Introduction
Lung cancer is one of the most common malignancies
and the leading cause of tumor-associated mortality worldwide
(1). Non-small cell lung cancer
(NSCLC) is the most common form of lung cancer, however, its
successful treatment remains difficult as <20% of patients are
candidates for curative surgical resection when NSCLC is initially
diagnosed (2). For patients who
cannot undergo surgery or who reject surgery, chemoradiotherapy is
an alternative. The Department of Radiology at the Affiliated
Hospital of Shandong Academy of Medical Sciences (Jinan, China)
often employs combined therapy with computed tomography (CT)-guided
radioactive iodine-125 (125I) seed implantation and a
gemcitabine plus cisplatin (GP) chemotherapy regime for patients
with advanced NSCLC. Compared with conventional external-beam
radiotherapy, CT-guided 125I seed implantation can allow
the application of an increased radiation dose without damaging
organs adjacent to the target tumor; therefore, this technique is
widely used for its curative effect, minimal surgical trauma and
small number of complications (3,4).
Chemotherapy with GP is a first-line treatment
strategy for advanced NSCLC. A randomized study comparing the
efficacy and safety of chemotherapeutic agents for advanced NSCLC
indicated that treatment with GP was associated with a
significantly longer time to the progression of disease, and higher
1- and 2-year survival rates (5).
Sodium glycididazole [CMNa
(C18H22N7NaO10·3H2O)],
a newly synthesized radio- and chemotherapy sensitizer, is widely
used in China. A number of previous studies have demonstrated
positive results regarding the application of CMNa as a sensitizer
for conventional external radiation or chemotherapy alone (6–10).
Additionally, a number of studies have reported that concurrent
chemoradiotherapy combined with CMNa may enhance the response rate
and prolong the survival of patients with advanced esophageal,
nasopharyngeal or laryngeal carcinoma (8,10,11). However, to the best of our knowledge,
the effect of CMNa on CT-guided 125I seed implantation
combined with chemotherapy has yet to be described in patients with
NSCLC.
Therefore, the present study investigated the
short-term efficacy and safety of combined therapy with CT-guided
125I seed implantation and GP regimen chemotherapy, in
combination with CMNa administration, in patients with NSCLC.
Patients and methods
Study population
Between May and October 2013, 81 consecutive
patients with NSCLC from the Affiliated Hospital of Shandong
Academy of Medical Sciences (Jinan, China) were enrolled in the
present study. The inclusion criteria were as follows: i) NSCLC
confirmed by needle biopsy, fiberoptic bronchoscopy or cast-off
cell examination; ii) stage III-IV NSCLC according to the
International Union Against Cancer staging system (2009) (12); iii) ineligible for surgical resection
or rejected surgical treatment for personal reasons; iv) newly
diagnosed with cancer or had not received anti-tumor therapy within
three months of undergoing the study treatment regime; and v) liver
and kidney function, as well as routine blood and coagulation
function, within the normal ranges. Patients with uncontrolled
infection, heart failure, respiratory failure or other concomitant
serious disease contraindicating the procedure were excluded from
the present study.
Patients were randomly divided into two groups for
treatment: An experimental group and a control group. The 40
experimental patients (19 females; mean age, 52.3±11.5 years;
range, 34–74 years) received the combined therapy of CT-guided
125I seed implantation and GP regimen chemotherapy, as
well as CMNa administration, and the 41 control patients (13
females; mean age, 53.7±10.7 years; range, 38–79 years) received
the combined therapy only. The two groups did not significantly
differ in any of the baseline characteristics investigated
(Table I).
 | Table I.Baseline characteristics of
experimental and control group patients receiving therapy for non
small-cell lung cancer. |
Table I.
