Introduction
Oral squamous cell carcinoma (SCC) is the most
commonly identified cancer of the oral cavity and the head and neck
region. More than 90% of the tumors occurring in the head and neck
region are SCCs; these can grow in several locations of the mucosal
lining, with relatively rare neoplasms arising in the minor
salivary glands and soft tissues (1,2).
Lymphatic metastasis is the most significant
predictive factor for the survival of patients with oral SCC.
Moreover, patients who suffer from recurrence of neck cancer, after
initial treatment, frequently die due to uncontrolled neck disease
and many other evaluated potential prognostic factors (3).
The vascular endothelial growth factor (VEGF) family
including VEGF-A, VEGF-B, VEGF-C, VEGF-D, VEGF-E, and placental
growth factor (PlGF), each acting through their respective VEGF
tyrosine kinase receptors (VEGFR-1, VEGFR-2, and VEGFR-3), play
significant roles in angiogenesis and lymphangiogenesis (4). Many studies have reported that the
overexpression of VEGF-C or VEGF-D, acting through the tyrosine
kinase receptor VEGF receptor-3 (VEGFR-3), promotes the process of
lymph node (LN) metastasis through the regulation of cancer
lymphangiogenesis (5). Moreover,
VEGF-C and VEGF-D are associated with LN metastasis through
intratumoral and peritumoral lymphatics in many types of cancers,
including esophageal, gastric, colon, breast, thyroid, pancreas,
prostate, and lung cancers (6).
Small pro-inflammatory ʻchemotactic cytokinesʼ are
secreted proteins that are involved in the migration of activated
hematopoietic cells (dendritic cells) to regional LNs (7). The chemokine superfamily is generally
classified into four groups based on the cysteine motifs in the
protein (CXC, CC, CX3C, and C), and the involvement of these
proteins in tumor metastasis has been determined (8). Recently, several studies have shown
that C-C motif chemokine receptor 7 (CCR7) plays an important role
in the metastasis of head and neck SCC, esophageal carcinoma,
gastric carcinoma, breast cancer, malignant melanoma, non-small
cell lung carcinoma, and gastrointestinal carcinoma (9).
Neuropilin (NRP)1 and NRP2 are transmembrane
glycoprotein receptors with roles in neuronal guidance,
angiogenesis, and lymphangiogenesis via VEGF binding and signaling
in the absence of other VEGF receptors (10). In addition, both are structural
receptors of the class 3 semaphorins (11). Several studies have reported their
expression and regulation in tumor cells of human breast, colon,
and prostate cancers (7). NRP
expression may be a prospective biomarker, and further studies may
eventually lead to more efficacious treatments (7).
Semaphorin 3E (SEMA3E) is a secreted protein
involved in axonal guidance and angiogenesis (12). There are eight groups of
semaphorins, which bind to the cell surface receptors NRPs (NRP1
and NRP2) (13) as well as
plexin-D1 for their signaling pathways (11). Casazza et al and other
studies have reported that secreted SEMA3E and its receptor
plexin-D1 inhibit tumor growth but promote the metastasis and
invasiveness of cancer cells (14).
They are involved in the metastasis of colon, liver, melanoma, and
breast cancers; however, the mechanism remains unclear (13–15).
Although the predictive value of these biomarkers is
yet to be established, it has been observed that lymphangiogenesis
in cancer is not limited to the areas within or immediately
adjacent to a primary tumor; however, it can also occur in the
sentinel LNs (16,17). The identification of effective and
innovative therapies that appear to influence cancer metastasis is
critical for the improvement of SCC therapy.
Therefore, the present study aimed to evaluate the
expression levels of the following growth factors and receptors in
SCC of the tongue: VEGF-C, VEGF-D, VEGFR-3, CCR7, NRP1, NRP2, and
SEMA3E. In order to demonstrate the prognostic value of these
proteins, we analyzed the correlation between them and the overall
or disease-free survival. Furthermore, we assessed the correlation
between microvessel density (MVD) and LN metastasis as well as the
correlation between lymphatic vessel density (LVD) and LN
metastasis, with respect to their clinicopathological features.
Materials and methods
Patients and tissues
All clinical studies were approved by the Ethics
Committee of Osaka University Dental Hospital. We conducted a
retrospective cohort study by randomly selecting 80 patients who
had been previously diagnosed with primary tongue SCC and undergone
curative tumor resection at the First Department of Oral and
Maxillofacial Surgery, Osaka University Dental Hospital (Osaka,
Japan) between 1995 and 2008.
Information regarding the clinicopathological
features of each case (including age, gender, tumor size, nodal
status, and the location and status of recurrence or metastasis)
was obtained from the patient histories. The study included 55 men
(68.75%) and 25 women (31.25%) between the ages of 22 and 92 years,
with a median age of 62 years. Forty (50%) of the patients had LN
metastasis.
All patients were staged according to the 2010 Japan
Society for Oral Tumors TNM Classification of Malignant Tumors
(18). The histological mode of
invasion was classified according to the YK classification
(19,20).
Immunohistochemistry
The paraffin sections were fixed in 10% neutral
buffered formalin. Sections of 5-µm thickness were cut
consecutively, deparaffinized in xylene, rehydrated with graded
concentrations of ethanol, and treated with citrate buffer, pH 6.0,
at 98°C for 30 min and EDTA buffer, pH 8.0, at 98°C for 15 min for
heat-induced antigen retrieval. These sections were then used in
histopathological and immunohistochemical analysis. To block
endogenous peroxide activity, 0.3%
H2O2·dH2O was applied to the
sections. Non-specific reactions were blocked with 1% bovine serum
albumin buffer [Histofine SAB-PO (Multi) kit; Nichirei Bioscience,
Tokyo, Japan]. The sections were incubated with the following
primary antibodies at 4°C, overnight: anti-human rabbit polyclonal
VEGF-C antibody (dilution 1:100), anti-human rabbit polyclonal
VEGF-D antibody (dilution 1:200) (both from Abcam, Tokyo, Japan),
anti-human mouse 9D9F9 VEGFR-3 antibody (dilution 1:500; Millipore
Corp., Billerica, MA, USA), anti-human goat polyclonal CCR7
antibody (dilution 1:250), anti-human rabbit monoclonal NRP1
antibody (dilution 1:100) (both from Abcam), anti-human rabbit
polyclonal NRP2 antibody (dilution 1:100; Atlas Antibodies,
Stockholm, Sweden), anti-human goat polyclonal SEMA3E antibody
(dilution 1:100; Abcam), anti-human mouse monoclonal CD-34 antibody
(dilution 1:100), and anti-human mouse monoclonal D2-40 antibody
(pre-diluted) (both from Nichirei Bioscience). Next, the
appropriate secondary antibodies and blocking agents were applied
using the Histofine SAB-PO (Multi or Goat) kit (Nichirei
Bioscience). Immunostaining and immunolocalization of the proteins
were performed using the DAB-Peroxidase Substrate Solution
Immunohistochemistry brown Histofine SAB-PO (Multi) kit (Nichirei
Bioscience), according to the manufacturer's instructions. The
sections were counterstained with Mayer's hematoxylin solution
(Sigma-Aldrich, St. Louis, MO, USA) dehydrated with graded
concentrations of ethanol, cleared with xylene, and mounted for
visualization using bright-field microscopy.
A positive control (immunohistochemical staining
demonstrating weakly positive tissue) and negative controls
(immunohistochemical staining with the omission of the primary
antibody) were included in the staining protocol. Scoring and cell
counts were performed without prior clinical knowledge of the
patients.
