Introduction
Asthma is a chronic airway disease that is
characterized by significantly exacerbated bronchospasms and marked
inflammation of the airways. Episodic airway obstruction and airway
inflammation are two features of bronchial asthma (1). While the exact etiology of asthma
remains unknown, it is involved in possible genetic predispositions
coupled with an exposure to ‘inflammatory triggers’ and
‘bronchospastic triggers’ (2).
Based on clinical manifestations, the principles of pharmacotherapy
are mainly centered on the reversal or prevention of bronchial
smooth muscle constriction and the reversal or prevention of airway
inflammation following asthmatic seizures. β-adrenergic receptor
agonists are key drugs in the management of asthma as they relax
the bronchial smooth muscles (3).
Previously, a highly-selective β2-agonist with a high
liposolubility, active over a longer period of time and with fewer
adverse reactions was identified, and is a potential option for the
treatment of bronchial asthma (4).
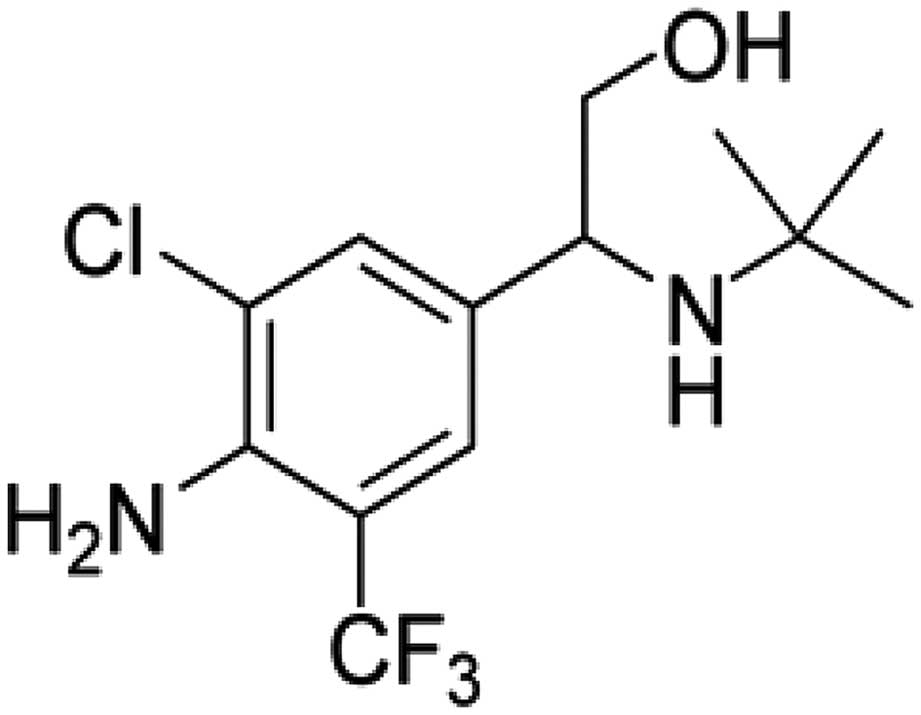
2-(4-Amino-3-chloro-5-trifluomethyl-phenyl)-2-tert-butyl-
amino-ethanol hydrochloride (SPFF) is a novel compound derived from
the traditional β2-agonist that, to the best of our
knowledge, was first developed by the Shenyang Pharmaceutical
University (Shenyang, Liaoning, China) (5). It is a racemic mixture of equal
amounts of (−)SPFF and (+)SPFF due to the chiral carbon atom in its
chemical structure. Previously, it was shown that SPFF was able to
relax isolated tracheal smooth muscles (5). The aim of the present study was
therefore to compare and contrast the relaxant effect on the
airways in vivo and the inhibition on allergy mediator
release by the various isomers of SPFF. The findings of this study
may also provide a theoretical and experimental basis for further
development of novel drugs for asthmatic pulmonary function.
Materials and methods
Chemicals and drugs
(−)SPFF, (±)SPFF, (+)SPFF and mabuterol (MAB) were
supplied by the Pharmaceutical Engineering Department, Shenyang
Pharmaceutical University (enantiomeric excess, >99%). The
chemical structure of SPFF is shown in Fig. 1. Isoprenaline chloride was purchased
from Shanghai Harvest Pharmaceutical Co., Ltd (Shanghai, China).
Pentobarbital sodium and histamine phosphate were purchased from
Sinopharm Chemical Reagent Co., Ltd. (Shanghai, China). Propranolol
hydrochloride was obtained from the Northeast Pharmaceutical Group
Co., Ltd. (Shenhe, Shenyang, China), ovalbumin (OVA) was provided
by Sigma-Aldrich (Hong Kong, China) and the adsorbed diphtheria,
tetanus and acellular pertussis combined vaccine were provided by
the Chengdu Institute of Biological Products (Chengdu, Sichuan,
China).
Animals
Dunkin-Hartley male guinea pigs, weighing 300±50 g,
and Wistar male rats, weighing 150±30 g, were provided by the
Experimental Animal Centre, Shenyang Pharmaceutical University.