Baseline characteristics of
experimental and control group patients receiving therapy for non
small-cell lung cancer.
| Characteristic | Experimental group
(n=40) | Control group
(n=41) | P-value |
|---|
| Age,
yearsa | 52.3±11.5
(34–74) | 53.7±10.7
(38–79) | 0.576 |
| Tumor size,
cma | 5.2±1.1
(3.3–7.3) | 4.9±1.1
(3.2–7.2) | 0.317 |
| Gender, n |
|
| 0.146 |
| Male | 21 | 28 |
|
|
Female | 19 | 13 |
|
| Malignancy, n |
|
| 0.850 |
|
Squamous | 18 | 16 |
|
|
Adenocarcinoma | 19 | 22 |
|
|
Other | 3 | 3 |
|
| UICC TNM stage,
n |
|
| 0.241 |
| III | 30 | 35 |
| IV | 10 | 6 |
The present study was approved by the Institutional
Ethics Committee of the Affiliated Hospital of Shandong Academy of
Medical Sciences. Written informed consent was obtained from each
patient following a full explanation of the nature of the current
protocols.
125I seed implantation
Within 1 week prior to treatment, a baseline
thoracic CT scan (SOMATOM Sensation 64; Siemens Healthcare,
Erlangen, Germany) was performed on all patients. The CT images
(120 kV, 250 mA, 300-mm field of view and 5-mm slice thickness)
were imported to the Fudan Brachytherapy Treatment Planning
Computer System v1.0 (Fudan University, Shanghai, China) to create
an individual treatment strategy for each patient. The gross tumor
volume (GTV) was outlined and the planning treatment volume (PTV)
included the entire GTV with 0.5–1.0-cm margins. The primary
planning goal was adequate PTV coverage with the prescribed
radiation dose; therefore, a dose of 100–140 Gy was prescribed
according to the location of each tumor. The system automatically
calculated the expected number of 125I seeds (Shanghai
Xinke Medical Company Co., Ltd., Shanghai, China) required and
optimized their spatial distribution. The physician adjusted the
number of seeds and their locations based on the isodose curves to
achieve optimal dose conformity and safety. The 125I
seeds (Xinke Medical Company Co., Ltd., Shanghai, China) were 4.5
mm long and 0.8 mm thick, with a half-life of 59.6 days, a
penetration depth of 17 mm, an incipient rate of 7 cGy/h and
activity of 0.5–0.8 mCi.
All interventional procedures were performed in a
standard CT room using a CT scanner. Following ≥6 h of fasting, the
patient was placed in the supine, prone or lateral position,
according to the position of the tumor, and was trained to ensure
steady breathing during the procedure. The pathway through which
the implantation needles reached the tumor was determined on the CT
image, avoiding critical structures, such as vital blood vessels,
major bronchi, the esophagus or the spinal cord. Subsequently, one
or more 18-gauge needles were inserted percutaneously into the
tumor with the patient under local anesthesia. A repeat CT scan
facilitated the adjustment of the depth and angle of needle
direction. Adjacent implantation needles were separated by ∼1 cm. A
turntable implantation gun (Xinke Medical Company Co., Ltd.) was
loaded, and 2–5 125I seeds were released along the path
at ∼1-cm intervals when the needle was withdrawn. The distance
between the 125I seeds and the boundary of the lesion
was maintained at 0.5–1.0 cm, and the 125I seeds
remained ≥1 cm away from the aforementioned critical structures.
The needles were removed only when all the seeds had been inserted
in the correct position. The mean number of 125I seeds
implanted in each patient was 41.7±11.5 (range, 20–74
125I seeds) and 42.2±8.0 (range, 27–55) seeds for the
experimental and control patients, respectively. CMNa and the first
cycle of GP were administered 5–7 days after the interventional
procedure in patients exhibiting no implantation-associated
complications.
Chemotherapy
Two cycles of chemotherapy consisting of gemcitabine
(1,000 mg/m2 on days 1 and 8) and cisplatin (30
mg/m2 on days 1, 2 and 3) were administered
intravenously to each patient 5–7 days after 125I seed
implantation. Each treatment cycle lasted 3 weeks. All patients
received prophylactic agents consisting of the 5-HT3 antagonist
metoclopramide, berbamine and dexamethasone. Supportive care,
including the administration of antibiotics or analgesics, was
provided if considered appropriate by the investigators. Adverse
events were treated symptomatically and all chemotherapy was
performed successfully.