Staining evaluation
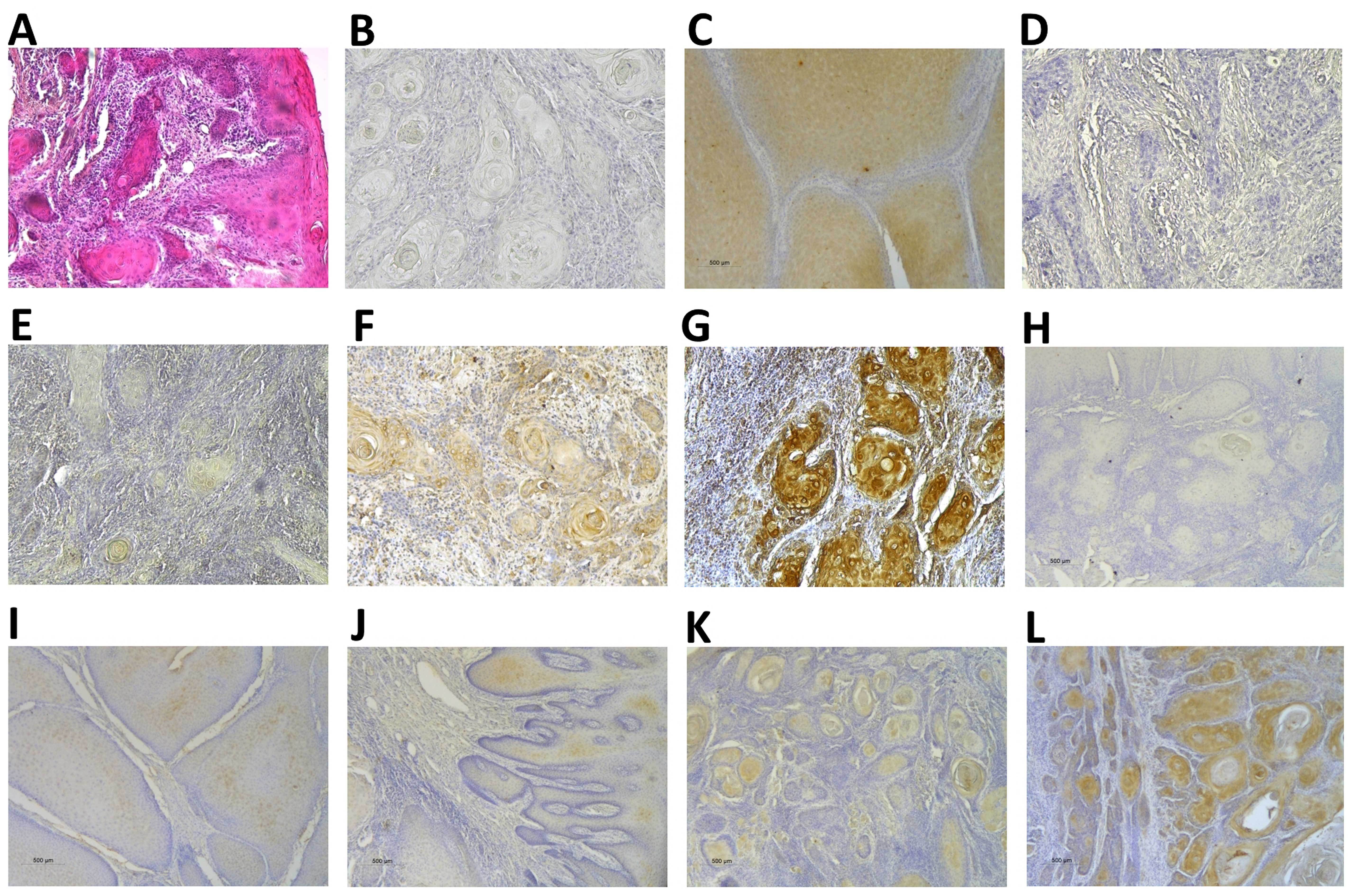
The immunohistochemical staining of these proteins
in SCC cells was evaluated based on the ratio and intensity of the
staining. Specimens were considered immunopositive when ≥1% of the
cancer cells showed clear evidence of immunostaining. The ratio of
staining for each specimen was determined as follows: specimens
with no positive tumor cells, score of 0; 1–25% positive cells,
score of 1; 26–50% positive cells, score of 2; 51–75% positive
cells, score of 3; and 76–100% positive cells, score of 4. The
intensity of immunostaining was determined as follows: specimens
with no staining, score of 0; weak staining, score of 1; moderate
staining, score of 2; and intense staining, score of 3 (21–23)
(Fig. 1). The tumors in this study
were sometimes heterogeneous and the staining was therefore
calculated by multiplying the ratio score with the intensity score
to give an overall staining score between 1 and 12, using a similar
rationale to the immunoreactivity score (IRS) first described by
Remmele and Stegner (24).
Using this scoring system, each component of the
tumor was scored independently, and the results were calculated.
The immunostaining of the specimens was evaluated independently by
two authors (Dr Al-Shareef Hani and Dr Yosuke Shogen), who were
blinded to patient results and other clinicopathological features,
and their scores were averaged to obtain a final IRS. Subsequently,
patients were divided into low and high expression groups, with the
mean IRS for each protein serving as the cut-off value (21–23).
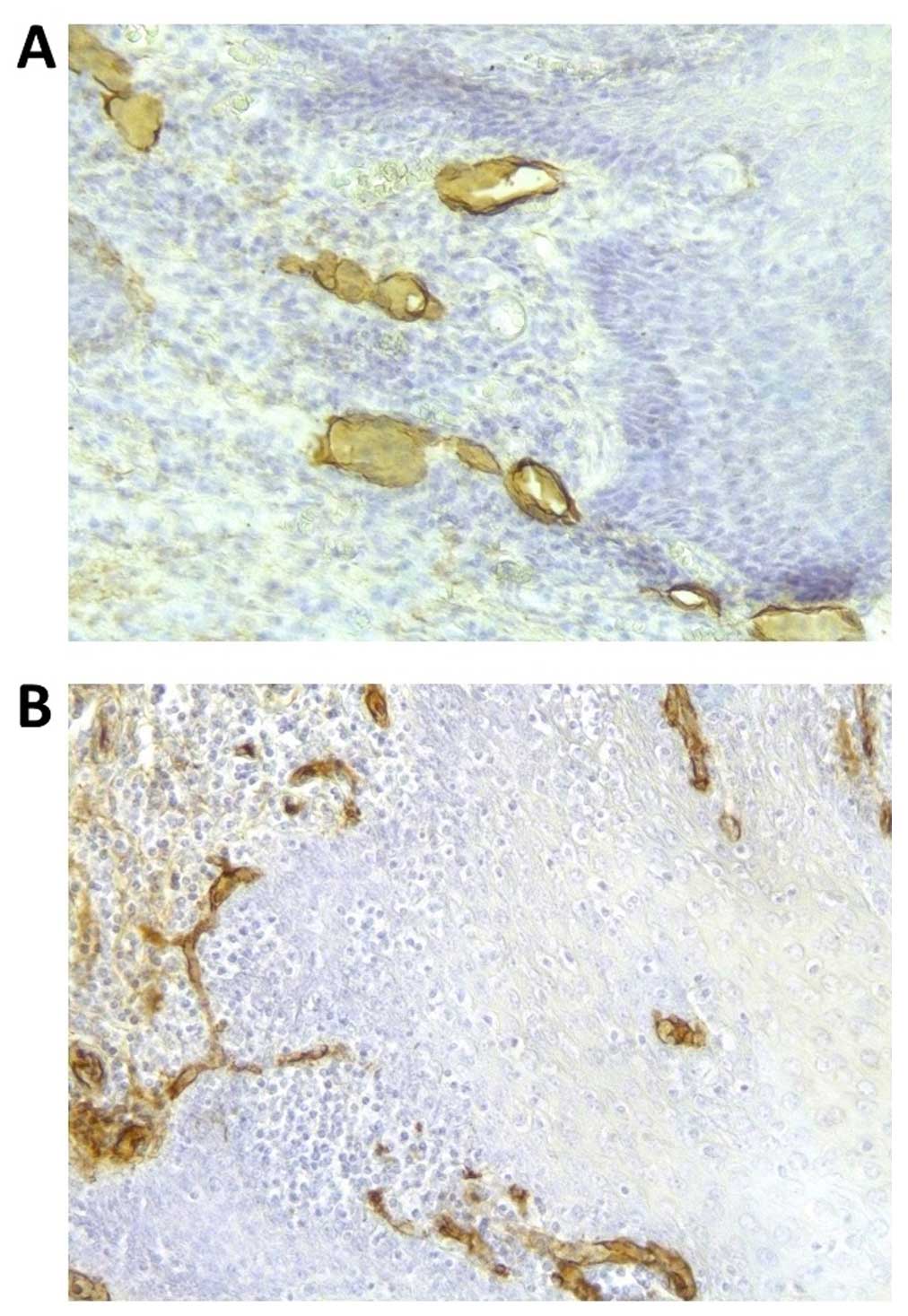
Assessment of MVD and LVD
MVD and LVD were estimated in tumor vessel ʻhot
spotsʼ by immunostaining with the CD-34 and D2-40 podoplanin
antibodies, respectively. Microvessel counts were assessed by light
microscopy in areas of the tumor with the highest number of
capillaries and small venules at the invasive edge, that is, in the
areas with the most intense neovascularization. Although SCCs have
a mostly heterogeneous MVD and LVD, areas of highly invasive
carcinoma were identified by the presence of a higher number of
discrete microvessels and lymphatic vessels that were positively
stained for CD-34 and D2-40, respectively. These areas of increased
neovascularization could occur anywhere in the invasive tumor;
however, they were most frequently observed in the intratumoral
region and at the margins of the carcinoma (3,25).
Microvessels and lymphatic vessels with positive
immunostaining for CD-34 and D2-40, respectively, were counted in
three hotspots per section, using a 20× objective lens, by two
authors (Dr Al-Shareef Hani and Dr Sanam Bakhshishayan), who were
blinded to patient results and other clinicopathological features.
The mean vessel counts in each of the three hotspots were recorded
and each component of the tumor was scored independently to give
six hotspot scores for each specimen. After averaging the three
hotspot scores of each component, to obtain a final hotspot score
for LVD and MVD, the specimens were divided into two groups (low or
high) based on the mean values for LVD and MVD (6.85 and 20.31
number of vessels/µm2 of tumor-free area,
respectively). In brief, the area with the highest vascular density
(hotspot) was selected, and the number of microvessels was
determined in each of the three microscopic fields by each
investigator using the 20× objective lens. The total lymphatic
vessel count was compared between the groups according to age,
gender, primary tumor site, clinical stage, tumor size, grade, and
the status of the lymphatic metastasis.