Animals were housed in a room at a temperature of 21–23°C, a
relative humidity of 30–70% and a 12-h light/dark cycle with free
access to food and water. All experimental procedures carried out
in the study were performed in accordance with the Guidelines for
the Care and Use of Laboratory Animals of Shenyang Pharmaceutical
University.
Konzett and Rössler experiment in
anesthetized guinea pigs
The animals were randomly divided into 11 groups
(n=6 per group) and anesthetized with pentobarbital [30 mg/kg,
intraperitoneal injection (i.p.)]. Body temperature was maintained
at 36–37°C with a heating pad and the Konzett and Rössler
experiment was performed with slight modifications to an
established method (6). Briefly,
the trachea was cannulated and ventilated 60 times/min with a tidal
air volume of 8 ml/kg using a respirator. The histamine-induced
bronchoconstriction was measured using a flow transducer and
recorded by a biosignal recording system. Histamine (20 μg/kg) was
administered intravenously 30, 60, 90, 120, 150, 180, 210 and 240
min after the intraduodenal administration of the test drugs.
Histamine-induced bronchoconstriction prior to the administration
of normal saline (N.S.) or the tested drugs was established as 100%
and the inhibition rate of each bronchodilator was calculated at
various time points.
Effect on allergic mediator (histamine)
release following an allergen challenge in rats
Wistar rats (n=24) were sensitized by i.p. of 0.5 ml
10% OVA emulsified in 10 mg aluminum hydroxide gel in a total
volume of 100 μl in N.S., according to the method described by
Kucharewicz et al (7) with
slight modifications. Two weeks later, the animals were sacrificed
by cervical dislocation and the lung tissues were removed and
divided into small samples. The tissues were incubated for 5 min in
37°C homothermal water. The tested drugs, in the absence and
presence of propranolol (10−5 M), were added and
incubated for another 5 min, and subsequently 2 mg/kg OVA was
added. The production of the allergic mediator (histamine) was
detected 10 min later in each sample of isolated ileum from the
guinea pigs by observing the change in tension of the ileum.
Determination of cyclic adenosine
monophosphate (cAMP) levels in the lungs of OVA-sensitized
rats
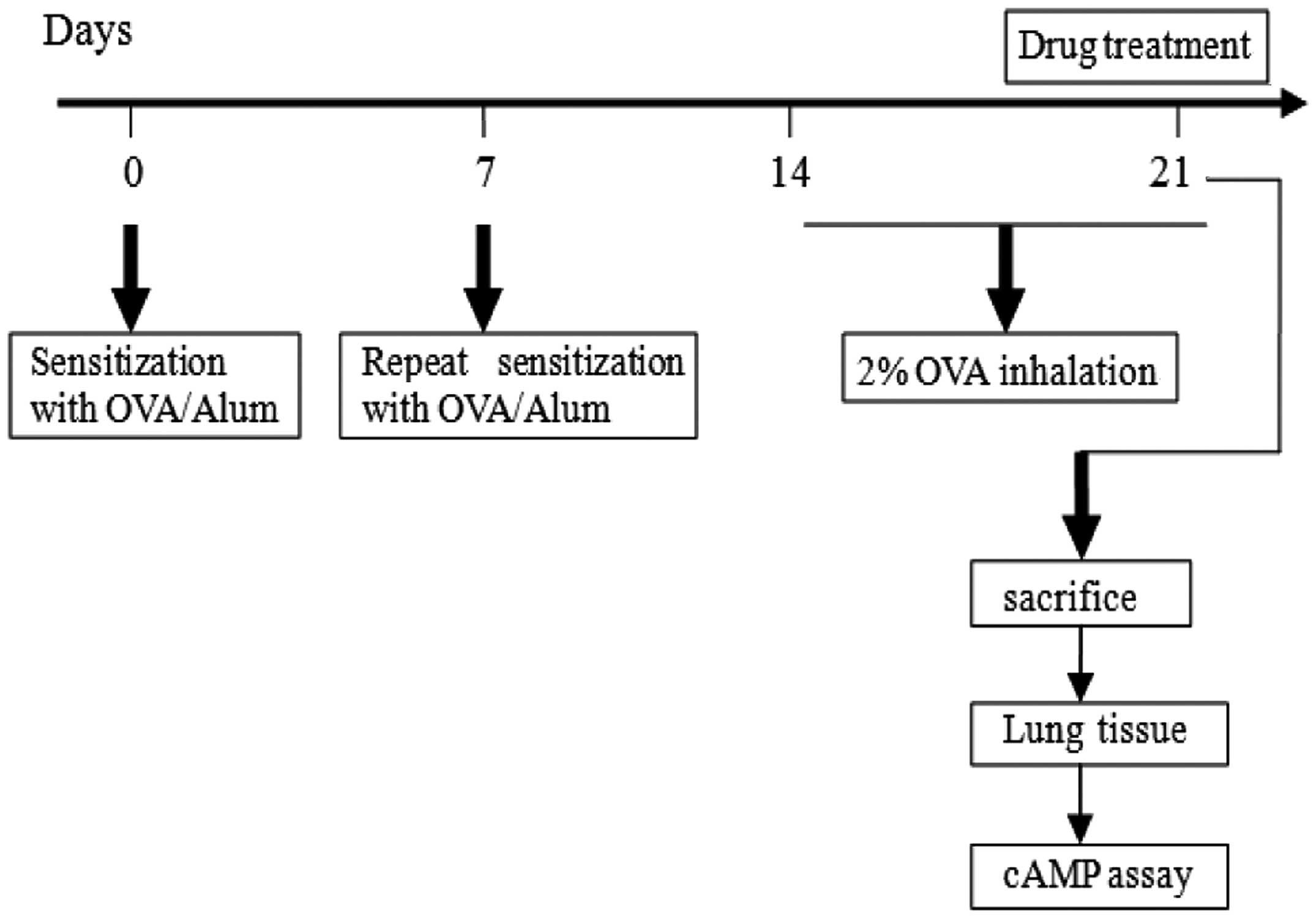
Wistar rats were randomly divided into 12 groups
(n=8). Suspensions of 100 mg OVA/600 mg of aluminum hydroxide in 1
ml N.S. were prepared. OVA-treated rats were sensitized by
subcutaneous injection with 0.5 ml of the suspension and were also
provided 0.5 ml of the same suspension by i.p. with the addition of
the deactivated pertussis bacillus vaccine (5×109
colony-forming units) on days 0 and 7. Non-sensitized rats received
aluminum hydroxide in N.S. From day 14, the animals were challenged
with aerosolized OVA (2% in N.S.) for 20 min a day over one week
(8,9), and 30 min prior to the last OVA
challenge (−)SPFF, (±)SPFF and (+)SPFF at 0.1, 0.25 and 0.5 mg/kg
dissolved in 0.7% sodium carboxymethyl cellulose (CMC-Na) was
administered intragastrically (i.g.), respectively, to rats in the
drug-treated groups. MAB (0.1 mg/kg) was i.g. administered as the