CMNa administration
Between 5 and 7 days after 125I seed
implantation, CMNa (LifeTech Pharmaceutical Ltd., Guangzhou,
Guangdong, China) was administered to each patient in the
experimental group. The method and dose were identical to that used
with external beam radiotherapy, as follows: CMNa (800
mg/m2 dissolved in 100 ml physiological saline)
administered intravenously within 30 min, three times a week (on
alternate days) for 8 weeks.
Follow-up and evaluation
All patients were followed up for 3–8 months (mean,
5.4±1.6 months). Within 1 week prior to treatment, all patients
underwent a baseline thoracic CT. Follow-up CT examinations were
performed monthly in the first 3 months and subsequently at 2-month
intervals. The short-term curative effects were graded according to
the Response Evaluation Criteria in Solid Tumors (13) as follows: Complete response (CR) was
defined as the disappearance of all target lesions; partial response
(PR) was defined as a ≥30% decrease in the sum of the longest
diameters of the target lesions; stable disease (SD) was defined as
a <30% reduction or <20% increase in the sum of the longest
diameters of the target lesions; and progressive disease (PD) was
defined as a ≥20% increase in tumor load or the development of new
lesions in a previously uninvolved site. Furthermore, response rate
was defined as the sum of CR and PR. Following implantation, liver
and kidney function tests, routine blood tests and
electrocardiography (ECG) were performed every 2 weeks in the first
3 months, or as indicated. Complications associated with the
implantation procedure and brachytherapy were investigated. In
addition, adverse events (grades 1 to 5) associated with
chemotherapy or CMNa were evaluated according to the Common
Terminology Criteria for Adverse Events (version 4.0) (14) of the US National Cancer Institute.
Statistical analysis
All numerical data were expressed as the mean ±
standard deviation and determined by performing independent-samples
t-tests between the two groups. Categorical variables at baseline