Statistical analysis
Statistical analysis was performed using the
statistical software IBM SPSS Advanced Statistics 20.0 (IBM Corp.,
Armonk, NY, USA). Subjects were grouped into the following
categories: <60 or ≥60 years of age; pathological negative (N0)
or pathological positive (N1) for LN metastasis; and high or low
protein expression based on the individual cut-off score for each
protein. Chi-square and Fisher's exact tests were performed to
assess the association between clinicopathological features and
protein expression levels. An independent samples t-test was
performed to determine the association between protein expression
levels and LN metastasis. In addition, an independent samples
t-test was performed to assess the relationship between LVD or MVD
and LN metastasis or protein expression.
Univariate and multivariate logistic regression
analyses were performed to assess the association between LN
metastasis and clinicopathological features or protein expression
as well as to assess the odds ratio (OR), and to define independent
risk factors for prognosis and incidence of nodal recurrence. The
overall and disease-free survival rates were estimated using the
Kaplan-Meier method and analyzed using the log-rank test. For all
tests, p<0.05 was accepted as statistically significant.
Results
MVD, LVD, and the expression of
angiogenic and lymphangiogenic biomarkers in oral SCC
The biomarkers for LN metastasis were analyzed
individually. The expression levels of VEGF-C, VEGF-D, VEGFR-3,
CCR7, NRP1, NRP2, and SEMA3E in oral SCC lesions were assessed by
immunohistochemistry. We found that these biomarkers were
predominantly expressed in the cell layer and the cytoplasm of the
SCC cells, especially at the invasive edges, and were occasionally
observed in endothelial cells in the stroma around or close to
carcinoma nests and tumor vessels (Fig.
1).
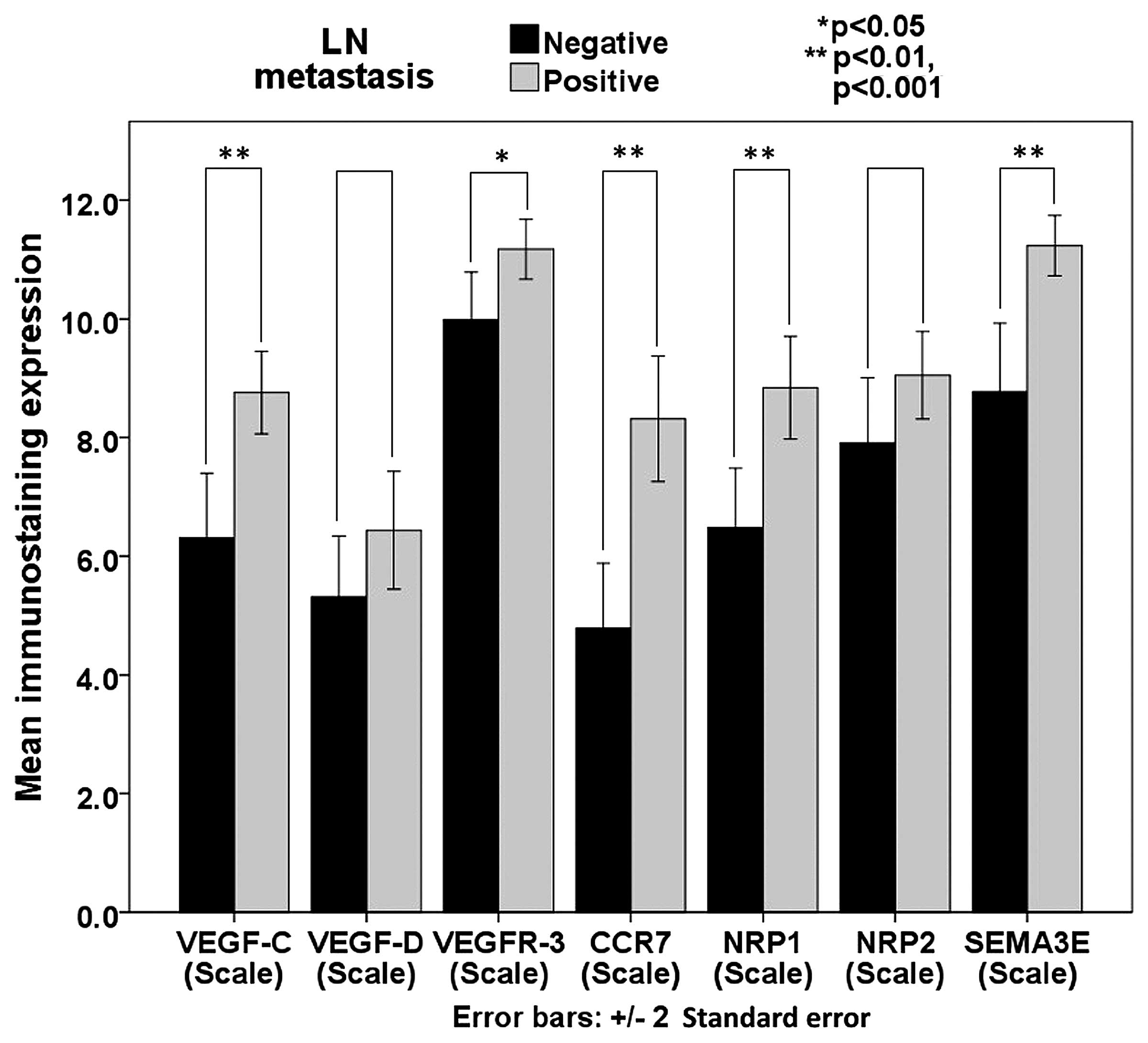
High expression levels of VEGF-C, VEGF-D, VEGFR-3,
CCR7, NRP1, NRP2, and SEMA3E were detected in 39 (48.8%), 44 (55%),
45 (56.3%), 41 (51.3%), 37 (46.3%), 45 (56.3%), and 54 (67.5%)
tumor specimens, respectively. In contrast, 41 (51.3%), 36 (45%),
35 (43.8%), 39 (48.8%), 43 (53.8%), 35 (43.8%), and 26 (32.5%)
tumor specimens exhibited low expression levels of VEGF-C, VEGF-D,
VEGFR-3, CCR7, NRP1, NRP2, and SEMA3E, respectively. The mean
expression levels of VEGF-C, VEGF-D, VEGFR-3, CCR7, NRP1, NRP2, and
SEMA3E were 7.538, 5.875, 10.581, 6.550, 7.663, 8.481, and 10.006,
respectively (Fig. 2).