positive-drug control, while 0.7% CMC-Na was the vehicle. The
animals were sacrificed following the last challenge and the lungs
were removed. The cAMP levels in the tissues were determined using
a commercial ELISA kit (Fengxiang Biotechnology Co., Ltd, Shanghai,
China). The experimental regime is shown in Fig. 2.
β1/β2
selectivity
Guinea pigs (n=8) were sacrificed by cervical
dislocation. The hearts were rapidly excised and the right atria
were dissected and mounted in an organ bath containing Tyrode’s
solution, which was gassed with 95% O2 and 5%
CO2. The contractions of the spontaneously beating right
atria were measured according to the method described by Ko et
al (10), which was slightly
modified. Subsequent to the baseline contraction of the
spontaneously beating right atria becoming stable, the contractile
tension was assessed in response to the cumulative addition of
(−)SPFF, (±)SPFF and (+)SPFF in final concentrations ranging from
10−7-3×10−4 M, or isoprenaline
(10−9-3×10−6 M).
Statistical analysis
Data were calculated as mean ± standard error of
mean (S.E.M.) and analyzed by one-way analysis of variance (ANOVA)
on SPSS 16.0. The statistical evaluation among the groups was
determined by LSD test if variance is homogeneity or by Dunnett’s
T3 test if variance is heterogeneity. The differences were
considered significantly at p<0.05.
Results
Effect of drug treatment on
histamine-induced bronchoconstriction in guinea pigs
As shown in Fig. 3,
MAB as a reference and (−)SPFF and (±)SPFF could suppress the
increase of histamine-induced bronchoconstriction. MAB caused a
statistically significant reduction of the histamine-induced
bronchoconstriction 60 min after administration and the effect
remained until 240 min. The lowest dose (10 μg/kg) of (−)SPFF
caused no statistically significant change (Fig. 3A), however, at doses of 30 and 100
μg/kg it caused a statistically significant suppression 30 min
after administration, but the effect at 30 μg/kg was rapidly
decreased after 180 min. The highest dose (100 μg/kg) of (−)SPFF
had the most efficient pharmacological effect and its effect was
still observed at 240 min. (±)SPFF was less efficient than (−)SPFF,
and doses of 100 and 300 μg/kg exhibited effects at 90 min but only
for a short duration (Fig. 3B).
(+)SPFF presented no significant effects (Fig. 3C).
Effect of drug treatment on allergic
mediator (histamine) release from the lung tissues in the asthma
rats
As shown in Fig. 4,
isoprenaline (1 μM) as a reference inhibited histamine release in
the lungs of OVA-sensitized/challenged rats. However, the
suppressive effect was evidently blocked with the addition of
propranolol, a β-receptor antagonist. (±)SPFF (0.01, 0.1 and 1 μM)
also produced a significant decrease in total histamine release and
the inhibition rates were 53.75, 58.86 and 79.77%, respectively
(Fig. 4A). The inhibition rates of
(+)SPFF (0.1 and 1 μM) were 69.94 and 71.52% (Fig. 4C) and for (−)SPFF (1 μM) the rate
was 69.64% (Fig. 4B). Pretreatment
with propranolol prevented the inhibitory effects of SPFF and its
enantiomers, which is consistent with β2 blockade,
suggesting that the mechanism is relevant to the β-receptor.