and clinical efficacy were compared using the χ2 test,
and adverse effects were evaluated by performing a χ2 or
Wilcoxon rank test. All significance tests were two-tailed, and
P<0.05 were considered to indicate a statistically significant
difference. Data processing and analysis involved the use of SPSS
software (version 15.0; SPSS Inc., Chicago, IL, USA).
Results
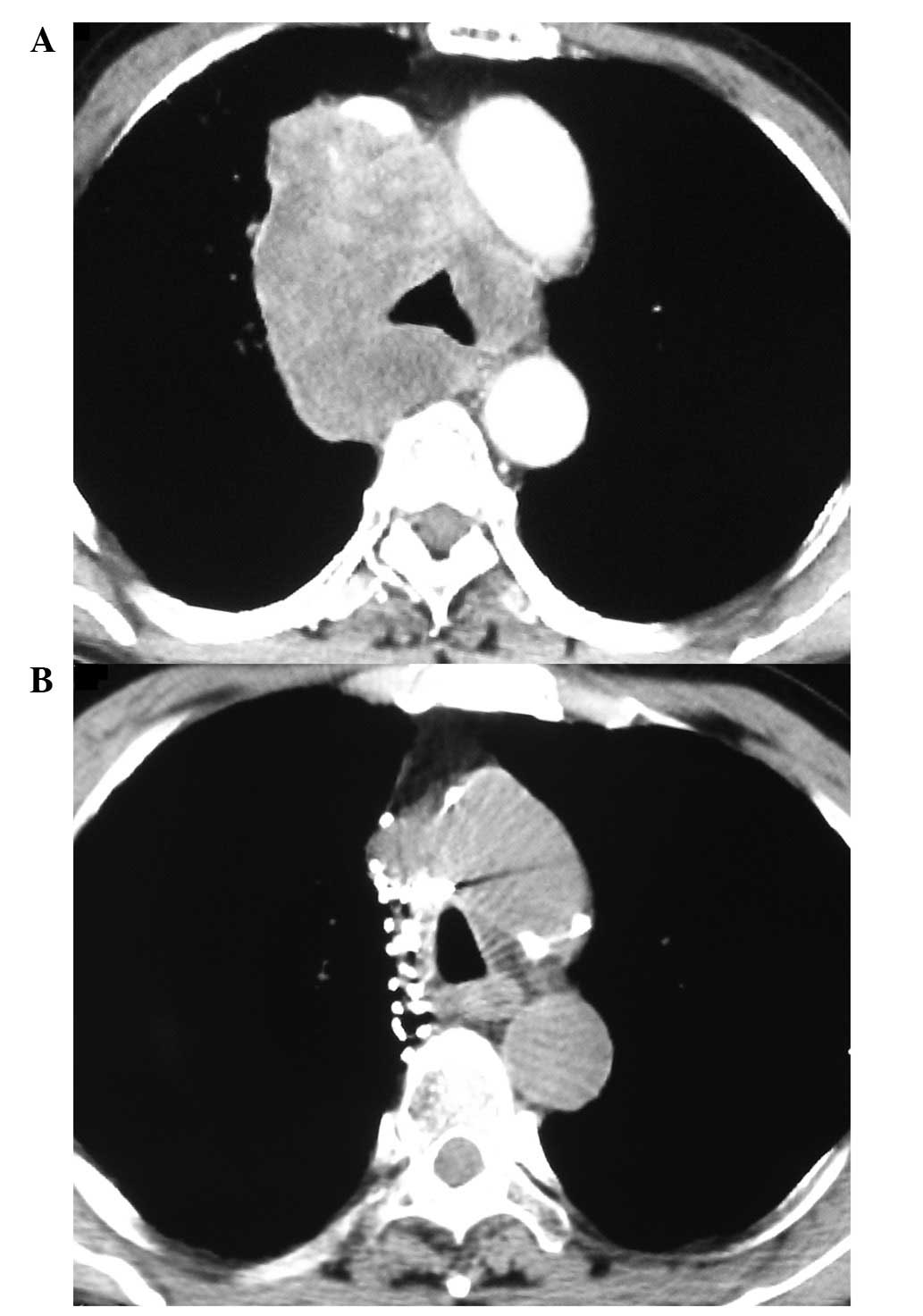
CR, PR, SD and PD were observed in 8, 26, 5 and 1
experimental patients, respectively, and 6, 20, 9 and 6 control
patients, respectively (Fig. 1). The
response rates (sum of CR and PR) were 85.5 and 63.4% for the
experimental and control groups, respectively (P=0.027).
A pneumothorax developed in 17 experimental patients
(42.5%) and 14 control patients (34.1%) during the procedures;
therefore, 6 (15.0%) and 7 (17.1%) patients, respectively,
underwent puncture aspiration or closed thoracic drainage for 1–2
days to relieve the complication. The remaining patients exhibited
no apparent symptoms and therefore received no treatment, as the
pneumothorax was mild. At 3 days post-treatment, all patients
demonstrated complete regression of the pneumothorax. Furthermore,
5 (12.5%) and 9 (22.0%) experimental and control patients,
respectively, demonstrated hemoptysis or focal hemorrhage, as
detected by CT. The two groups did not significantly differ in the
rate of pneumothorax and hemoptysis or focal hemorrhage (P=0.439
and P=0.261, respectively). No lethal hemoptysis or hemorrhage
occurred, and no 125I seeds migrated to other tissues or
organs. Additionally, no patients appeared to exhibit radiation
pneumonia or radiation esophagitis.
Thus, the two groups did not significantly differ in
the occurrence of adverse events associated with chemotherapy or
CMNa (Table II). Adverse events of
grade 3 were treated using routine clinical methodology. No adverse
events of grade 4 or above were identified; therefore, chemotherapy
was not delayed or canceled in any of the cases.
 | Table II.Adverse events observed in the
experimental and control groups upon follow-up. |
Table II.