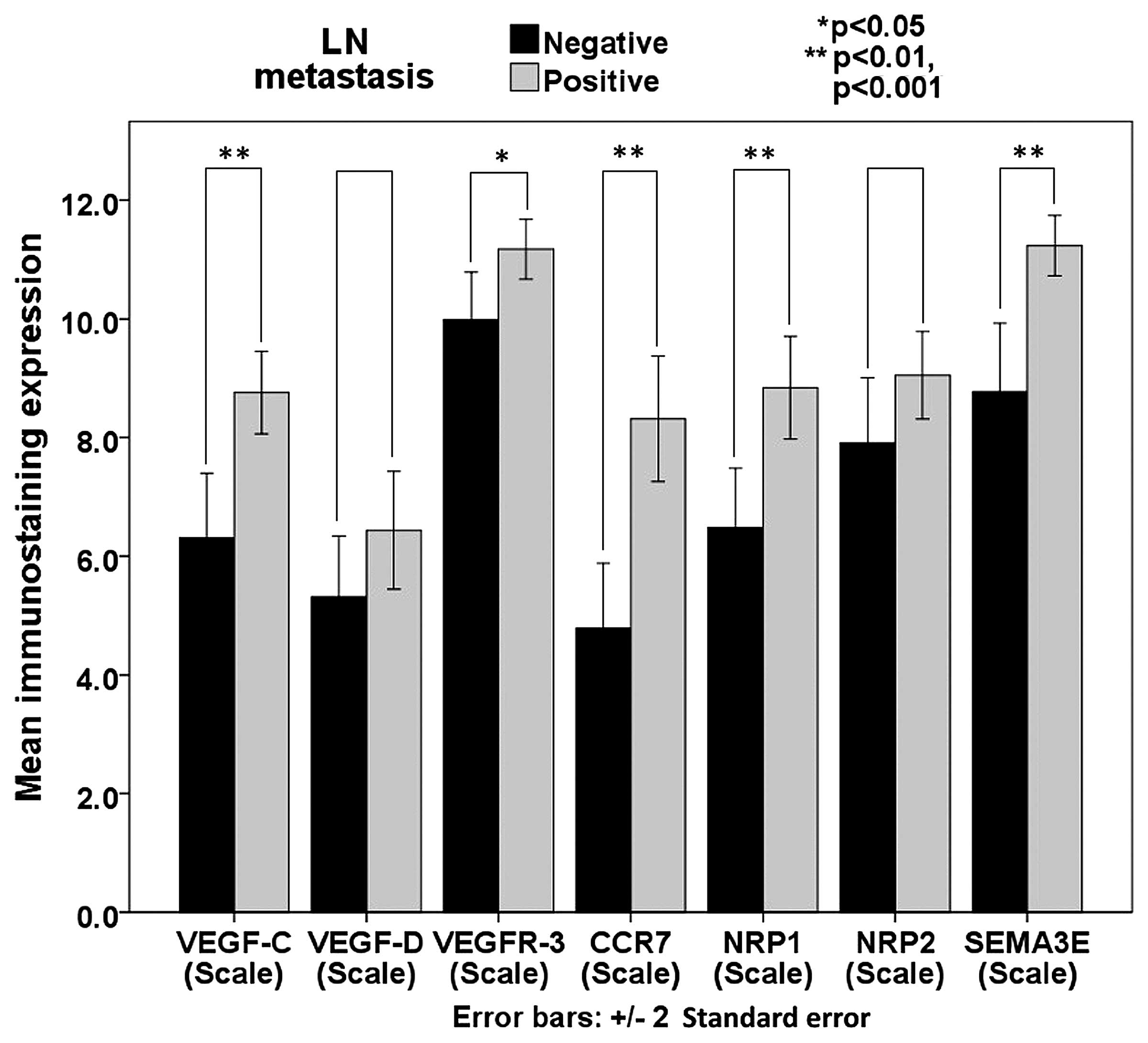 | Figure 2Relationship between the expression
of proteins and LN metastasis. The relationship between protein
expression and LN metastasis was analyzed by the independent
samples t-test, and it is shown in this clustered bar chart. High
expression levels for each of the proteins were identified in most
of the specimens, and a significant association was demonstrated
between LN metastasis and the expression levels of VEGF-C, VEGFR-3,
CCR7, NRP1, and SEMA3E. *P<0.05;
**p<0.01, p<0.001. LN, lymph node; VEGF, vascular
endothelial growth factor; VEGFR-3, VEGF receptor-3; CCR7, C-C
motif chemokine receptor 7; NRP, neuropilin; SEMA3E, semaphorin
3E. |
MVD was found to range between 5.5 and 38.5
µm2 of blood vessels per square millimeter
of the tumor (median, 19.92; mean ± standard deviation (SD),
20.31±6.26), whereas LVD ranged between 3.83 and 20.83
µm2 of lymphatic vessels per square millimeter of
the tumor (median, 6.33; mean ± SD, 6.85±2.29) (Figs. 3 and 4).
The relationship between
clinicopathological features and the expression of angiogenic and
lymphangiogenic biomarkers
Chi-square and Fischer's exact tests were performed
to assess the association between clinicopathological features and
the expression levels of VEGF-C, VEGF-D, VEGFR-3, CCR7, NRP1, NRP2,
and SEMA3E. The results showed that the expression level of VEGF-C
was significantly associated with only pathological LN size
(p<0.05) and LN metastasis (p<0.05), whereas the expression
level of VEGF-D was significantly associated with only gender
(p<0.05) and age (p<0.05). Moreover, the expression level of
VEGFR-3 was significantly associated with only age (p<0.01), N
classification (Japan Society for Oral Tumors, classification for
regional LN metastasis; p<0.05), and LN metastasis (p<0.01).
The expression level of CCR7 was significantly associated only with
gender (p<0.05), N classification (p<0.05), and LN metastasis
(p=0.001). In addition, the expression level of NRP1 in the SCC
cells was significantly associated only with pathological LN size
(p<0.05) and LN metastasis (p=0.001), and the expression level
of NRP2 was not significantly associated with any of the
clinicopathological features, whereas the expression level of
SEMA3E was significantly associated with only N classification
(p<0.05) and LN metastasis (p=0.001) (Table I).
 | Table IRelationship between
clinicopathological features and the expression levels of the
proteins VEGF-C, VEGF-D, VEGFR-3, CCR7, NRP1, NRP2, and SEMA3E. |
Table I
Relationship between
clinicopathological features and the expression levels of the
proteins VEGF-C, VEGF-D, VEGFR-3, CCR7, NRP1, NRP2, and SEMA3E.
| Cases | VEGF-C expression
| VEGF-D expression
| VEGFR-3 expression
| CCR7 expression
|
|---|
| Low | High | P-value | Low | High | P-value | Low | High | P-value | Low | High | P-value |
|---|
| Gender |
| Female | 25 | 14 | 11 | N.S. | 7 | 18 | 0.039 | 8 | 17 | 0.153 | 7 | 18 | 0.012 |
| Male | 55 | 27 | 28 | | 29 | 26 | | 27 | 28 | | 32 | 23 | |
| Age (years) |
| <60 | 34 | 19 | 15 | N.S. | 20 | 14 | 0.033 | 21 | 13 | 0.005 | 19 | 15 | N.S. |
| ≥60 | 46 | 22 | 24 | | 16 | 30 | | 14 | 32 | | 20 | 26 | |
| N
classification |
| N0 | 40 | 26 | 14 | 0.047 | 20 | 20 | N.S. | 24 | 16 | 0.035 | 27 | 13 | 0.015 |
| N1 | 13 | 4 | 9 | | 3 | 10 | | 5 | 8 | | 3 | 10 | |
| N2b | 18 | 7 | 11 | | 8 | 10 | | 5 | 13 | | 5 | 13 | |
| N2c | 7 | 2 | 5 | | 4 | 3 | | 1 | 6 | | 3 | 4 | |
| N3 | 2 | 2 | 0 | | 1 | 1 | | 0 | 2 | | 1 | 1 | |
| LN metastasis |
| Negative | 40 | 26 | 14 | 0.014 | 20 | 20 | N.S. | 24 | 16 | 0.003 | 27 | 13 | 0.001 |
| Positive | 40 | 15 | 25 | | 16 | 24 | | 11 | 29 | | 12 | 28 | |
| Cases | NRP1 expression
| NRP2 expression
| SEMA3E expression
|
|---|
| Low | High | P-value | Low | High | P value | Low | High | P-value |
|---|
| Gender |
| Female | 25 | 10 | 15 | N.S. | 10 | 15 | N.S. | 7 | 18 | N.S. |
| Male | 55 | 33 | 22 | | 25 | 30 | | 19 | 36 | |
| Age (years) |
| <60 | 34 | 22 | 12 | N.S. | 17 | 17 | N.S. | 12 | 22 | N.S. |
| ≥60 | 46 | 21 | 25 | | 18 | 28 | | 14 | 32 | |
| N
classification |
| N0 | 40 | 29 | 11 | 0.012 | 20 | 20 | N.S. | 20 | 20 | 0.016 |
| N1 | 13 | 5 | 8 | | 3 | 10 | | 1 | 12 | |
| N2b | 18 | 7 | 11 | | 8 | 10 | | 4 | 14 | |
| N2c | 7 | 1 | 6 | | 4 | 7 | | 1 | 6 | |
| N3 | 2 | 1 | 1 | | 0 | 2 | | 0 | 2 | |
| LN metastasis |
| Negative | 40 | 29 | 11 | 0.001 | 20 | 20 | N.S. | 20 | 20 | 0.001 |
| Positive | 40 | 14 | 26 | | 15 | 25 | | 6 | 34 | |
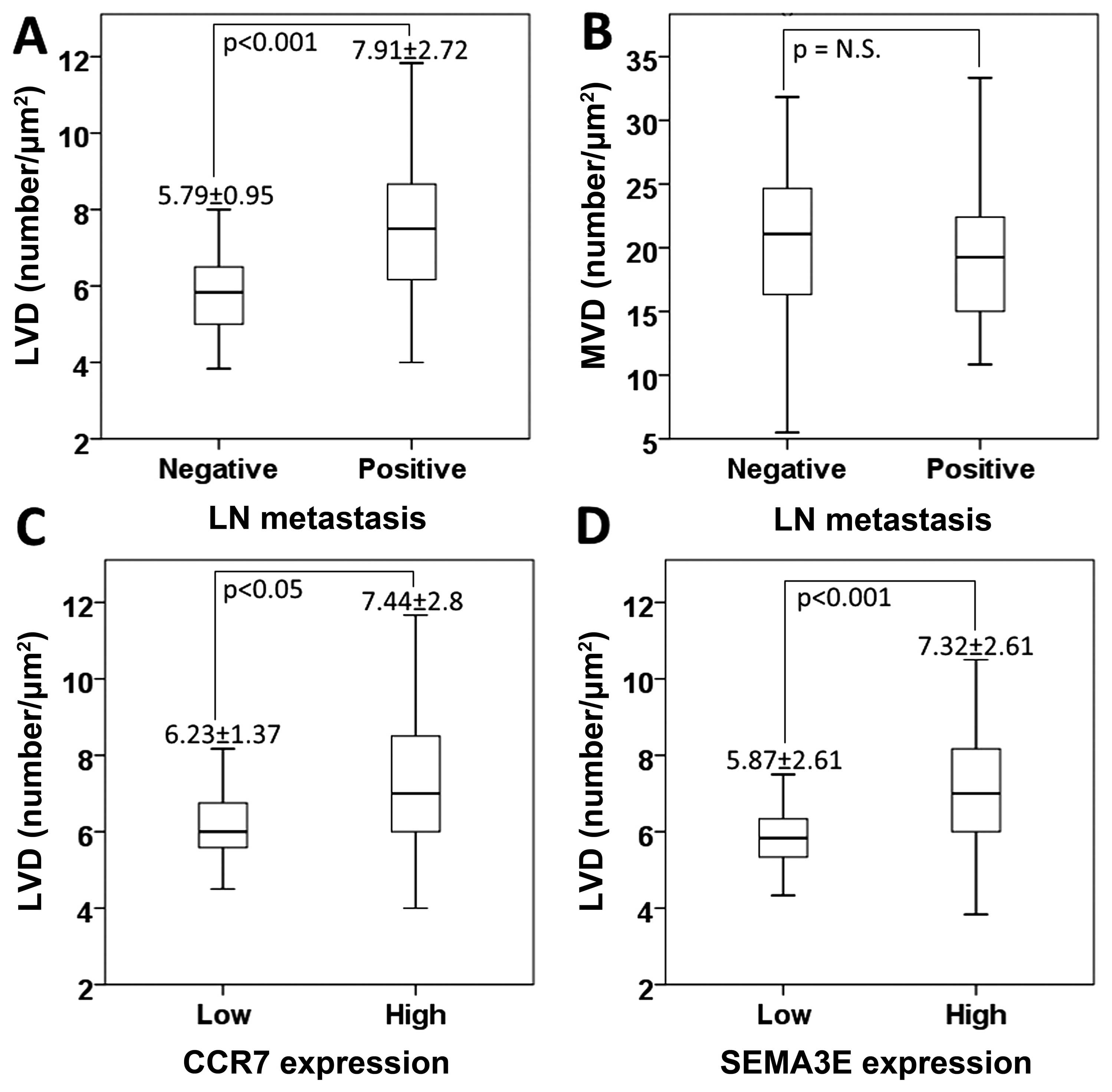
The relationship between the expression
levels of angiogenic and lymphangiogenic biomarkers and MVD or
LVD
