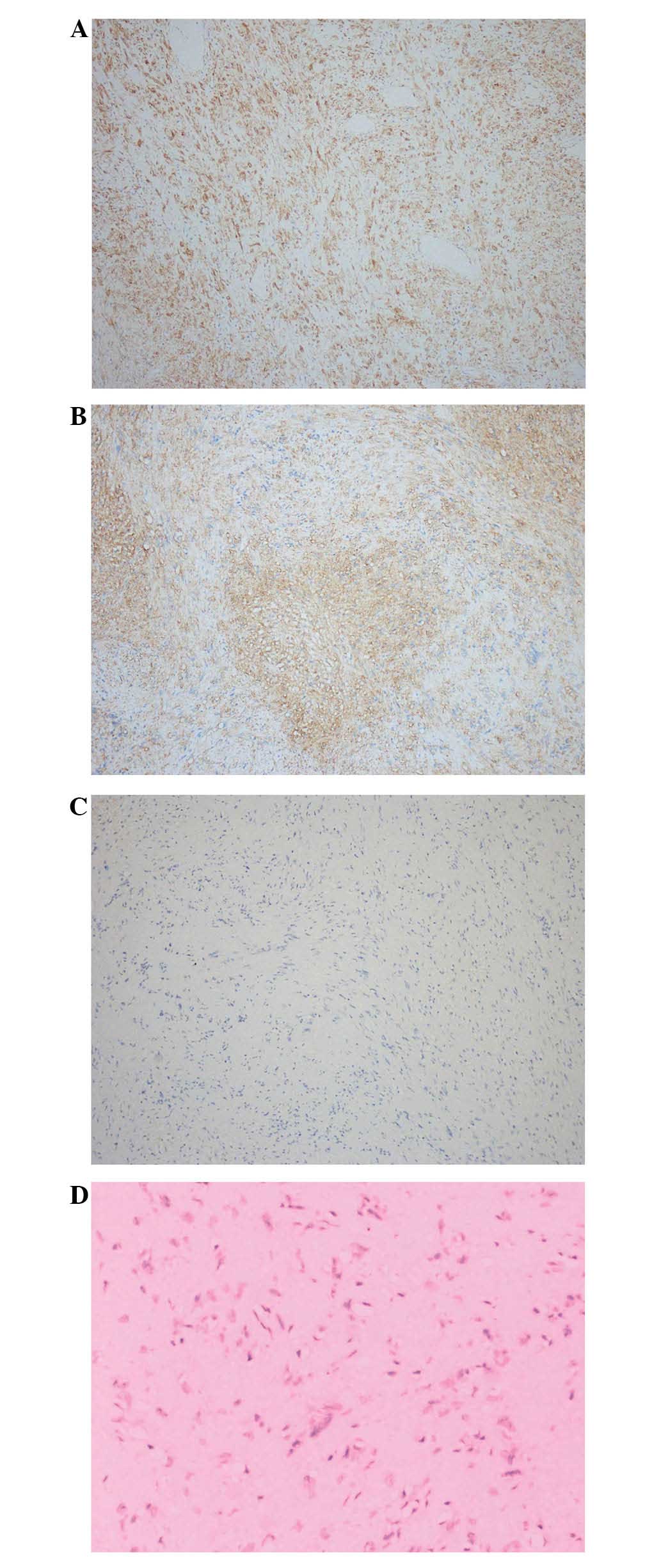
bundles of mature collagen fibers parallel to the cells (Fig. 2). Immunohistochemical staining
revealed that the tumor was immunopositive for vimentin and S-100,
and immunonegative for epithelial membrane antigen and Leu-7
(Fig. 3), leading to a final
diagnosis of OECT.
The post-operative course was uneventful, and the
patient was discharged two weeks after surgery, without headache
but with left-sided anosmia. The patient was in relatively good
health during the two-month follow-up examination, despite
persistent left-sided anosmia. A cranial MRI revealed no recurrence
of the tumor.
Discussion
OECT was first identified as a being distinct from
schwannoma based on its Leu-7 immunoreactivity (1). The current study is the eighth reported
case of OECT. Table I summarizes the
clinical manifestations, imaging characteristics, intraoperative
findings and immunohistochemical features of all reported cases.
There appears to be no gender difference amongst the eight OECT
cases, with four male and four female patients affected. The
patient in the present case is the youngest from the reported
cases, and the average age of the OECT patients is 34.1 years
(range, 20–49 years). This is younger than that of patients with
schwannomas (9).
 | Table I.Summary of the eight published
olfactory ensheathing cell tumor cases. |
Table I.