Adverse events observed in the
experimental and control groups upon follow-up.
|
|
Grade |
|
|---|
|
|
|
|
|---|
|
| Experimental group
(n=40) | Control group
(n=41) |
|
|---|
|
|
|
|
|
|---|
| Adverse event | 0 | 1 | 2 | 3 | 4 | 5 | 0 | 1 | 2 | 3 | 4 | 5 | P-value |
|---|
| White blood cell
decrease | 20 | 10 | 8 | 2 | 0 | 0 | 24 | 8 | 7 | 2 | 0 | 0 | 0.505 |
| Platelet count
decrease | 19 | 9 | 9 | 3 | 0 | 0 | 20 | 11 | 8 | 2 | 0 | 0 | 0.726 |
| Alanine
aminotransferase increase | 17 | 14 | 5 | 4 | 0 | 0 | 20 | 13 | 6 | 2 | 0 | 0 | 0.536 |
| Creatinine
increase | 21 | 9 | 8 | 2 | 0 | 0 | 25 | 10 | 4 | 2 | 0 | 0 | 0.350 |
| Vomiting | 13 | 17 | 8 | 2 | 0 | 0 | 15 | 15 | 10 | 1 | 0 | 0 | 0.833 |
| Palpitations | 32 | 5 | 3 | 0 | 0 | 0 | 36 | 4 | 1 | 0 | 0 | 0 | 0.318 |
| Sinus
tachycardia | 31 | 6 | 2 | 1 | 0 | 0 | 35 | 3 | 3 | 0 | 0 | 0 | 0.390 |
Discussion
The present study evaluated the short-term efficacy
and safety of combined therapy with CT-guided radioactive
125I seed implantation and GP regimen chemotherapy, as
well as CMNa administration, in patients with advanced NSCLC. This
treatment strategy produced greater efficacy compared with the
control treatment of combined therapy alone, and the two groups did
not significantly differ in the rate of adverse events.
Interstitial permanent brachytherapy is based on the
implantation of radioactive sources inside or close to the tumor
target, thereby delivering high-dose radiation directly to the
tumor, while sparing the surrounding healthy tissues, as a sharp
dose drop-off occurs outside of the implanted target area. Thus,
percutaneous CT-guided 125I seed implantation has become
a treatment focus due to its ability to increase the possible
radiation dose to tumors without damage to neighboring organs
(15). Using this method, highly
effective radiation doses can be applied as a single fraction.
Compared with fractionated external radiotherapy, which is
effective only to tumor cells in specific phases of the cell cycle,
the 125I seed continuously generates a low level of
radiation sufficient to kill the tumor cells or cause them to lose
the ability to reproduce, thus providing protracted cell killing
for up to several weeks or months (16). Additionally, by providing continuous
low-dose radiation, 125I seeds may decrease the oxygen
enhancement ratio, thus improving efficacy in hypoxic regions of the
tumor (17). Previous studies
investigating this strategy for the treatment of liver cancer and
other malignancies demonstrated that 125I brachytherapy
is safe and may provide long-term local control and increased
survival (4,18).
GP is a standard chemotherapeutic regimen for the
first-line treatment of advanced NSCLC. Chemotherapy with GP may
result in a higher overall survival rate for patients with advanced
NSCLC when compared with other cisplatin-based regimens (19). A randomized study comparing the
efficacy and safety of various chemotherapy agents for advanced
NSCLC indicated that treatment with GP was associated with a
significantly longer time to the progression of disease, and higher
1- and 2-year survival rates (5).
The treatment of advanced NSCLC is based on local
and systemic control of the disease (20). CT-guided 125I seed
implantation may improve the local control rate (21), and chemotherapy potentially exhibits
an effect on distant metastasis (22). Therefore, the combination of
brachytherapy and chemotherapy is considered to be superior to
either alone.