The relationship between angiogenesis and
lymphangiogenesis in the primary SCC and LN metastasis was examined
by assessing MVD, through immunohistochemical staining with the
CD-34 antibody, and LVD, through immunohistochemical staining with
the D2-40 antibody. LVD ranged between 3.83 and 20.83
µm2 of lymphatic vessels per square millimeter of
the tumor (median, 6.33; mean ± SD, 6.85±2.29). The independent
samples t-test showed a significant association between LVD and LN
metastasis, with the mean LVD being lower in the metastatic
LN-negative group when compared to the metastatic LN-positive group
[mean ± SD, 5.79±0.95 and 7.91±2.72, respectively; p<0.001; t
(78)=4.66]. No significant association was detected between MVD and
LN metastasis.
The independent samples t-test was also used to
assess the association between biomarker expression and MVD or LVD.
We found that LVD was significantly associated with the expression
of CCR7 (p<0.05) and SEMA3E (p<0.001), mainly at the invasive
edges. However, no such association was detected between MVD and
the expression of any of the biomarkers (Fig. 4) (Table
II).
 | Table IIThe relationship between protein
expression levels and MVD or LVD. |
Table II
The relationship between protein
expression levels and MVD or LVD.
| MVD
| LVD
|
|---|
| Mean | SD | P-value | Mean | SD | P-value |
|---|
| LN metastasis |
| Negative | 20.79 | 6.72 | 0.497 | 5.79 | 0.95 | <0.001 |
| Positive | 19.83 | 5.82 | | 7.91 | 2.72 | |
| VEGF C |
| Low | 21.28 | 5.49 | 0.154 | 6.53 | 1.5 | 0.154 |
| High | 19.28 | 6.90 | | 7.18 | 2.89 | |
| VEGF D |
| Low | 20.17 | 6.19 | 0.856 | 6.72 | 1.54 | 0.207 |
| High | 20.42 | 6.40 | | 6.95 | 2.77 | |
| VEGFR 3 |
| Low | 19.71 | 6.17 | 0.458 | 6.46 | 1.46 | 0.183 |
| High | 20.77 | 6.37 | | 7.15 | 2.75 | |
| CCR7 |
| Low | 20.63 | 6.48 | 0.655 | 6.23 | 1.37 | 0.016 |
| High | 20.00 | 6.11 | | 7.44 | 2.8 | |
| NRP1 |
| Low | 20.33 | 6.27 | 0.979 | 6.42 | 1.62 | 0.69 |
| High | 20.29 | 6.35 | | 7.35 | 2.83 | |
| NRP2 |
| Low | 20.15 | 6.03 | 0.841 | 6.8 | 1.66 | 0.877 |
| High | 20.43 | 6.50 | | 6.89 | 2.7 | |
| SEMA3E |
| Low | 21.49 | 5.60 | 0.245 | 5.87 | 0.86 | <0.001 |
| High | 19.74 | 6.53 | | 7.32 | 2.61 | |
Logistic regression analysis of
predictive factors and LN metastasis
Univariate logistic regression analysis was
performed to assess the association between clinicopathological
features and LN metastasis. The results showed that SCC of cancer
stage T4 is more likely to have LN metastasis (OR, 9.778; 95%
confidence interval (CI), 1.551–61.646; p≤0.05). Multivariate
logistic regression analysis also showed that cancer stage T4 was
significantly associated with LN metastasis (OR, 12.601; 95% CI,
0.998-159.08; p≤0.05). No significant relationship was identified
between LN metastasis and the mode of invasion (YK classification),
the differentiation of SCC cells, or other clinical factors in any
of the regression analyses (Table
III).
 | Table IIIRelationship between the predictive
factors and LN metastasis. |
Table III
Relationship between the predictive
factors and LN metastasis.
| Univariate
| Multivariate
|
|---|
| Odds ratio | 95% CI | P value | Odds ratio | 95% CI | P value |
|---|
| T stage T1 ref
T4 | 9.778 | 1.551–61.646 | 0.015 | 12.601 | 0.998–159.08 | 0.05 |
| VEGF-C
expression | 3.095 | 1.243–7.706 | 0.015 | 2.06 | 0.462–9.178 | 0.343 |
| VEGFR-3
expression | 3.955 | 1.546–10.114 | 0.004 | 2.436 | 0.484–12.272 | 0.28 |
| CCR7
expression | 4.846 | 1.882–12.482 | 0.001 | 1.402 | 0.301–6.538 | 0.667 |
| NRP1
expression | 4.896 | 1.892–12.669 | 0.001 | 5.905 | 1.274–27.372 | 0.023 |
| SEMA3E
expression | 5.667 | 1.951–16.462 | 0.001 | 1.979 | 0.389–10.065 | 0.411 |
| LVD (D2-40) | 2.832 | 1.716–4.673 | <0.001 | 2.527 | 1.412–4.522 | 0.002 |
Univariate analysis showed significant association
between LN metastasis and the expression levels of VEGF-C (OR,
3.095; 95% CI, 1.243–7.706; p<0.05), VEGFR-3 (OR, 3.955; 95% CI,
1.546–10.114; p<0.01), CCR7 (OR, 4.846; 95% CI, 1.882–12.482;
p=0.001), NRP1 (OR, 4.896; 95% CI, 1.892–12.669; p=0.001), and
SEMA3E (OR, 5.667; 95% CI, 1.951–16.462; p=0.001). No correlation
was identified between LN metastasis and the expression levels of
NRP2 and VEGF-D. However, a significant association was observed
between LN metastasis and LVD (OR, 2.832; 95% CI, 1.716–4.673;
p<0.0001), but not MVD. By contrast, multivariate analysis
showed only the association between LN metastasis and NRP1
expression level (OR, 5.905; 95% CI, 1.274–27.372; p<0.05) or
LVD (OR, 2.527; 95% CI, 1.412–4.522; p<0.01). No correlation was
identified between LN metastasis and the expression levels of the
other proteins (Table III).