Effects of drug treatment on the cAMP
levels in the lung tissues of the asthma rats
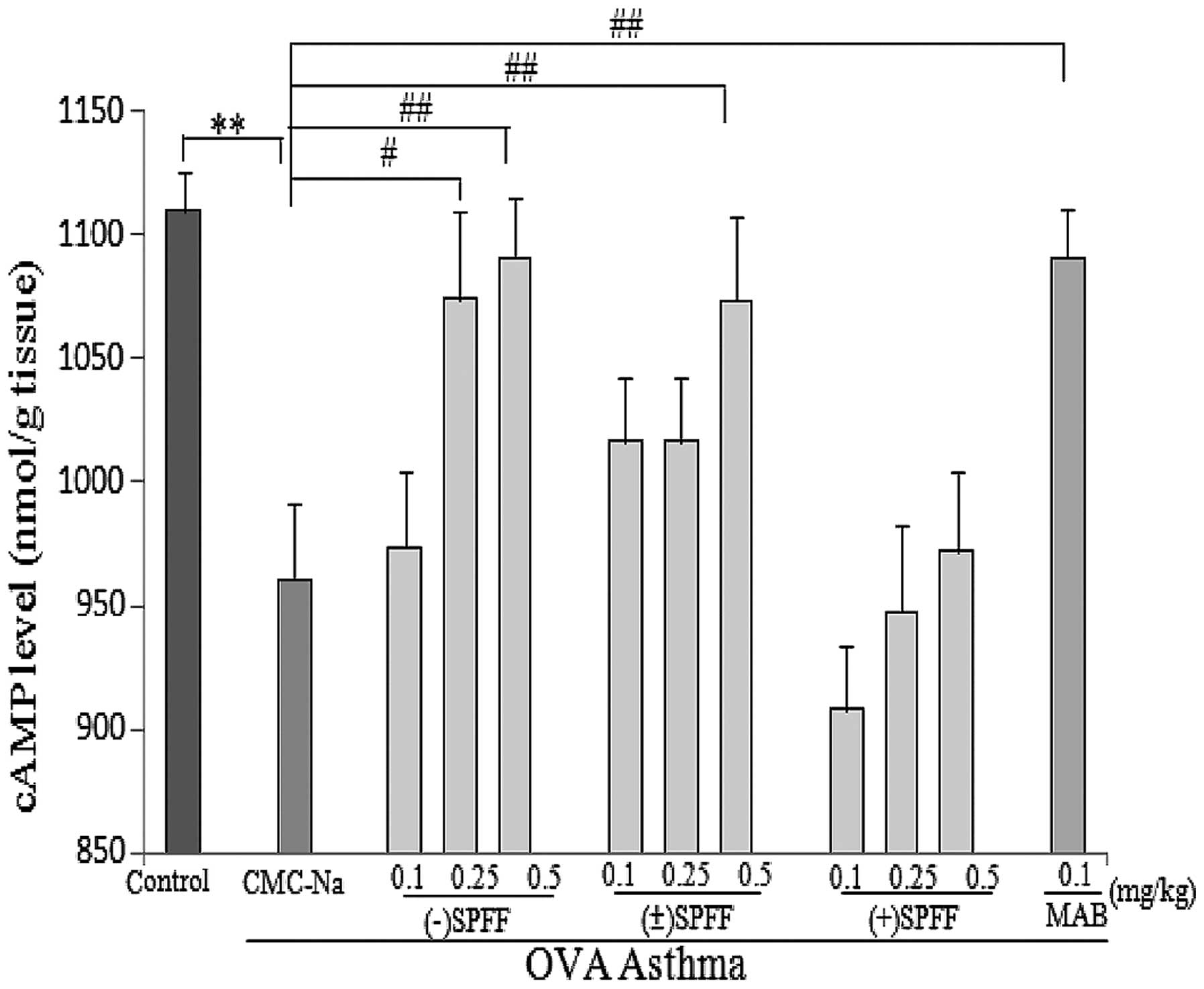
The effect of drug treatment on the cAMP levels is
shown in Fig. 5. The cAMP levels in
the lung tissues were found to be significantly reduced in
OVA-sensitized/challenged rats (0.7% CMC-Na group) compared with
the control (Fig. 5), which showed
that the asthma model had been successfully established. The
reference drug, MAB, clearly enhanced the level of cAMP (P<0.01)
and treatment with (±)SPFF and (−)SPFF also showed dose-dependent
beneficial effects. In addition, treatment with (−)SPFF (0.25 and
0.5 mg/kg) and (±)SPFF (0.5 mg/kg) resulted in a significant
increment of the cAMP content compared with the 0.7%CMC-Na group.
However, (+)SPFF showed no effects at all the tested doses
(Fig. 5).