CMNa, a novel nitroimidazole compound, is the first
hypoxic sensitizer synthesized in China and is widely used
(6–9).
The mechanism of CMNa involves the selective potentiation of DNA
duplex damage caused by chemoradiotherapy in hypoxic cells, and the
inhibition of DNA polymerase B activity to inhibit the recovery of
potentially lethal and sub-lethal cellular damage. Previous studies
have demonstrated that CMNa exhibits an overt radiation-enhancing
effect in vitro and in vivo (6–9,23,24). In
addition, a number of studies have indicated that CMNa may enhance
the chemosensitivity of specific chemotherapeutic agents (25,26). In
the present study, the efficacy of 125I seed
implantation combined with GP regimen chemotherapy and CMNa
administration was significantly improved in the experimental group
compared with the control group. Thus, CMNa may enhance the
therapeutic effect of 125I seed implantation combined
with GP regimen chemotherapy for the treatment of patients with
NSCLC.
The two groups experienced no serious complications.
In previous studies (27,28), pneumothorax and hemoptysis were the
predominant complications of 125I seed implantation.
However, in the present study, the two groups did not significantly
differ in the rates of pneumothorax and hemoptysis or focal
hemorrhage, and all patients were successfully treated using
appropriate therapies. Furthermore, no lethal hemoptysis occurred
and no 125I seeds migrated to other tissues or organs.
Due to a sharp dose drop-off outside of the implanted target area,
125I seed implantation delivers a low dose of radiation
to the healthy tissues surrounding the tumor; therefore, it does
not typically result in serious complications (29). No patients in the current study
appeared to exhibit radiation pneumonia, radiation esophagitis or
other radiation-association complications upon follow-up. Thus, the
safety of GP chemotherapy alone or combined with CMNa was
considered to be acceptable. As in previous studies, the most
common adverse reactions associated with CMNa in the present study
were mild gastrointestinal duct reactions, including nausea,
vomiting and constipation; mild reversible increases in alanine
aminotransferase and bilirubin expression levels; and varying
degrees of change in cardiac function and ECG results upon
treatment with large doses of CMNa (7,30,31). In the current study, the use of CMNa
did not significantly increase the occurrence of adverse events
associated with chemotherapy in the experimental group compared
with the control group.
Various factors affected the results of the present
study. First, the heterogeneity of radiation distribution. Despite
the assistance of the TPS, the positioning of all seeds in
accurately remains difficult due to the complexity of the
implantation procedure. Furthermore, the prescribed dose (seed
number) varied depending on the location of the tumor. For example,
in patients with NSCLC close to critical structures, such as vital
blood vessels, the major bronchi, the esophagus and the spinal
cord, a low radiation dose was prescribed. The 125I
seeds are positioned ≥1 cm away from these critical structures due
to the concern of possible complications, such as hemorrhage and
bronchial injury. Therefore, regions of insufficient dose or cold
spots remain in specific lesions. The heterogeneity of radiation
distribution and the variety of prescribed doses affected the
response of the tumor or in specific cases resulted in local
relapse.
The second factor affecting the results of the
present study was the method used to administer CMNa. CMNa was
administered according to the clinical practice used with external
beam radiotherapy. However, as opposed to conventional fractionated
radiotherapy, 125I seed implantation continuously
generates a low level of radiation and provides protracted cell
killing over a relatively long period of time. Thus, the optimal
dose and method of administering CMNa requires additional
investigation. The third factor was the interaction between CMNa
and chemotherapeutic agents. These interactions also require
further investigation, in particular, whether CMNa increases the
toxicity of specific chemotherapeutic agents. The final affecting
factors were the small sample size and the short follow-up
time.
In conclusion, despite the aforementioned
limitations, the preliminary results of the current study indicate
that CMNa may enhance the short-term efficacy of combined therapy
with 125I seed implantation and GP regimen chemotherapy
for NSCLC. This strategy appears to be safe and effective for the
treatment of patients with NSCLC. However, additional studies with
larger samples and a longer follow-up period are required to
validate the findings of the present study.