The relationship between the expression
of angiogenic and lymphangiogenic biomarkers and survival time
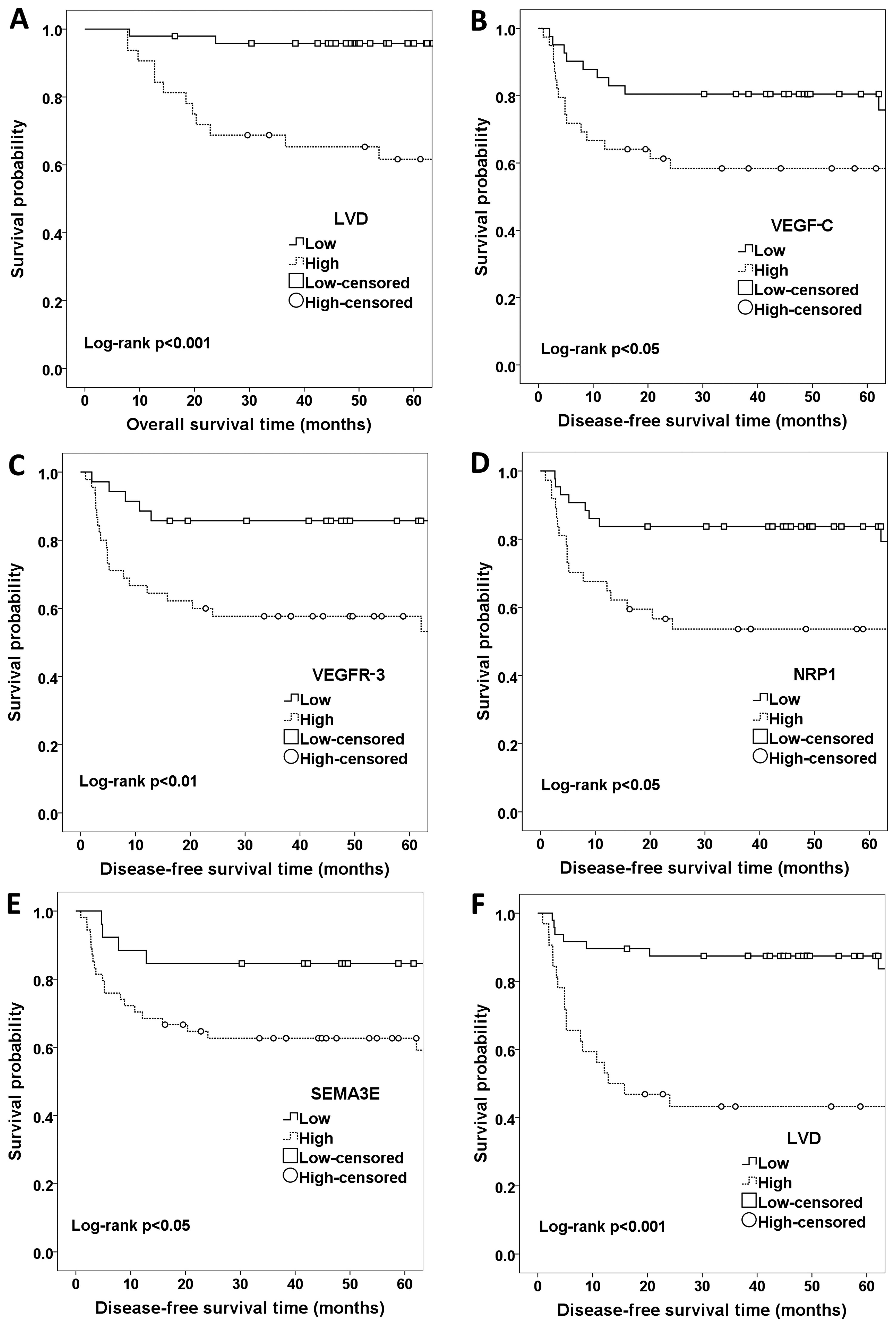
We used the Kaplan-Meier method to determine the
association between LN metastasis and prognosis in patients with
oral SCC. The results showed a reduced overall survival time for
patients with metastatic SCC when compared to patients with
non-metastatic cancer (patients with LN metastasis were associated
with overall survival time and LVD exhibited an association,
log-rank p<0.001) (Fig. 5).
The Kaplan-Meier analysis also showed that patients
with high expression levels of VEGF-C, VEGFR-3, NRP1, and SEMA3E,
were more likely to have localized or regional recurrence after
treatment (VEGF-C, VEGFR-3, NRP1, and SEMA3E were associated with
disease-free survival time, log-rank p<0.05).
Patients with metastatic SCC were also more likely
to have localized or regional recurrence after treatment (patients
with LN metastasis were associated with disease-free survival time
and LVD exhibited an association, log-rank p<0.001) (Fig. 5). To summarize, LN metastasis was
found to be associated with poor survival in SCC.
Discussion
In the present study, several biomarkers have been
proposed for SCC. The aim of this study was to evaluate the
expression levels of the following growth factors and receptors in
SCC of the tongue: VEGF-C, VEGF-D, VEGFR-3, CCR7, NRP1, NRP2, and
SEMA3E. Furthermore, we investigated the association between the
expression levels of these proteins and intratumoral MVD, using
CD-34 antibody, or LVD, using D2-40 podoplanin antibody, as
indicators of angiogenesis and lymphangiogenesis, respectively.
The PI3K/AKT, ERK1/2, and p38 pathways are crucial
for cellular proliferation and survival (26). However, the association between
disease-specific survival and the expression of VEGF-C, VEGF-D, and
their receptor VEGFR-3 remains controversial. Many studies have
proposed a strong association between LN metastasis and the
expression levels of VEGF-C and VEGF-D in SCC. However, the
association between LN metastasis and VEGF-D is controversial and
has not been supported by other studies. In fact, VEGF-D has been
reported to act as a suppressor in some types of cancers (27,28). A
relationship between LN metastasis and the expression levels of
VEGF-C or VEGFR-3 has been reported for head and neck SCC, gastric,
breast, thyroid, prostate, esophageal, and colorectal carcinomas
(6).
The present study showed that LN metastasis is
significantly correlated with the expression levels of VEGF-C and
VEGFR-3, but not VEGF-D, based on immunohistochemical staining
(p<0.05) and univariate logistic regression analysis
(p<0.01). Immunostaining for these proteins was extensively
associated with some clinicopathological features and was strongly
correlated with disease-specific survival, suggesting a role for
VEGF-C and VEGFR-3 as biomarkers for oral SCC metastasis. These
results are in agreement with other reports on head and neck cancer
(29), which suggest that VEGF-D is
less important than VEGF-C for LN metastasis. However, it is still
necessary for the metastasis mechanism, although its role is
presently controversial. The possibility that VEGFR-3 expression in
cancer cells could be associated with increased regional LN
metastasis in oral SCC is also in agreement with other recent
studies, suggesting a role for VEGFR-3 expression in predicting LN
metastasis of SCC.
Furthermore, we found a strong relationship between
the expression levels of both VEGF-C and VEGFR-3 and
lymphangiogenesis in patients with oral SCC. Many clinical and
preclinical studies have suggested that clinicopathological
features are usually unreliable predictors of LN metastasis, with
highly variable results, particularly for oral SCC (30–32).
However, in this study, we suggest that LVD could be a predictive
marker for LN metastasis in oral SCC. Furthermore, VEGF-C/VEGFR-3
pathway inhibition has been shown to inhibit cancer progression
(33–36). Therefore, signaling through VEGFR-3
is not necessarily a result of LN metastasis. The fact that VEGFR-3
can form heterodimers with VEGFR-2 makes this mechanism even more
complicated (17).
This study also predicted a strong correlation
between LVD and LN metastasis in oral SCC. Both disease-free and
overall survival were associated with intra- and peritumoral LVD,
as patients with a high LVD were revealed to have poor survival and
a high possibility of recurrence. We did not detect any association
between MVD and LN metastasis or prognosis. Other studies, by
systematic review, have shown that MVD is unlikely to be a
prognostic factor in early stage non-small cell lung cancer
patients (6).
The association of angiogenic and lymphangiogenic
biomarkers with prognosis in SCC patients remains controversial due
to the variable outcomes reported by independent studies (17,37).
Some biomarkers have been correlated with poor prognosis or
prolonged survival (38–40), whereas others have failed to show
any prognostic significance (37).
In our study, VEGF-C and VEGFR-3 expression levels were correlated
with poor prognosis and a high possibility of localized or regional
recurrence after treatment.
Many studies have reported that the expression of
CCR7 in tumors, such as metastatic tumor cells of gastric,
esophageal, breast, renal, oropharyngeal, and head and neck
cancers, is significantly correlated with poor prognosis. Many
studies have also reported a relationship between CCR7 expression
levels and oral as well as head and neck SCC (9,41).
In the present study, we found that CCR7
immunostaining was strong in tongue cancer tissue. Univariate
logistic regression analysis showed that CCR7 expression was
significantly correlated with LN metastasis (p=0.001) as well as
some clinicopathological features. Furthermore, a significant
association was detected between upregulated CCR7 expression and
LVD; however, no association was estimated between this upregulated
CCR7 expression and prognosis. The results showed a possible role
for CCR7 in the progression of tongue SCC as well as in mediating
signaling in metastatic SCC.