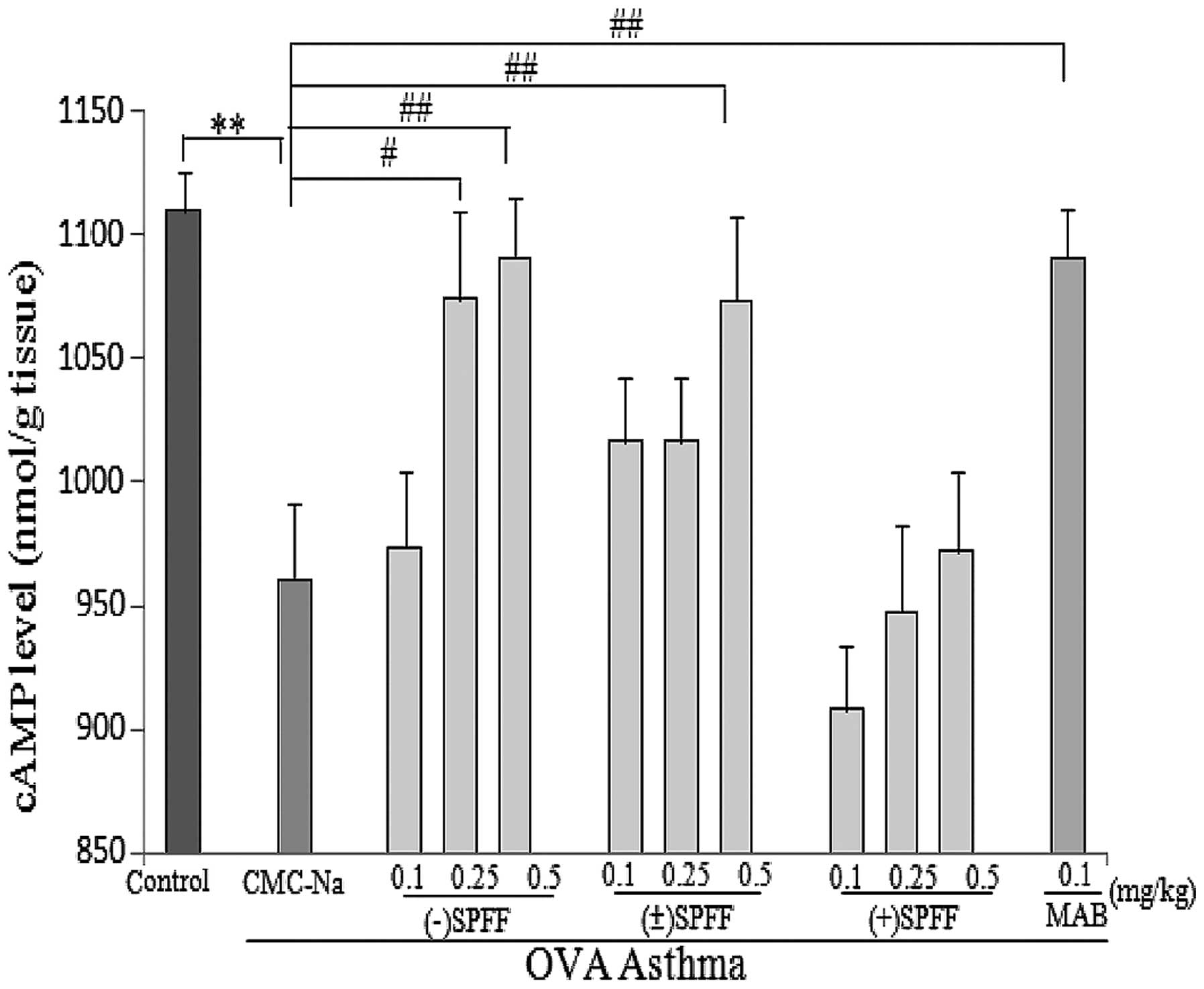 | Figure 5Effect of (±)SPFF, (−)SPFF, (+)SPFF
and mabuterol on the level of cAMP in the lungs of rats (n=8; mean
± SEM). **P<0.01 compared with normal saline;
#P<0.05 and ##P<0.01 compared with the
OVA-asthma model by ANOVA followed LSD on SPSS 16.0. cAMP, cyclic
adenosine monophosphate; CMC-Na, sodium carboxy methylcellulose;
SPFF,
2-(4-amino-3-chloro-5-trifluomethyl-phenyl)-2-tert-butylamino-ethanol
hydrochloride; MAB, mabuterol; SEM, standard error of the mean;
OVA, ovalbumin; ANOVA, analysis of variance; LSD, least significant
difference. |
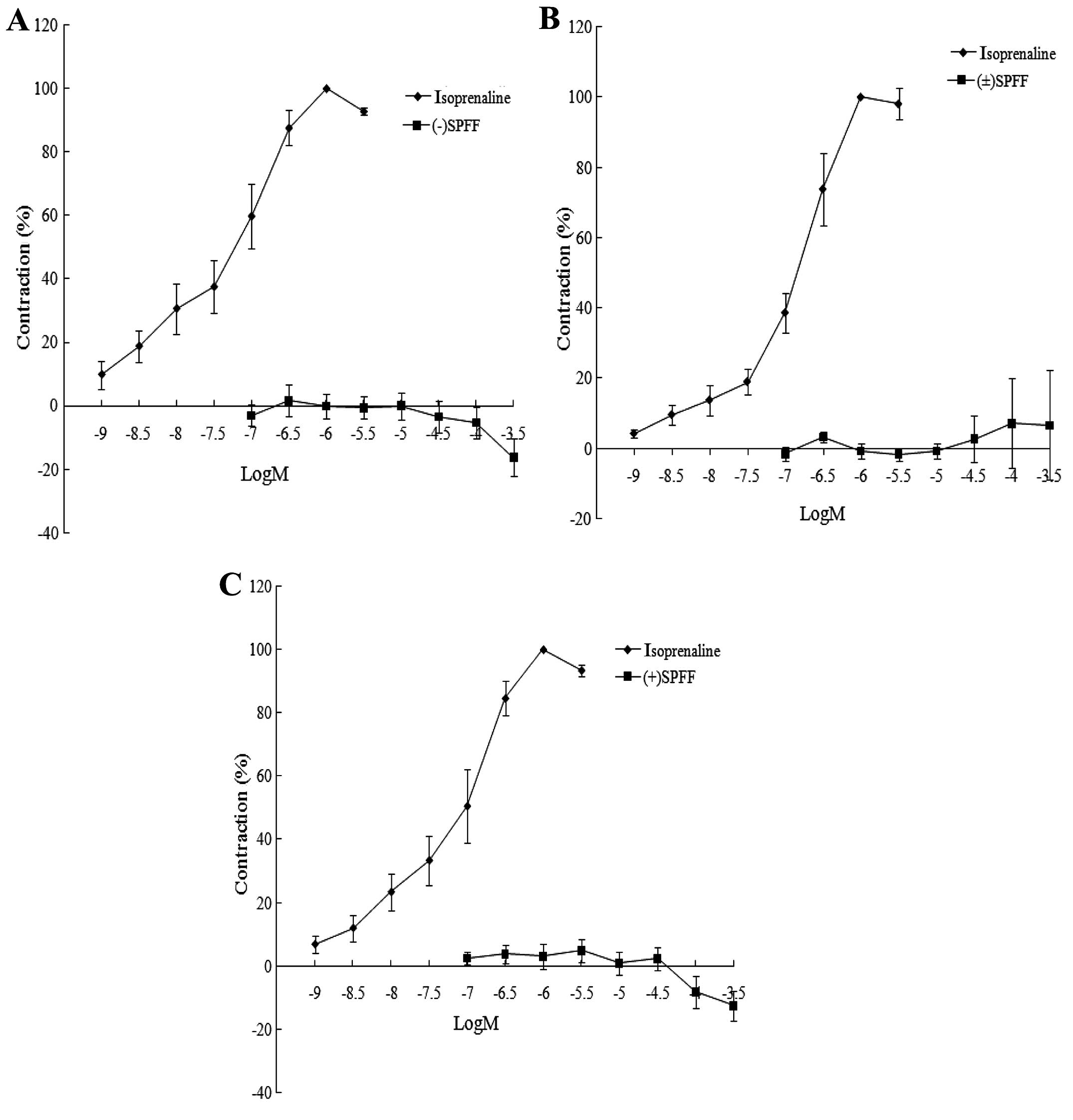
No effect of drug treatment on the
contration of isolated guinea pig atria
As shown in Fig. 6,
isoprenaline (10−9-3×10−6 M) induced an
increase in the cardiac contractility in vitro, while
(±)SPFF, (−)SPFF and (+)SPFF did not show any positive inotropic
action on the isolated guinea pig right atria. This result
indicated that in addition to their relaxant effects on the small
airway and release of allergic mediators, the tested drugs did not
enhance cardiac contractility and thus they may have an improved
selectivity for the β2-receptor compared with
isoprenaline.
Discussion
It has been confirmed in the present study that SPFF
and its optical isomers reduced the resistance in the airways of
guinea pigs, but there were differences in the intensity and
duration of action. Compared with the other tested drugs, the high
dose of (−)SPFF (100 mg/kg) almost achieved the same inhibitory