Acknowledgements
The authors would like to thank Dr. Yue Ren of the
Department of Radiology at the Affiliated Hospital of Shandong
Academy of Medical Sciences for providing assistance in performing
the present study.
References
|
1
|
Devesa SS, Bray F, Vizcaino AP and Parkin
DM: International lung cancer trends by histologic type:
male:female differences diminishing and adenocarcinoma rates
rising. Int J Cancer. 117:294–299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cardona AF, Reveiz L, Ospina EG, et al:
Palliative endobronchial brachytherapy for non-small cell lung
cancer. Cochrane Database Syst Rev. CD004284:2008. View Article : Google Scholar
|
|
3
|
Ebara S, Katayama N, Tanimoto R, et al:
Iodine-125 seed implantation (permanent brachytherapy) for
clinically localized prostate cancer. Acta Med Okayama. 62:9–13.
2008.PubMed/NCBI
|
|
4
|
Nag S, DeHaan M, Scruggs G, Mayr N and
Martin EW: Long-term follow-up of patients of intrahepatic
malignancies treated with iodine-125 brachytherapy. Int J Radiat
Oncol Biol Phys. 64:736–744. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schiller JH, Harrington D, Belani CP, et
al: Comparison of four chemotherapy regimens for advanced
non-small-cell lung cancer. N Engl J Med. 346:92–98. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shen G and Bao Y: Sodium Glycididazole
Clinical Trial Cooperative Group: Double blind randomized clinical
trail phase II on the sensitization by sodium glycididazole
injection. Chin J Radiat Oncol. 12:254–258. 2003.(In Chinese).
View Article : Google Scholar
|
|
7
|
Wang XP, Yun S, Zhang XL and Ding W:
Primary clinical study of radiosensitizer CMNa. Chin Clin Oncol.
8:28–32. 2003.(In Chinese).
|
|
8
|
Zeng YC, Wu R, Xu ZG, et al: Safety and
radiation-enhancing effect of sodium glycididazole in
locoregionally advanced laryngeal cancers previously treated with
platinum-containing chemotherapy regimens: A preliminary report.
Cancer Radiother. 14:59–64. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu MZ, He LR, Lu TX, et al: Effect of
hypoxic radiosensitizer sodium glycididazole on long-term result of
radiotherapy for nasopharyngeal carcinoma. Chin J Oncol.
28:932–937. 2006.(In Chinese).
|
|
10
|
Yang J, Liu MZ, Cai L, et al: Phase II
clinical trial of sodium glyci-didazole (CM-Na) combined with
concurrent radiochemotherapy for advanced esophageal carcinoma.
Chin J Cancer. 622–626. 2008.(In Chinese).
|
|
11
|
He ZY, Li FY, Tong Q, Liao ZW, Guan XX and
Wang W: Concurrent chemoradiotherapy with sodium glycididazole and
cisplatin for local advanced nasopharyngeal carcinoma. J First Mil
Med Univ. 28:2038–2040. 2008.(In Chinese).
|
|
12
|
International Union Against Cancer (UICC):
Lung and Pleural TumoursTNM Classification of Malignant Tumours.
Sobin LH, Gospodarowicz MK and Wittekind C: 7th. Wiley-Blackwell;
New York, NY: pp. 99–106. 2009
|
|
13
|
Eisenhauer EA, Therasse P, Bogaerts J, et
al: New response evaluation criteria in solid tumours: revised
RECIST guideline (version 1.1). Eur J Cancer. 45:228–247. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
National Cancer Institute, . Common
Terminology Criteria for Adverse Events (CTCAE) version 4.0.