The interactions between the proteins in the VEGF
pathway are complex; which includes VEGF-A, VEGF-B, VEGF-C, VEGF-D,
and PlGF, their tyrosine kinase receptors VEGFR-1, VEGFR-2, and
VEGFR-3, and two NRP receptors NRP1 and NRP2. The VEGF receptors
can form complexes with the NRP receptors and modulate the
signaling outcomes through p38 MAPK pathway activation, leading to
migration and survival of endothelial cells. Semaphorin family
competes with VEGFs to bind to NRPs and modulate the angiogenesis
mechanism (42). Many previous
studies have investigated the expression of NRP1 and NRP2 in SCC of
the tongue, esophagus, colon/rectum, breast, stomach, and lungs
(10). Moreover, some studies have
shown that NRP1 had a higher expression level compared to that of
NRP2 (7). NRP1 and NRP2 expression
levels have been shown to be prospective indicators of poor
prognosis in colorectal cancer (7).
However, other studies have found that NRP1 was neither correlated
with any clinical features nor with poor prognosis in SCC of the
tongue (43).
In the present study, NRP1 was shown, by
immunohistochemical analysis, to be extensively expressed in
cancerous tongue tissue. Univariate logistic regression analysis
showed that NRP1 expression was significantly correlated with LN
metastasis (p=0.001) as well as with some other clinicopathological
features (such as N classification). This indicates the
controversial role of NRP1 in tumor growth and progression. The
upregulation of NRP1 was also significantly correlated with poor
disease-free survival. However, NRP2 did not show any association
with LN metastasis, prognosis, or clinicopathological features. A
possible explanation may be that NRP1 inhibits apoptosis by binding
to VEGF and NRP2 increases the epithelial-mesenchymal transition
(7). Furthermore, NRP1 expression
appears to be more involved in angiogenesis and lymphangiogenesis
than NRP2 expression. In general, these data suggest that both NRP1
and NRP2 are possible targets for chemotherapy; however, agents
targeting NRP1 may have a greater anti-angiogenic effects in
SCC.
Semaphorins, and their receptors, are a large family
of extracellular signaling proteins with important roles in
angiogenesis and tumor progression. SEMA3E is a secreted protein
that recognizes the plexin-D1 receptor as well as the NRP receptors
(12,44). However, the functional relevance of
SEMA3E in cancer is poorly understood. In addition to providing
inhibitory signals for angiogenesis, SEMA3E/plexin-D1 signaling can
regulate other cell types (42,45).
Casazza et al found that ʻSEMA3E inhibits tumor growth, but
promotes metastasisʼ, in an NRP-independent manner (14).
SEMA3E expression is positively correlated with
metastatic progression in highly invasive and metastatic mammary
carcinomas, high- vs. low-grade glioblastomas, colon and liver
cancers, and melanomas (13,14).
Increased expression of SEMA3E has been shown in metastatic cancers
when compared to that of non-metastatic cancers. Kaplan-Meier
survival analysis revealed that SEMA3E expression levels in primary
tumors were significantly inversely correlated with patient
survival, whereas the opposite was true for bladder carcinomas
(14) as well as for primary and
metastatic prostate tumors (42).
The present study is the first time where SEMA3E
expression has been investigated in SCC of the tongue. Univariate
logistic regression analysis revealed that SEMA3E expression was
significantly correlated with LN metastasis (p=0.001). SEMA3E was
shown to be highly expressed in immunohistochemical analysis, and
its association with clinicopathological features was stronger than
the association detected between upregulated CCR7 expression and
LVD. In addition, SEMA3E is strongly correlated with
disease-specific survival, suggesting its importance as a biomarker
in oral SCC metastasis. This result is consistent with previous
studies in colon and liver cancers, melanomas, and metastatic
mammary carcinomas. The finding that SEMA3E is also important in
tongue SCC suggests that its signaling is crucially involved in the
metastatic mechanisms of multiple cancer cells and is therefore a
promising therapeutic target for the prevention of tumor
metastasis.
Due to the limitations of this retrospective cohort
study, the analysis of archival documents is a better way to
analyze multiple outcomes and deal with potential heterogeneity and
rare cases. This may also help in obtaining sufficient data for the
identification of prognostic and predictive biomarkers and may
improve the study design of randomized trials. Further studies in
larger cohorts would better validate our results for oral SCC
patients.
In summary, we suggest that high expression levels
of VEGF-C, VEGFR-3, CCR7, and SEMA3E, as detected by
immunohistochemical staining, serve as non-independent predictors
of LN metastasis. Furthermore, LVD and NRP1 were found to be
independent predictors of LN metastasis in SCC of the tongue.
Statistical regression analysis and prognostic analysis showed that
these factors are more likely to predict LN metastasis; therefore,
these factors would be useful in estimating the possibility of LN
metastasis in SCC. The accurate assessment of LN metastasis is
crucial to improve the survival of oral cancer patients after
treatment.
Acknowledgments
This study was supported by grants from the Ministry
of Education, Culture, Sports, Science, and Technology in Japan and
by JSPS KAKENHI (grant no. 15K20519).
References
|
1
|
Lee D, Wada K, Taniguchi Y, Al-Shareef H,
Masuda T, Usami Y, Aikawa T, Okura M, Kamisaki Y and Kogo M:
Expression of fatty acid binding protein 4 is involved in the cell
growth of oral squamous cell carcinoma. Oncol Rep. 31:1116–1120.
2014.PubMed/NCBI
|
|
2
|
Doshi NP, Shah SA, Patel KB and Jhabuawala
MF: Histological grading of oral cancer: A comparison of different
systems and their relation to lymph node metastasis. Nat J Commun
Med. 2:136–142. 2011.
|
|
3
|
Watanabe S, Kato M, Kotani I, Ryoke K and
Hayashi K: Lymphatic vessel density and vascular endothelial growth
factor expression in squamous cell carcinomas of lip and oral
cavity: A clinicopathological analysis with immunohistochemistry
using antibodies to D2-40, VEGF-C and VEGF-D. Yonago Acta Med.
56:29–37. 2013.PubMed/NCBI
|
|
4
|
Miyata Y, Kanda S, Ohba K, Nomata K,
Hayashida Y, Eguchi J, Hayashi T and Kanetake H: Lymphangiogenesis
and angiogenesis in bladder cancer: Prognostic implications and
regulation by vascular endothelial growth factors-A, -C, and -D.
Clin Cancer Res. 12:800–806. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hicklin DJ and Ellis LM: Role of the
vascular endothelial growth factor pathway in tumor growth and
angiogenesis. J Clin Oncol. 23:1011–1027. 2005. View Article : Google Scholar
|
|
6
|
Sugiura T, Inoue Y, Matsuki R, Ishii K,
Takahashi M, Abe M and Shirasuna K: VEGF-C and VEGF-D expression is
correlated with lymphatic vessel density and lymph node metastasis
in oral squamous cell carcinoma: Implications for use as a
prognostic marker. Int J Oncol. 34:673–680. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Staton CA, Koay I, Wu JM, Hoh L, Reed MW
and Brown NJ: Neuropilin-1 and neuropilin-2 expression in the
adenoma-carcinoma sequence of colorectal cancer. Histopathology.
62:908–915. 2013. View Article : Google Scholar
|
|
8
|
Kodama J, Hasengaowa, Kusumoto T, Seki N,
Matsuo T, Ojima Y, Nakamura K, Hongo A and Hiramatsu Y: Association
of CXCR4 and CCR7 chemokine receptor expression and lymph node
metastasis in human cervical cancer. Ann Oncol. 18:70–76. 2007.
View Article : Google Scholar
|
|
9
|
Ishida K, Iwahashi M, Nakamori M, Nakamura
M, Yokoyama S, Iida T, Naka T, Nakamura Y and Yamaue H: High CCR7
mRNA expression of cancer cells is associated with lymph node
involvement in patients with esophageal squamous cell carcinoma.
Int J Oncol. 34:915–922. 2009.PubMed/NCBI
|
|
10
|
Alattar M, Omo A, Elsharawy M and Li J:
Neuropilin-1 expression in squamous cell carcinoma of the
oesophagus. Eur J Cardiothorac Surg. 45:514–520. 2014. View Article : Google Scholar
|
|
11
|
Nasarre P, Gemmill RM and Drabkin HA: The
emerging role of class-3 semaphorins and their neuropilin receptors
in oncology. Onco Targets Ther. 7:1663–1687. 2014.PubMed/NCBI
|
|
12
|
Kumanogoh A and Kikutani H: Immunological
functions of the neuropilins and plexins as receptors for
semaphorins. Nat Rev Immunol. 13:802–814. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Klagsbrun M and Shimizu A: Semaphorin 3E,
an exception to the rule. J Clin Invest. 120:2658–2660. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Casazza A, Finisguerra V, Capparuccia L,
Camperi A, Swiercz JM, Rizzolio S, Rolny C, Christensen C, Bertotti
A, Sarotto I, et al: Sema3E-Plexin D1 signaling drives human cancer
cell invasiveness and metastatic spreading in mice. J Clin Invest.