effect as the reference drug, MAB, and also extend the duration of
action until 4 h. (±)SPFF at approximately 3-fold higher doses than
(−)SPFF showed less potency as the effect began 90 min after
intraduodenal administration and its active duration was maintained
for a short time. (+)SPFF did not show any significant dilation of
the airways until the dose administered was 10-fold higher than the
dose of (−)SPFF used. It is generally accepted that relaxant
effects of (−)-enantiomeric β2 agonists, including
salbutamol or terbutaline, were greater than the (+)-enantiomeric
one, which is presumed to be highly associated with the strong
affinity of the (−)-enantiomer to the β2-receptor
(11). Henderson et al
(12) found that in a mouse asthma
model sensitized/challenged by OVA, obvious differences in the
pharmacodynamics between the (S)- and (R)-enantiomers of albuterol
were evident. The enantiomers inhibited the inflammation reactions,
including reducing airways eosinophil infiltration, goblet cell
hyperplasis and mucus occlusion, but the efficacy of the
(R)-enantiomer was greater compared with the (S)-enantiomer. In
addition, (S)-albuterol increased airways edema and reactivity in
the mice, while (R)-albuterol had no effect. A possible reason for
this may be attributed to the higher affinity of (S)-albuterol to
the β2-receptor, compared with (R)-albuterol. The
(R)-enantiomer of albuterol bound to the β2-receptor
with an affinity of almost 100-fold greater than that of the
(S)-enantiomer (9).