Accessed. June 14–2010.
|
|
15
|
Hu XK, Wang MY, Yang ZG, et al: The study
of curing central-type lung cancer by CT guided percutaneous
embedding of 125I seeds. Chin J Radiol. 38:910–915. 2004.(In
Chinese).
|
|
16
|
Ling CC: Permanent implants using Au-198,
Pd-103 and I-125: radiobiological considerations based on the
linear quadratic model. Int J Radiat Oncol Biol Phys. 23:81–87.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Blasko JC, Mate T, Sylvester JE, Grimm PD
and Cavanagh W: Brachytherapy for carcinoma of the prostate:
techniques, patient selection and clinical outcomes. Semin Radiat
Oncol. 12:81–94. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Henry AM, Al-Qaisieh B, Gould K, et al:
Outcomes following iodine-125 monotherapy for localized prostate
cancer: the results of Leeds 10-year single-center brachytherapy
experience. Int J Radiat Oncol Biol Phys. 76:50–56. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kubota K, Nishiwaki Y, Ohashi Y, et al:
The Four-Arm Cooperative Study (FACS) for advanced non-small cell
lung cancer (NSCLC). J Clin Oncol (Meeting Abstracts). 22
(Suppl):70062004.
|
|
20
|
Vokes EE, Choy H, Gandara D and Mattson K:
Adjuvant and neoadjuvant treatments for NSCLC. Lung Cancer. 38
(Suppl 4):29–35. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen A, Galloway M, Landreneau R, et al:
Intraoperative 125I brachytherapy for high-risk stage I non-small
cell lung carcinoma. Int J Radiat Oncol Biol Phys. 44:1057–1063.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Depierre A, Milleron B, Moro-Sibilot D, et
al: French Thoracic Cooperative Group: Preoperative chemotherapy
followed by surgery compared with primary surgery in resectable
stage I (except T1N0), II, and IIIa non-small-cell lung cancer. J
Clin Oncol. 20:247–253. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zheng X, Meng X, Zhao F, LI Y and GAO J:
The in situ tumor response to radiosensitization of a novel
sensitizer sodium glycididazole. J Radiat Res Radiat Process.
18:91–95. 2000.(In Chinese).
|
|
24
|
Zhang X, Ji HB, Chen ZH, OuYang XN and
Yang RJ: Lung cancer radiosensitization by CMNa in vitro and in
vivo. Chin J Radiol Med and Prot. 25:316–318. 2005.(In
Chinese).
|
|
25
|
Lei KJ, Wang J, Jia YM and Cao YY:
Chemo-sensitivity-enhancing effects of low dose glycididazolum
natrium on patients with advanced non-small cell lung cancer during
intervention. Chinese-German J Clin Oncol. 9:385–387. 2010.(In
Chinese). View Article : Google Scholar
|
|
26
|
Lei KJ, Jia YM, Wang J and Du YP: Effects
of CMNa combined with paclitaxel and carboplatin on elevated CA12-5
levels in post-operation advanced ovarian cancer patients.
Chinese-German J Clin Oncol. 7:600–602. 2008.(In Chinese).
View Article : Google Scholar
|
|
27
|
Brach B, Buhler C, Hayman MH, Joyner LR Jr
and Liprie SF: Percutaneous computed tomography-guided fine needle
brachytherapy of pulmonary malignancies. Chest. 106:268–274. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Martinez-Monge R, Pagola M, Vivas I and
Lopez-Picazo JM: CT-guided permanent brachytherapy for patients
with medically inoperable early-stage non-small cell lung cancer
(NSCLC). Lung Cancer. 61:209–213. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lewis JW Jr, Ajlouni M, Kvale PA, et al:
Role of brachytherapy in the management of pulmonary and
mediastinal malignancies. Ann Thorac Surg. 49:728–733. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fu LQ, Huang F, Guo JH, et al: Phase I
clinical pharmacokinetics of glycididazolum natrium. Chin J Pharm
Toxicol. 18:87–92. 2004.(In Chinese).
|
|
31
|
Gao HJ, Shen G, Wang HM, et al: Phase I
clinical trail of sodium glycididadole (CMNa) in cancer patients.
Chin J New Drugs. 13:260–263. 2004.(In Chinese).
|