Summary of the eight published
olfactory ensheathing cell tumor cases.
| A, Yasuda et
al, 2006 (1) |
|---|
|
|---|
| Parameter | Findings |
|---|
| Patient
gender/age | Female/31 years |
| Symptoms and
signs | Generalized
convulsion; loss of olfactory sensation through the right nostril
of the nose; no other abnormalities |
| Skin | No nevus or
pigmentation |
| Radiological
findings | CT: Tumor of 6.5 cm
in diameter with calcified nodules located slightly right of the
center of the anterior skull base. MRI: Round structure exhibiting
high intensity on T1WI and low intensity on T2WI; finger-like
extensions toward the cerebral parenchyma; heterogeneous
enhancement; no edema. Angiography: Avascular structure. EEG:
Sporadic slow waves in the right frontal area. |
| Intraoperative
findings | The tumor was totally
removed. The tumor was capsulated and attached strongly to the
right olfactory groove. The right olfactory bulb was absent, and a
5-mm bone defect was identified on the right olfactory groove. The
tumor extended into the sinus through the bone defect. The bone
defect was repaired. |
| Outcome | Uneventful |
| Follow-up | No recurrence during
16-month follow-up |
| Electron microscopic
findings | Amoeba-like
cytoplasmic process; irregular nucleus with marginally distributed
chromatin; abundant collagen fibers around the cells. The outer
surface of the cell was covered with an interrupted thin layer of
basal lamina. |
| Pathological
findings | Spindle-shaped cells
in an interwoven pattern; distorted and twisted nuclei; wavy
cellular arrangement in an atypical palisading pattern. |
|
| B, Ippili et
al, 2009 (3) |
|
| Parameter | Findings |
|
| Patient
gender/age | Male/42 years |
| Symptoms and
signs | Multiple episodes of
generalized tonic clonic seizures; normal olfaction; no local
neurological deficits |
| Skin | No neurocutaneous
markers |
| Radiological
findings | CT: Extra-axial
isodense mass in the left subfrontal region; homogenously enhanced
with contrast. MRI: Isointense on T1WI and mildly hyperintense on
T2WI and FLAIR. |
| Intraoperative
findings | Excision of the tumor
was performed via a left frontal craniotomy. The tumor was
partially removed by suction and partially fibrous, and arose from
the left olfactory bulb. |
| Outcome | Uneventful |
| Follow-up | No recurrence during
the one-year follow-up |
| Electron microscopic
findings | NA |
| Pathological
findings | Spindle-shaped cells
arranged in short fascicles, palisades and whorls. The cells were
spindled out with curved vesicular nuclei and ill-defined
cytoplasmic margins. |
|
| C, Lin et al,
2010 (4) |
|
| Parameter | Findings |
|
| Patient
gender/age | Male/32 years |
| Symptoms and
signs | Seizure attacks for
six months, with one episode resulting in a traffic accident; no
neurological deficits |
| Skin | No abnormality or
stigmata of neurofibromatosis |
| Radiological
findings | MRI: 3.6×3.3×3.9-cm,
extra-axial well-defined mass at the left frontal base; hypointense
on T1WI and isointense on T2WI; heterogeneously enhanced after
intravenous gadolinium administration; intact cribriform plate; no
dural tail sign; no ethmoidal sinus invasion. |
| Intraoperative
findings | The tumor was
completely removed via frontal craniotomy. The tumor was
greyish-white with a glistening appearance and rubbery consistency
over the frontal base region. The tumor was traced to the proximal
part of the left olfactory tract. The olfactory bulb was not
identified. Intact frontal skull base. |
| Outcome | Uneventful |
| Follow-up | No recurrence during
the six-month follow-up |
| Electron microscopic
findings | Amoeba-like
cytoplasmic process; irregular or indented nucleus in the center of
the cell. The chromatin was evenly distributed throughout the
karyoplasm, and slightly condensed below the nuclear membrane. No
prominent external lamina. A layer of interrupted deposits of basal
lamina at certain parts of the cellular membrane was observed.
Numerous extra cellular collagen fibers were present. |
| Pathological
findings | Low cellular tumor
with dense hyalinization in the majority of areas. Tumor cells had
ovoid to elongated, normochromatic and often comma-shaped nuclei.