Mast cells play an important role in the
pathogenesis of asthma. In the fast phase of asthma, specific
immunoglobulin E can induce the degranulation of mast cells, which
results in the release of histamine and other allergic mediators
and eventually induces airway smooth muscle (ASM) contraction. In
addition, mast cells also release a variety of other cytokines and
inflammation factors, which mediate chronic airways inflammation.
Stabilizing the mast cell membranes should be one of the important
antasthmatic strategies (13). In
the fast phase, β2 agonists exerted inhibitory effects
on the mediators released from mast cells and the degranulation of
the cells (14). Previously, it was
shown that the inhibitory effects were associated with the affinity
to the β2-receptor (15). Formoterol was demonstrated to have a
more efficient effect on stabilizing the mast cell membranes than
salmeterol as it had a higher affinity to the receptor (15). In the present study, the role of
SPFF and its enantiomers in stabilizing mast cells was investigated
by determination of the release of inflammatory mediators from the
lungs of allergic rats. The results showed that all the tested
drugs were capable of inhibiting the release. Among them, (±)SPFF
showed the most efficient activity, and the potency of (−)SPFF and
(+)SPFF was almost identical. When propranolol was added to block
the β2-receptors, the effects of SPFF and its
enantiomers were all blocked, indicating that the compounds can
bind exactly to the β2-receptors, however, the
β2-adrenergic receptor blockade showed the greatest
tendency when propranolol was incubated with (−)SPFF. This
indicated that (−)SPFF may be the compound that had the strongest
affinity to the β2-receptors among the three drugs
tested. However, more data are required to confirm this
hypothesis.
β2-receptor agonists can induce the
relaxation of ASM by coupling with β2-receptors, which
is the major antasthmatic mechanism pathway of these drugs. The
β2-adrenergic receptor is a member of the
G-protein-coupled receptors. It can stimulate adenylyl cyclase and
subsequently generate an important regulatory second messenger,
cAMP. In turn, increased levels of cAMP can stimulate
cAMP-dependent protein kinase A. Calcium extrusion and
sequestration is then induced and thus results in smooth muscle
relaxation (16,17). Therefore, the mechanism of drug
action can be preliminarily understood by detecting the influence
of the tested drugs on the cAMP content, and determining the
intensity of the airway expansion from a deeper lever. The results
demonstrated that both (±)SPFF and (−)SPFF can dose-dependently
increase the cAMP content in the lung tissue. In addition, the cAMP
levels in the lungs following (±) SPFF (0.25 and 0.5 mg/kg) and
(−)SPFF (0.5 mg/kg) treatment were significantly enhanced compared
with the negative vehicle rats. It is postulated that the tested
drugs can significantly relax the airways and have a high enough
intrinsic activity. As mentioned previously, the (+)enantiomer did
not have an effect through β2-receptor activation
(9), and it was also demonstrated
that none of the (+)SPFF doses can increase the cAMP content,
indicating that the compound has no association with this pathway
and its therapeutic effect on asthma may occur through other
pathways.
Atria contractility of guinea pigs was determined to
evaluate the subtype receptor selectivity of the compounds. It is
well known that the β-receptors are mainly divided into
β1, β2 and β3 subtypes. Certain
drugs acting on the β2 receptor may also bind to
β1 receptor due to their poor selectivity. This may
result in enhanced myocardial contractility and other cardiac
side-effects when used for treating asthma (18). A good β2-receptor agonist
should have a high selectivity to the β2-receptor and
cause less cardiac side-effects, similar to formoterol and
salmeterol. Fromoterol is reported to have a
β2:β1 adrenoceptor selectivity ratio of
between 200 and 400, while salmeterol is >10,000 (19). Data from the current study have
shown that the three drugs, (±)SPFF, (−)SPFF and (+)SPFF, had no
significant effects on isolated guinea pig cardiac contractility,
indicating that they may have a good selectivity to the
β2 subtypes.
(−)SPFF and (±)SPFF significantly inhibited the
increase of the histamine-induced lung outflow of the guinea pigs,
whereas (+)SPFF did not show a similar effect. (−)SPFF, (±)SPFF and
(+)SPFF inhibited the release of allergic mediators in lung tissues
of OVA-sensitized/challenged rats, possibly by stabilizing the mast
cell membrane. Among the tested compounds, (±)SPFF showed the
greatest efficacy. The cAMP assay showed that the therapeutic
effect of (±)SPFF and (−)SPFF were associated with an increase in
cAMP levels, but (+)SPFF did not show any effect. None of the
compounds had any significant effect on isolated guinea pig cardiac
contractility. Concerning the pharmacodynamic properties and
mechanism, (−)SPFF was more efficient than (+)SPFF. However, for
the receptor selectivity there was no significant difference
between (−)SPFF and (+)SPFF.