120:2684–2698. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Luchino J, Hocine M, Amoureux MC, Gibert
B, Bernet A, Royet A, Treilleux I, Lécine P, Borg JP, Mehlen P, et
al: Semaphorin 3E suppresses tumor cell death triggered by the
plexin D1 dependence receptor in metastatic breast cancers. Cancer
Cell. 24:673–685. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Franceschi S, Bidoli E, Herrero R and
Muñoz N: Comparison of cancers of the oral cavity and pharynx
worldwide: Etiological clues. Oral Oncol. 36:106–115. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Anagnostou VK, Tiniakos DG, Fotinou M,
Achimastos A and Syrigos KN: Multiplexed analysis of angiogenesis
and lymphangiogenesis factors predicts outcome for non-small cell
lung cancer patients. Virchows Arch. 458:331–340. 2011. View Article : Google Scholar
|
|
18
|
Izumo T, Kirita T, Ariji E, Ozeki S, Okada
N, Okabe S, Okazaki Y, Omura K, Kusama M, Sato T, et al: Working
Group 1 on the ʻGuidelines for Clinical and Pathological Studies of
Oral Cancerʼ, Scientific Committee, Japan Society for Oral Tumors:
General rules for clinical and pathological studies on oral cancer:
A synopsis. Jpn J Clin Oncol. 42:1099–1109. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yamamoto E, Kohama G, Sunakawa H, Iwai M
and Hiratsuka H: Mode of invasion, bleomycin sensitivity, and
clinical course in squamous cell carcinoma of the oral cavity.
Cancer. 51:2175–2180. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yamamoto E, Miyakawa A and Kohama G: Mode
of invasion and lymph node metastasis in squamous cell carcinoma of
the oral cavity. Head Neck Surg. 6:938–947. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Barnes DM, Harris WH, Smith P, Millis RR
and Rubens RD: Immunohistochemical determination of oestrogen
receptor: Comparison of different methods of assessment of staining
and correlation with clinical outcome of breast cancer patients. Br
J Cancer. 74:1445–1451. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ding Y, Shimada Y, Maeda M, Kawabe A,
Kaganoi J, Komoto I, Hashimoto Y, Miyake M, Hashida H and Imamura
M: Association of CC chemokine receptor 7 with lymph node
metastasis of esophageal squamous cell carcinoma. Clin Cancer Res.
9:3406–3412. 2003.PubMed/NCBI
|
|
23
|
Krajewska M, Krajewski S, Epstein JI,
Shabaik A, Sauvageot J, Song K, Kitada S and Reed JC:
Immunohistochemical analysis of bcl-2, bax, bcl-X, and mcl-1
expression in prostate cancers. Am J Pathol. 148:1567–1576.
1996.PubMed/NCBI
|
|
24
|
Remmele W and Stegner HE:
Immunhistochemischer nachweis von östrogenerezeptoren (ER-ICA) im
mammakarizi-nomgewebe: Vorschlag zur einheitlichen bewertung des
untersu- chungsbefundes. Frauenarzt. 28:41–43. 1987.
|
|
25
|
Weidner N, Semple J, Welch W and Folkman
J: Tumor angiogenesis and metastasis - correlation in invasive
breast carcinoma. N Engl J Med. 324:1–8. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Feng Y, Hu J, Ma J, Feng K, Zhang X, Yang
S, Wang W, Zhang J and Zhang Y: RNAi-mediated silencing of VEGF-C
inhibits non-small cell lung cancer progression by simultaneously
down-regulating the CXCR4, CCR7, VEGFR-2 and VEGFR-3-dependent
axes-induced ERK, p38 and AKT signalling pathways. Eur J Cancer.
47:2353–2363. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Niki T, Iba S, Tokunou M, Yamada T,
Matsuno Y and Hirohashi S: Expression of vascular endothelial
growth factors A, B, C, and D and their relationships to lymph node
status in lung adenocarcinoma. Clin Cancer Res. 6:2431–2439.
2000.PubMed/NCBI
|
|
28
|
George ML, Tutton MG, Janssen F, Arnaout
A, Abulafi AM, Eccles SA and Swift RI: VEGF-A, VEGF-C, and VEGF-D
in colorectal cancer progression. Neoplasia. 3:420–427. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shintani S, Li C, Ishikawa T, Mihara M,
Nakashiro K and Hamakawa H: Expression of vascular endothelial
growth factor A, B, C, and D in oral squamous cell carcinoma. Oral
Oncol. 40:13–20. 2004. View Article : Google Scholar
|
|
30
|
Kitadai Y, Amioka T, Haruma K, Tanaka S,
Yoshihara M, Sumii K, Matsutani N, Yasui W and Chayama K:
Clinicopathological significance of vascular endothelial growth
factor (VEGF)-C in human esophageal squamous cell carcinomas. Int J
Cancer. 93:662–666. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lalla RV, Boisoneau DS, Spiro JD and
Kreutzer DL: Expression of vascular endothelial growth factor
receptors on tumor cells in head and neck squamous cell carcinoma.
Arch Otolaryngol Head Neck Surg. 129:882–888. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sanmartín E, Sirera R, Usó M, Blasco A,
Gallach S, Figueroa S, Martínez N, Hernando C, Honguero A,
Martorell M, et al: A gene signature combining the tissue
expression of three angiogenic factors is a prognostic marker in
early-stage non-small cell lung cancer. Ann Surg Oncol. 21:612–620.
2014. View Article : Google Scholar
|
|
33
|
Iljin K, Karkkainen MJ, Lawrence EC, Kimak
MA, Uutela M, Taipale J, Pajusola K, Alhonen L, Halmekytö M,
Finegold DN, et al: VEGFR3 gene structure, regulatory region, and
sequence polymorphisms. FASEB J. 15:1028–1036. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Neuchrist C, Erovic BM, Handisurya A,
Fischer MB, Steiner GE, Hollemann D, Gedlicka C, Saaristo A and
Burian M: Vascular endothelial growth factor C and vascular
endothelial growth factor receptor 3 expression in squamous cell
carcinomas of the head and neck. Head Neck. 25:464–474. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Su JL, Yang PC, Shih JY, Yang CY, Wei LH,
Hsieh CY, Chou CH, Jeng YM, Wang MY, Chang KJ, et al: The
VEGF-C/Flt-4 axis promotes invasion and metastasis of cancer cells.
Cancer Cell. 9:209–223. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chaudary N, Milosevic M and Hill RP:
Suppression of vascular endothelial growth factor receptor 3
(VEGFR3) and vascular endothelial growth factor C (VEGFC) inhibits
hypoxia-induced lymph node metastases in cervix cancer. Gynecol
Oncol. 123:393–400. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhan P, Wang J, Lv XJ, Wang Q, Qiu LX, Lin
XQ, Yu LK and Song Y: Prognostic value of vascular endothelial
growth factor expression in patients with lung cancer: A systematic
review with meta-analysis. J Thorac Oncol. 4:1094–1103. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Carrillo de Santa Pau E, Arias FC, Caso
Peláez E, Muñoz Molina GM, Sánchez Hernández I, Muguruza Trueba I,
Moreno Balsalobre R, Sacristán López S, Gómez Pinillos A and del
Val Toledo Lobo M: Prognostic significance of the expression of
vascular endothelial growth factors A, B, C, and D and their
receptors R1, R2, and R3 in patients with nonsmall cell lung
cancer. Cancer. 115:1701–1712. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Maekawa S, Iwasaki A, Shirakusa T, Enatsu
S, Kawakami T and Kuroki M and Kuroki M: Correlation between lymph
node metastasis and the expression of VEGF-C, VEGF-D and VEGFR-3 in
T1 lung adenocarcinoma. Anticancer Res. 27:3735–3741.
2007.PubMed/NCBI
|
|
40
|
Saintigny P, Kambouchner M, Ly M, Gomes N,
Sainte-Catherine O, Vassy R, Czernichow S, Letoumelin P, Breau JL,
Bernaudin JF, et al: Vascular endothelial growth factor-C and its
receptor VEGFR-3 in non-small-cell lung cancer: Concurrent
expression in cancer cells from primary tumour and metastatic lymph
node. Lung Cancer. 58:205–213. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Pitkin L, Luangdilok S, Corbishley C,
Wilson POG, Dalton P, Bray D, Mady S, Williamson P, Odutoye T, Rhys
Evans P, et al: Expression of CC chemokine receptor 7 in tonsillar
cancer predicts cervical nodal metastasis, systemic relapse and
survival. Br J Cancer. 97:670–677. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bender RJ and Mac Gabhann F: Dysregulation
of the vascular endothelial growth factor and semaphorin
ligand-receptor families in prostate cancer metastasis. BMC Syst
Biol. 9:552015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Song X, Zhang W, Zhang Y, Zhang H, Fu Z,
Ye J, Liu L, Song X and Wu Y: Expression of semaphorin 3A and
neuropilin 1 with clinicopathological features and survival in
human tongue cancer. Med Oral Patol Oral Cir Bucal. 17:e962–e968.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Cagnoni G and Tamagnone L: Semaphorin
receptors meet receptor tyrosine kinases on the way of tumor
progression. Oncogene. 33:4795–4802. 2014. View Article : Google Scholar
|
|
45
|
Tamagnone L and Rehman M: To die or not to
die: Sema3E rules the game. Cancer Cell. 24:564–566. 2013.
View Article : Google Scholar : PubMed/NCBI
|