The cells had no particular arrangement. Myxoid changes of stroma
were prominent in focal areas with no necrosis, mitosis or
hypercellularity. A previous hemorrhage with hemosiderin deposition
was observed. |
|
| D, Darie et
al, 2010 (5) |
|
| Parameter | Findings |
|
| Patient
gender/age | Female/28 years |
| Symptoms and
signs | 18-month history of
complex partial seizures, emotional lability, and anosmia; no
increase in intracranial pressure; no visual symptoms |
| Skin | No cutaneous stigmata
of neurofibromatosis; no family history of von Recklinghausen
disease |
| Radiological
findings | CT: Homogenous
extra-axial isodense lesion at the middle of anterior cranial fossa
with a left preponderance development; bone window coronal CT scan
showed skull base erosion under the tumor bulk. MRI: Mass of
4×3.5×2.5 cm; hypointense on T1WI; hyperintense on T2WI and FLAIR
without surrounding edema; strong heterogeneous enhancement of the
tumor after intravenous gadolinium injection. |
| Intraoperative
findings | A total excision of
the tumor via a left frontal pterional craniotomy was performed.
The tumor was whitish, firm and non-hemorrhagic, with erosion into
the cranial base; the tumor was surrounded by arachnoiditis and
connected to the anterior part of the cribriform plate and the left
olfactory tract. The right olfactory tract displaced laterally and
was preserved, however the left olfactory tract was removed due to
close adhesion to the tumor. Bone scalloping was observed
underneath the tumor; no bone defect was disclosed. The dura mater
defect was repaired by a temporalis flap and fibrin glue. |
| Outcome | Anosmia |
| Follow-up | No recurrence during
the 16-month follow-up |
| Electron microscopic
findings | NA |
| Pathological
findings | Well-circumscribed
tumor respecting the arachnoid space and the cerebral tissue. The
tumor showed an atypical fibrous component with a few areas of
compact spindle-shaped cells and no necrosis, mitosis or
hypercellularity. |
|
| E, Yamaguchi et
al, 2010 (6) |
|
| Parameter | Findings |
|
| Patient
gender/age | Female/30 years |
| Symptoms and
signs | Headache for several
months with right anosmia; no other neurological deficits |
| Skin | NA |
| Radiological
findings | CT: Three-dimensional
CT revealed erosion of the cribriform plates. MRI: Heterogeneously
enhancing mass of ∼4 cm in diameter in the frontal base. |
| Intraoperative
findings | The tumor was
completely removed via a bilateral frontal craniotomy. The tumor
was located in the intradural, extra-axial space, attached to the
right cribriform plate. |
| Outcome | Olfactory function
was not restored |
| Follow-up | NA |
| Electron microscopic
findings | NA |
| Pathological
findings | Tumor cells formed
patterns of compact fascicular Antoni A areas with palisading
nuclei. |
|
| F, Ogino-Nishimura
et al, 2012 (7) |
|
| Parameter | Findings |
|
| Patient
gender/age | Female/41 years |
| Symptoms and
signs | Headache and loss of
olfactory function |
| Skin | NA |
| Radiological
findings | CT: Lesion at the
olfactory cleft that extended superiorly to the olfactory groove,
with a bone defect in the skull base; the cribriform plate was
elevated upward. MRI: Mass showing cystic changes, with solid
portions demonstrating strong post gadolinium contrast enhancement.
Nasal endoscopy: Soft, whitish mass occupying the olfactory cleft
and extending laterally to the middle meatus, with destruction of
the middle turbinate in the left nostril. |
| Intraoperative
findings | Subtotal resection of
the tumor via an endoscopic endonasal approach was performed. The
tumor was attached, but had not invaded the internal orbital wall.