Acknowledgements
The present study was a Grants-in-Aid for Scientific
Research (2009ZX09102-018) from the National Ministry of Science
and Technology.
References
|
1
|
Henderson WR Jr, Chiang GK, Tien YT and
Chi EY: Reversal of allergen-induced airway remodeling by CysLT1
receptor blockade. Am J Respir Crit Care Med. 173:718–728. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jung WK, Lee DY, Choi YH, Yea SS, Choi I,
Park SG, Seo SK, Lee SW, Lee CM, Kim SK, Jeon YJ and Choi IW:
Caffeic acid phenethyl ester attenuates allergic airway
inflammation and hyperresponsiveness in murine model of
ovalbumin-induced asthma. Life Sci. 82:797–805. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cazzola M and Matera MG: Novel long-acting
bronchodilators for COPD and asthma. Br J Pharmacol. 155:291–299.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zdanowicz MM: Pharmacotherapy of asthma.
Am J Pharm Educ. 71:982007. View
Article : Google Scholar
|
|
5
|
Gan LL, Wang MW, Cheng MS and Pan L:
Trachea relaxing effects and beta2-selectivity of SPFF, a newly
developed bronchodilating agent, in guinea pigs and rabbits. Biol
Pharm Bull. 26:323–328. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tjesi -Drinkovi D, Stambuk N,
Tjesi-Drinkovi D, Konjevoda P, Gotovac N, Curkovi T and Votava-Rai
A: Met-enkephalin effects on histamine-induced bronchoconstriction
in guinea pigs. Coll Antropol. 29:689–692. 2005.PubMed/NCBI
|
|
7
|
Kucharewicz I, Kasacka I, Pawlak D,
Tankiewicz-Kwedlo A, Mroczko B, Buczko W and Bodzenta-Lukaszyk A:
The concentration of kynurenine in rat model of asthma. Folia
Histochem Cytobiol. 46:199–203. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Onoue S, Sato H, Ogawa K, Kojo Y, Aoki Y,
Kawabata Y, Wada K, Mizumoto T and Yamada S: Inhalable dry-emulsion
formulation of cyclosporine A with improved anti-inflammatory
effects in experimental asthma/COPD-model rats. Eur J Pharm
Biopharm. 80:54–60. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen YH, Wu R, Geng B, Qi YF, Wang PP, Yao
WZ and Tang CS: Endogenous hydrogen sulfide reduces airway
inflammation and remodeling in a rat model of asthma. Cytokine.
45:117–123. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ko WC, Shih CM, Chen MC, Lai YH, Chen JH,
Chen CM and Lin CN: Suppressive effects of 3-O-methylquercetin on
ovalbumin-induced airway hyperresponsiveness. Planta Med.
70:1123–1127. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Waldeck B: Enantiomers of bronchodilating
beta2-adrenoceptor agonists: is there a cause for concern? J
Allergy Clin Immunol. 103:742–748. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Henderson WR Jr, Banerjee ER and Chi EY:
Differential effects of (S)- and (R)-enantiomers of albuterol in a
mouse asthma model. J Allergy Clin Immunol. 116:332–340. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Boyce JA, Broide D, Matsumoto K and
Bochner BS: Advances in mechanisms of asthma, allergy, and
immunology in 2008. J Allergy Clin Immunol. 123:569–574. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hanania NA and Moore RH: Anti-inflammatory
activities of beta2- agonists. Curr Drug Targets Inflamm Allergy.
3:271–277. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Scola AM, Chong LK, Suvarna SK,
Chess-Williams R and Peachell PT: Desensitisation of mast cell
beta2-adrenoceptor-mediated responses by salmeterol and formoterol.
Br J Pharmacol. 141:163–171. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Trian T, Burgess JK, Niimi K, Moir LM, Ge
Q, Berger P, Liggett SB, Black JL and Oliver BG: β2-Agonist induced
cAMP is decreased in asthmatic airway smooth muscle due to
increased PDE4D. PLoS One. 6:e200002011.
|
|
17
|
Moon HG, Kim YS, Choi JP, Choi DS, Yoon
CM, Jeon SG, Gho YS and Kim YK: Aspirin attenuates the
anti-inflammatory effects of theophylline via inhibition of cAMP
production in mice with non-eosinophilic asthma. Exp Mol Med.
42:47–60. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Baker JG: The selectivity of
beta-adrenoceptor agonists at human beta1-, beta2- and
beta3-adrenoceptors. Br J Pharmacol. 160:1048–1061. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ryall JG, Sillence MN and Lynch GS:
Systemic administration of beta2-adrenoceptor agonists, formoterol
and salmeterol, elicit skeletal muscle hypertrophy in rats at
micromolar doses. Br J Pharmacol. 147:587–595. 2006. View Article : Google Scholar : PubMed/NCBI
|