The tumor was debulked with an ultrasonic surgical aspiration. The
bone defect was covered with a mucoperiosteal pedicle flap. |
| Outcome | Uneventful |
| Follow-up | No recurrence during
the two-year follow-up |
| Electron microscopic
findings | NA |
| Pathological
findings | Tumor composed of
cells with eosinophilic cytoplasm and elongated or wavy nuclei with
occasional symplastic changes. The mitotic index was <1 per 10
high-power fields. No tumor necrosis was observed, and the Ki-67
labeling index was 2%. |
|
| G, Al-Ghanem et
al 2013 (8) |
|
| Parameter | Findings |
|
| Patient gender/
age | Male/49 years |
| Symptoms and
signs | Visual impairment and
hyposmia |
| Skin | NA |
| Radiological
findings | CT and MRI:
Subfrontal cystic extra-axial mass that eroded the right cribriform
plate |
| Intraoperative
findings | A total excision of
the tumor via bilateral craniotomy was performed. |
| Outcome | NA |
| Follow-up | NA |
| Electron microscopic
findings | NA |
| Pathological
findings | NA |
|
| H, Present
case |
|
| Parameter | Findings |
|
| Patient
gender/age | Male/20 years |
| Symptoms and
signs | Severe headache
with a generalized convulsion; no anosmia; no neurological
deficits |
| Skin | No cutaneous stigma
of neurofibromatosis |
| Radiological
findings | MRI: Round, patchy
mass of 3.4×2.6×5.0 cm in the left anterior fossa, with long T1 and
T2 signals; hypointense on FLAIR sequence; heterogeneous
enhancement after intravenous gadolinium injection |
| Intraoperative
findings | The tumor was
completely removed through a left frontal craniotomy via a coronal
incision. The tumor extended into the anterior clinoid process, and
slightly adhered to the dura mater of the anterior fossa. The tumor
tended to grow toward the left olfactory groove, and had compressed
the left frontal cortex. The greyish-red tumor with rich blood
supply was capsulated with rubbery consistency, and clear
boundaries with surrounding brain tissues. Cystic necrosis inside
the tumor was observed. |
| Outcome | Left anosmia;
normal right olfactory function |
| Follow-up | No recurrence
during the two-month follow-up |
| Electron
microscopic findings | NA |
| Pathological
findings | Spindle-shaped
cells were predominantly arranged in compact fascicles or fibrous
cords, and a few cells were arranged in whorls. The matrix
contained bundles of mature collagen fibers parallel to the
cells. |
As OECTs are located in the anterior fossa close to
the olfactory nerve, olfactory dysfunction is a common clinical
manifestation (1,3–8). Five of
the seven cases reported in the literature presented with anosmia,
including two cases with right-sided anosmia, two cases with
bilateral anosmia and one case with hyposmia. However, the current
patient, along with two additional cases, had normal olfaction,
suggesting that olfactory dysfunction is not a necessary indicator
for OECT patients. In addition, seizures occurred in four cases,
including one case with a generalized convulsion (1), one case with multiple episodes of
generalized tonic clonic seizures (3), one case with seizure attacks for six
months (4), and one case with complex
partial seizures for 18 months (5).
In the present case, the patient experienced a severe headache with
a generalized convulsion, and also presented with a history of
intermittent headaches over four years, which may have been
associated with increased intracranial pressure. Furthermore,
emotional lability with complex partial seizures occurred in one
patient (6), and visual impairment
occurred in another case (8). No
cutaneous stigmata of neurofibromatosis were observed in any of the
cases, however, five cases, including the present case, reported
skin conditions.
All patients in the eight reported cases underwent
CT and/or MRI scans. Of the six patients for whom CT scans were
conducted, a tumor with calcified nodules was observed in one
patient (1), and homogenous
enhancement was found in another (3).
In addition, tumor invasion to the skull base and ethmoid bone was
reported in four cases. In certain cases, tumor erosion of the
cribriform plates or skull base was clearly visualized by
three-dimensional (6) and bone window
coronal (5) CT scans. Therefore,
these types of CT scan are strongly recommended due to their
ability to identify tumor invasion, and thus are useful for
distinguishing OECT from meningioma. One study reported that the
tumor appeared as an avascular structure on angiography (1). Tumors with cystic changes were described
in two cases (7,8), and strong post-gadolinium contrast
enhancement in the solid portions of the tumor was reported in one
case (7). Two cases reported that
there was no edema in the tissues surrounding the tumor (1,5), possibly
due to the encapsulation and expansive growth of the tumors. The
large diameter of the masses, ranging from 3.9 to 6.5 cm, is likely
due to the large space available in the anterior fossa, and the
prolonged growth period promoted by minimal intracranial pressure
symptoms. Heterogeneous enhancement of the tumor on MRI following
intravenous contrast administration was reported in six cases, and
no dural tail signs were observed in any of the eight cases. Tumor
necrosis was visible on enhanced MRI in the present case. Enhanced
MRI may therefore be useful for distinguishing OECTs from
meningiomas in the anterior fossa, which commonly display
homogeneous enhancement without any signs of necrosis (2). However, radiological imaging may be
unable to distinguish OECT from OGS.
To date, the only method that allows the distinction
of OECT from OGS is immunohistochemical staining: OECTs are
immunonegative for Leu-7 and epithelial membrane antigen, and
immunopositive for S-100, while OGSs are immunoreactive for Leu-7
(1). Other pathological
characteristics of OECTs include the arrangement of spindle-shaped
cells in fascicles, fibrous cords or whorls, with distorted nuclei
arranged in a palisading pattern, as observed by HE staining. In
the cases described, only one reported that the tumor had
indications of a previous hemorrhage with hemosiderin deposits
(4). Two cases reported electron
microscopic findings, in which amoeba-like cytoplasmic processes
with abundant collagen fibers around the cells were observed
(1,4).
Since OECTs are located in the midline or
extra-axial spaces, the majority of the tumors (7/8) were excised
via unilateral or bilateral frontal craniotomies, with a subtotal
incision performed via an endoscopic endonasal approach in one case
(7). The tumors were described as
greyish-white (4,5), firm (5) or
cystic (7), with less blood loss
during surgery compared with OGS. However, the tumor in the present
case was greyish-red with a rich blood supply and cystic necrosis.
Tumor invasion into the olfactory groove, cranial base, internal
orbital wall or cribriform plate was reported in four cases
(1,5–7), and the
bone or dura mater defects were repaired using a temporalis flap
and fibrin glue, or mucoperiosteal pedicle flaps (5,6). Similar
to two of the reported cases (1,4), in the
present case, the olfactory bulb and tract (left side) were not
observed. In addition, the current patient exhibited no tumor
recurrence at the two-month follow-up examination. Likewise, no
tumor recurrences were reported in the previous cases, with a mean
follow-up period of 14.8 months (range, 6–24 months).
Taken together, the results of the current case and
the eight reviewed cases indicate that a diagnosis of OECT should
be considered for tumors in the anterior fossa occurring in
patients with a history of single or multiple seizure attacks and
no cutaneous stigmata of neurofibromatosis, who present with tumor
invasion into the skull base and ethmoid bone on CT scans, and
heterogeneous enhancement of the tumor with no edema in surrounding
tissues on MRI scans. These encapsulated tumors tend to grow toward
the ethmoid bone with clear boundaries from surrounding tissue,
enabling their complete removal. If the tumor invades the bone, the
bone defect may be repaired by a mucoperiosteal pedicle flap and
fibrin glue. Although OECTs may be diagnosed by immunostaining,
further cases are required to enable further characterization of
the clinical findings, imaging features and immunohistochemical
properties of OECTs.
References
|
1
|
Yasuda M, Higuchi O, Takano S and
Matsumura A: Olfactory ensheathing cell tumor: a case report. J
Neurooncol. 76:111–113. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Morales-Valero SF, Van Gompel JJ,
Loumiotis I and Lanzino G: Craniotomy for anterior cranial fossa
meningiomas: historical overview. Neurosurg Focus. 36:E142014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ippili K, Ratnam BG, Gowrishankar S,
Ranjan A and Lath R: Olfactory ensheathing cell tumor. Neurol
India. 57:76–78. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lin SC, Chen MH, Lin CF and Ho DM:
Olfactory ensheathing cell tumor with neurofibroma-like features: a
case report and review of the literature. J Neurooncol. 97:117–122.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Darie I, Riffaud L, Saïkali S, Brassier G
and Hamlat A: Olfactory ensheathing cell tumour: case report and
literature review. J Neurooncol. 100:285–289. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yamaguchi T, Fujii H, Dziurzynski K,
Delashaw JB and Watanabe E: Olfactory ensheathing cell tumor: case
report. Skull Base. 20:357–361. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ogino-Nishimura E, Nakagawa T, Mikami Y
and Ito J: Olfactory ensheathing cell tumor arising from the
olfactory mucosa. Case Rep Med. 2012:4268532012.PubMed/NCBI
|
|
8
|
Al-Ghanem R, Ramos-Pleguezuelos FM,
Pérez-Darosa SI and Galicia-Bulnes JM: Cabrerizo-Carvajal F and
El-Rubaidi OA: Olfactory ensheathing cell tumour: case report and
literature review. Neurocirugia (Astur). 24:130–134. 2013.[(In
Spanish)]. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
van Leeuwen BM, Borst JM, Putter H, Jansen
JC, van der Mey AG and Kaptein AA: Emotional intelligence in
association with quality of life in patients recently diagnosed
with vestibular schwannoma. Otol Neurotol. 35:1650–1657. 2014.
View Article : Google Scholar : PubMed/NCBI
|